24 December 2020: Articles 
Celiac Disease in an Adult Presenting as Behavioral Disturbances
Rare coexistence of disease or pathology
Andrew K. Murphy1ACEF, Joseph A. Norton1AEF, Benjamin R. Pflederer12AEG*DOI: 10.12659/AJCR.928337
Am J Case Rep 2020; 21:e928337
Abstract
BACKGROUND: Celiac disease is very common, with some estimates placing the prevalence at approximately 1: 300 worldwide. Typified by autoimmune degradation of the duodenal brush border due to reactivity with dietary gluten, causing malabsorption, it classically presents with both gastrointestinal and extra-intestinal symptoms. Gastrointestinal symptoms commonly include diarrhea, constipation, foul steatorrhea, flatulence, and bloating. With increased awareness and availability of testing, it is rare that a patient would present with celiac crisis, which is a syndrome of profuse diarrhea and severe metabolic/nutritional disturbances. In children, interestingly, celiac disease can present primarily as behavioral disturbance, such as increased aggression or anxiety, with milder or absent gastrointestinal symptoms.
CASE REPORT: A 25-year-old man with a history of schizophrenia and autism spectrum disorder presented for behavioral disturbance after breaking into a neighbor’s house to eat food. He also reported several months of diarrhea and fecal incontinence and was noted to have severe malnutrition on exam, despite dramatic food intake. Tissue transglutaminase IgA antibody (TTG) and gliadin IgA were highly suggestive of celiac disease, which was confirmed by biopsy. He was started on a lactose-free and gluten-free diet, and required a short course of total parenteral nutrition (TPN) for nutritional resuscitation. He improved rapidly with this intervention, and returned to nutritional and behavioral baseline.
CONCLUSIONS: We report a unique case in which an adult with psychiatric comorbidities presented with predominantly behavioral disturbances, a more common presentation in children with the disorder. These patients may present in an atypical fashion, and the clinician should have a high index of suspicion.
Keywords: Autistic Disorder, Behavioral Symptoms, celiac disease, Autism Spectrum Disorder, Child, Diet, Gluten-Free, Duodenum, Glutens
Background
Celiac disease is a very common disease process, with some estimates placing the prevalence at approximately 1: 300 worldwide [1]. This disease is typified by autoimmune degradation of the duodenal brush border due to reactivity with dietary gluten, causing malabsorption [2]. In adults, it classically presents with both gastrointestinal and extra-intestinal symptoms. Gastrointestinal symptoms commonly include diarrhea, constipation, foul steatorrhea, flatulence, and bloating [3], but these may vary, with approximately 4% of patients presenting with constipation or dyspepsia instead of the classic diarrhea [4]. Extra-intestinal symptoms are often anemia, vitamin D deficiency, bone mineral deficiencies, dermatitis herpetiformis, or, rarely, neuropsychiatric symptoms such as headache or depression [4,5]. The presentation of celiac disease in children can vary dramatically from that of adults. Notably, it can present primarily as behavioral disturbance, such as increased aggression or anxiety, with milder or absent gastrointestinal symptoms [6]. Indeed, more patients with extra-intestinal, atypical, or mild presentations are being detected as awareness of the disease increases and serologic testing allows for easy testing [7]. Thus, it is now rare that a patient would present with a celiac crisis, which is a syndrome of profuse diarrhea and severe metabolic/nutritional disturbances [8]. This presentation has become increasingly uncommon as testing has become easier, and has been almost completely confined to a diagnosis in children [8]. Although recent evidence suggests not all patients require a biopsy for diagnosis, it remains the criterion standard, showing villous atrophy, intraepithelial lymphocytosis, and crypt hyperplasia [9,10]. These 3 pathologic findings have been standardized through the Marsh classification [9]. Our case highlights the fact that celiac disease may also present primarily as behavioral disturbance in adults, particularly if underlying psychiatric disease or intellectual deficits are present.
Case Report
A 25-year-old man with a past medical history of autism spectrum disorder and schizophrenia presented with 1–2 months of vomiting and diarrhea, with weight loss of 14–18 kg over 12 months. Five months prior to admission, however, he had reported having mild abdominal pain and severe behavioral disorders, which were a departure from his baseline. His guardian described aggressive behaviors and fights with family, which worsened before the diarrhea was prominent. The patient’s guardian also noted that his abdomen had started to protrude and his legs were swollen. The patient was eating constantly due to unremitting hunger, which was a change from his normal baseline. In fact, his parents had to place locks on the cabinets and refrigerator to mitigate his eating. He later developed diarrhea that was so severe he was frequently in-continent. In the 2 months prior to admission, the patient was evaluated by Gastroenterology, Nephrology, his primary care provider (PCP), and another facility’s Emergency Department, without a definitive diagnosis. The patient became significantly weaker, and his extreme hunger led to him breaking into his neighbor’s house for food, which prompted his mother to bring him to the Emergency Department.
The patient had been followed by a psychiatrist and diagnosed with autism spectrum disorder, episodic mood disorder, and psychosis of unspecified type. He was taking lamotrigine, lithium carbonate, risperidone, and topiramate.
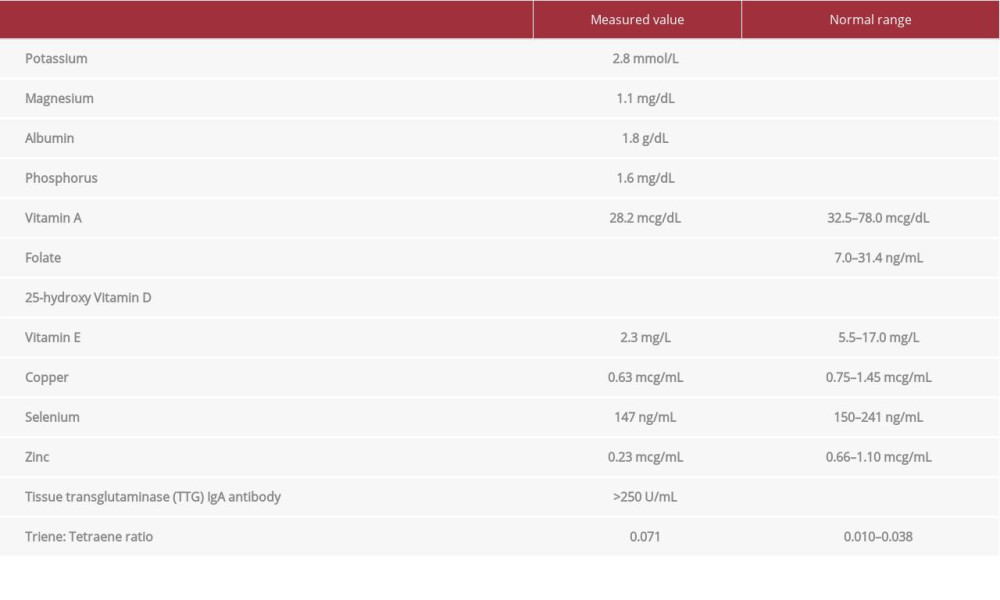
On exam, evidence of malnutrition with bitemporal wasting, abdominal distention, diffuse anasarca, and 4+ bilateral lower-extremity pitting edema was noted. Laboratory investigations revealed significant metabolic derangements and nutritional deficiencies (Table 1). A computed tomography (CT) abdomen and pelvis was performed, demonstrating small-bowel enteritis. The patient had no travel history or exposure risk to suggest an infectious etiology. A stool sample was collected for culture, ova, and parasite examination, white blood cell lactoferrin, and
After initiation of TPN, potassium, magnesium, and phosphorus levels were monitored closely, with appropriate repletion to prevent onset of re-feeding syndrome.
After initiation of a gluten-free, lactose-free diet and 10 days of TPN, the patient was discharged with significant improvement in symptoms, including near-total resolution of his anasarca. Two days following admission, the patient presented to the Emergency Department following partial traumatic removal of his Groshong catheter. After re-evaluation, it was deemed that he had sufficiently recovered after 12 days total of TPN, and the Groshong catheter was removed.
Discussion
Celiac disease resulting in electrolyte and metabolic derangements in adults has previously been described. These case reports describe a shorter time course and were often associated with an inciting event, such as infection or surgery [8,11–13]. In the present report, we describe a patient who showed signs and symptoms on a time frame of months to a year, with weight loss and diarrhea that progressed to peripheral edema and, ultimately, weakness. His diagnosis was obfuscated by his baseline function in the setting of autism spectrum disorder and episodic mood disorder, masking gastrointestinal symptoms and likely impairing his ability to adequately describe symptoms that he was experiencing. As a result, his diagnosis was delayed despite visits with several providers of varying specialties.
A similar presentation has been noted in a patient with Down syndrome [14]. In this opinion paper published in JAMA, Khorana and Khorana share the story of their son, a young man with Down syndrome who presented with stark behavioral changes and outbursts that were similar to those in our patient. He also had significant gastrointestinal symptoms, but these were masked by the behavioral issues. Like our patient, he was treated with several behavioral medications. Some of these, including lamotrigine, can have gastrointestinal adverse effects in a significant proportion of patients [15], further confounding the diagnostic assessment. His eventual diagnosis of celiac disease, which resulted in appropriate treatment and resolution of behavioral symptoms, came about through the clinical suspicion of a physician who was attuned to the interaction of these symptoms in a person with Down syndrome.
In the pediatric literature, Taddeucci and colleagues reported several cases of celiac disease presenting primarily with neuropsychological disorders [16]. They recommended screening for celiac disease in children presenting with disorders including “behavioral disorders and some psychiatric troubles.”
Over the past decade there has been significant interest in the association, if any, between psychiatric disorders and celiac disease. This is outlined in Slim and colleagues’ helpful 2014 review [17]. Their comprehensive literature review of this issue in children and adults included such disorders as depression, schizophrenia, autistic disorders, and ADHD. Their assessment was that their review “revealed the existence of an association between CD (celiac disease) and other gluten-related disorders with psychiatric disorders across different age groups.” They suggest that “gastroenterologists and other healthcare professionals involved in the management of patients with CD should be aware of the increased risk of psychiatric disorders in these patients.” They also note that the interaction between psychiatric symptoms and GI pathology may well be bidirectional.
Returning to our case in light of this literature, we see a patient with psychiatric disease who also developed severe celiac disease and presented in nutritional crisis and exacerbation of psychiatric symptoms. Similar to other reports, this interaction led to delayed diagnosis. Given the disparity in time between onset of symptoms and diagnosis, the patient had a prolonged exposure to dietary gluten. This results in profound degradation via gluten-bound HLA-DQ2 and HLA-DQ8 molecules propagating a T-cell-mediated inflammatory response [2]. The prolonged inflammatory response ultimately impairs the function of the brush border, producing metabolic derangements and nutritional deficiencies, as seen in our patient.
Conclusions
Celiac disease is a common cause of malabsorption that may lead to severe malnutrition in extreme cases. The literature suggests an association between celiac disease and psychiatric disorders such as those experienced by our patient, although the data are conflicting and definite conclusions are difficult to draw. At a minimum, however, we would suggest that physicians should be aware of possible association between psychiatric symptoms/disorders and celiac disease. Exacerbation of psychiatric symptoms, especially if accompanied by diarrhea, weight loss, or other indications of gastrointestinal disease, may a reasonable indication to screen for celiac disease.
References:
1.. Gujral N, Freeman HJ, Thomson AB, Celiac disease: Prevalence, diagnosis, pathogenesis and treatment: World J Gastroenterol, 2012; 18(42); 6036-59
2.. Kagnoff MF, Overview and pathogenesis of celiac disease: Gastroenterology, 2005; 128(4 Suppl. 1); S10-18
3.. Rubin CE, Brandborg LL, Phelps PC, Taylor HC, Studies of celiac disease. I. The apparent identical and specific nature of the duodenal and proximal jejunal lesion in celiac disease and idiopathic sprue: Gastroenterology, 1960; 38; 28-49
4.. Ehsani-Ardakani MJ, Nejad RM, Villanacci V, Gastrointestinal and non-gastrointestinal presentation in patients with celiac disease: Arch Iran Med, 2013; 16(2); 78-82
5.. Kemppainen T, Kröger H, Janatuinen E, Osteoporosis in adult patients with celiac disease: Bone, 1999; 24(3); 249-55
6.. Smith LB, Lynch KF, Kurppa K, Psychological manifestations of celiac disease autoimmunity in young children: Pediatrics, 2017; 139(3); e20162848
7.. Bottaro G, Cataldo F, Rotolo N, The clinical pattern of subclinical/silent celiac disease: An analysis on 1026 consecutive cases: Am J Gastroenterol, 1999; 94(3); 691-96
8.. Jamma S, Rubio-Tapia A, Kelly CP, Celiac crisis is a rare but serious complication of celiac disease in adults: Clin Gastroenterol Hepatol, 2010; 8(7); 587-90
9.. Marsh MN, Crowe PT, Morphology of the mucosal lesion in gluten sensitivity: Baillieres Clin Gastroenterol, 1995; 9(2); 273-93
10.. Husby S, Koletzko S, Korponay-Szabó IR, European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease: J Pediatr Gastroenterol Nutr, 2012; 54(1); 136-60
11.. Gonzalez JJ, Elgamal M, Mishra S, Adekolujo OS, Severe coagulopathy as a rare feature of celiac crisis in a patient previously diagnosed with celiac disease: Am J Case Rep, 2019; 20; 290-93
12.. Bul V, Sleesman B, Boulay B, Celiac disease presenting as profound diarrhea and weight loss – a celiac crisis: Am J Case Rep, 2016; 17; 559-61
13.. Balaban DV, Dima A, Jurcut C, Celiac crisis, a rare occurrence in adult celiac disease: A systematic review: World J Clin Cases, 2019; 7(3); 311-19
14.. Khorana MM, Khorana AA, Measuring quality: JAMA, 2019; 322(21); 2077-78
15.. : IBM Watson Health, Colorado, USA, Greenwood Village https://www.micromedexsolutions.com/
16.. Taddeucci G, Bonuccelli A, Polacco P, [Diagnosis of coeliac disease in patients with isolated neuropsychological symptoms. Cases reports]: Pediatr Med Chir, 2005; 27(6); 43-45 [in Italian]
17.. Slim M, Rico-Villademoros F, Calandre EP, Psychiatric comorbidity in children and adults with gluten-related disorders: A narrative review: Nutrients, 2018; 10(7); 875
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250