25 April 2021: Articles 
May-Thurner Syndrome with Double Compression of the Iliac Vein: Lessons Based on a Case Report
Challenging differential diagnosis, Rare disease, Educational Purpose (only if useful for a systematic review or synthesis)
Renato Farina1ABCDEF*, Pietro Valerio Foti1BEF, Francesco Aldo Iannace1BEF, Andrea Conti1BEF, Isabella Pennisi1BEF, Pietro Coppolino1BEF, Tiziana Vasile1BE, Cecilia Gozzo1BE, Giovanni Failla1BE, Antonio Basile1BEDOI: 10.12659/AJCR.928957
Am J Case Rep 2021; 22:e928957
Abstract
BACKGROUND: May-Thurner syndrome, also known as Cockett’s syndrome, is characterized by vascular alterations due to stenosis of the left iliac vein, usually caused by compression against the vertebral column by the right iliac artery. Doppler ultrasound represents the first level of examination for the study of this vascular pathology, and allows a very accurate study of the lower-limb vessels. We describe an unusual presentation with double stenosis of the left common iliac vein.
CASE REPORT: A 73-year-old woman came to the clinic for acute onset of worsening dyspnea, with lymphedema of the left lower limb, and was examined using ultrasound and multidetector computed tomography. The Doppler ultrasound exam showed 2 compressions of the common iliac vein by the right and left iliac artery due to a combination of osteophytosis of the vertebral column and reduced distance between the left iliac vein and the spine.
CONCLUSIONS: May-Thurner syndrome should be suspected in patients with symptoms of venous stasis of the left lower limb. Doppler ultrasound identified stenosis of the common iliac vein and the consequent flow changes. Failure to diagnose and treat May-Thurner syndrome could expose patients to very serious risks to their health.
Keywords: Cardiovascular Abnormalities, May-Thurner Syndrome, multidetector computed tomography, Ultrasonography, Doppler, Color, Constriction, Pathologic, Iliac Artery, Iliac Vein, Phlebography
Background
May-Thurner syndrome (MTS) was described in 1957 by May and Thurner as a vascular anomaly due to stenosis of the left common iliac vein (LCIV) caused by the contiguous iliac artery pushing the LCIV against the vertebra [1]. The disease is also known as Cockett’s syndrome [2]. If the space separating the iliac arteries from the spine is narrowed, either congenitally or acquired, it can cause venous compression (Figure 1A, 1B). Stenosis results when chronic pulsing of the arterial vessel leads to accumulation of elastin and collagen in the vein, causing a progressive hardening and reduction of the lumen with consequent venous stasis and chronic thrombosis [3]. Ultrasound is the first-level exam for patients with MTS, and allows a very accurate study of the iliac vessels. Multidetector computed tomography (MDCT) can also be used in these patients to exclude any utero-adnexal neoplasms [4], abdominal aortic dilations [5], uterine myoma [6], spinal listhesis [7], pulmonary embolism [8], or cerebral embolism [9]. MDCT can also show the compression of the LCIV as well as the venous thrombosis [10]. Magnetic resonance imaging (MRI) can highlight the alterations brought about by MTS, and can be used in cases of renal insufficiency to avoid the nephrotoxicity of the contrast agents used in MDCT [11]. In MTS, the stenosis of the LCIV is almost always caused by RCIA. We describe a case with LCIV double stenosis of the common iliac arteries due to the combination of an osteophytosis of the spine and reduced distance between the LCIA and the vertebral column.
Case Report
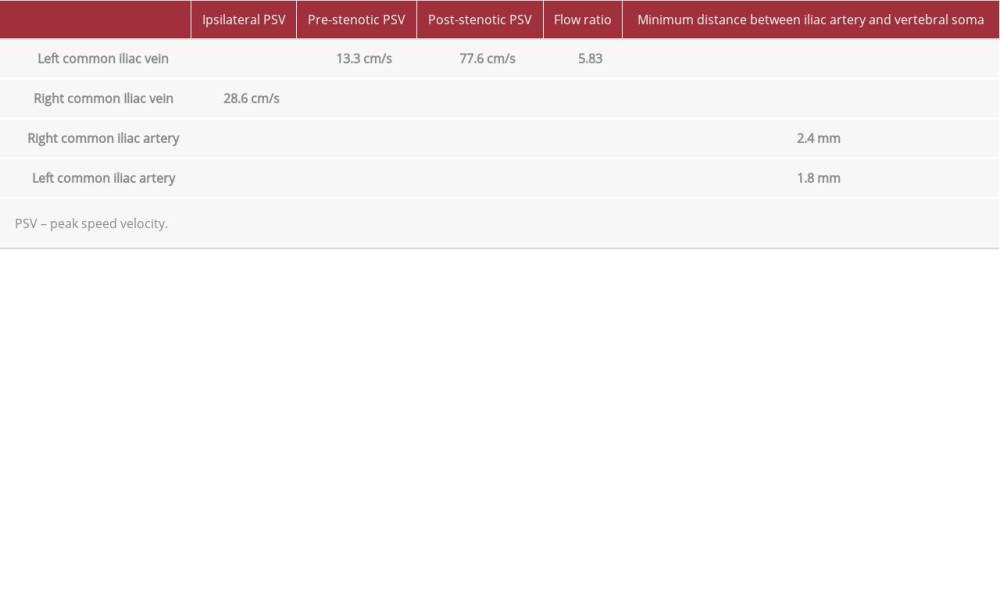
A 73-year-old woman came to our clinic for acute onset of worsening dyspnea, with lymphedema of the left lower limb. The patient initially underwent MDCT angiography of the pulmonary arteries and deep vessels of the legs using a 64-slice CT device and was subsequently subjected to ultrasound examination performed with a Toshiba ultrasound system, using a 3.5 MHz transducer with B-mode ultrasound and Doppler ultrasound techniques. The ultrasound was performed with the patient in supine position for the study of the arterial and venous vessels. Ultrasound examination was performed by an operator with 20 years of experience. The following were measured in detail: pre- and post-stenotic LCIV peak speed velocity (PSV); flow ratio (FR) obtained from the difference between the speed peak after (Video 1) and before (Video 2) stenosis; the thickness of the iliac-vertebral space measured between the arterial wall and the adjacent vertebra; and diameter and and reduction of the iliac-vertebral space (Figure 5). No morphological or flowmetric changes were detected in the arterial vessels or RCIV by either ultrasound or MDCT. In our case, the patient was prescribed drug therapy: 15 mg oral rivaroxaban twice daily for the first 4 weeks, followed by 10 mg oral rivaroxaban and 100 mg aspirin once daily for the next 6 months.
Discussion
Ultrasound allowed us to identify the stenosis and partial thrombosis of the LCIV, and also made it possible to very accurately measure the minimum distances between the iliac arteries and the spine, which showed a more severe stenosis by the LCIA. There is still no cut-off value in the literature on the iliac-vertebral space below which MTS occurs, which would be very useful for the diagnosis, as in the case of other vascular flow of the RCIV for comparison. The following results were obtained: First, the LCIV color Doppler ultrasound showed 2 ste-noses, one sustained by an osteophyte of the fifth lumbar vertebra that reduced the space between the RCIA and the spine and the other due to reduced space between the LCIA and the fifth lumbar vertebra. Second, the duplex Doppler ultrasound of the LCIV showed a flow with low PSV in the portion of the vein upstream of the venous compression and an increase in PSV downstream of the venous compression (Figure 2A–2D). Color Doppler ultrasound also showed a partial thrombosis of the LCIV, which extended from the stenosis for a distance of 2 cm toward the iliac bifurcation (Figure 3A, 3B). The flow ratio of the LCIV was 5.83. The results are summarized in Table 1. Chest MDCT angiography examination showed enhancement defects in some branches of the right pulmonary artery compatible with pulmonary embolism (Figure 4A, 4B), double stenosis of the LCIV (Figure 4C, 4D), partial thrombosis of the LCIV, compression syndromes [12]. The measurements of the PSV values in the LCIV performed with duplex Doppler ultrasound were very important because they allowed us to have information on the degree of stenosis through the calculation of flow ratio. The flow ratio value was necessary to determine the correct therapy, which requires adjustment to the severity of the stenosis. To be considered hemodynamically significant, a venous stenosis must have a flow ratio greater than 2.5 cm/s [13], which corresponds to 50% stenosis. In the present case, the stenosis was very severe; greater than 70%, and was certainly one of the causal factors of the thrombosis. Doppler ultrasound can be limited by excessive intestinal meteorism and obesity, which can hinder the complete visualization of the iliac veins in 20–50% of patients, and by deeply positioned common iliac veins, which reduces the sensitivity of the method. The treatment of first choice for MTS patients is generally the combined use of drugs (thrombolytic and anticoagulants) and endovascular stenting. In our case, long-term thrombolytic and anticoagulant drug treatment was not accompanied by endovascular stenting due to the reduced iliac-vertebral space, especially at the level of the osteophytosis, which did not guarantee a good long-term stent seal. The diagnosis of MTS is almost always made after the appearance of venous stasis in the left lower limb. In asymptomatic patients, the finding of a compression of the LCIV is often random and the discovery usually occurs following routine computed tomography or ultrasound examinations; in these patients we suggest measuring the degree of stenosis of the LCIV for possible long-term anticoagulant prophylaxis if the value is close to or greater than 50%. MTS is not a well-known disease; it has only been observed in 2–3% of cases of vein thrombosis of the lower limbs. As 60% of all MTS cases involve the left venous circulation, the incidence of MTS is probably higher than the documented cases would suggest.
Conclusions
In cases such as the present case described here, ultrasound examination is important because duplex Doppler confers the ability to estimate the degree of stenosis of the LCIV. We recommend thorough examination of the LCIV with Doppler ultrasound in all patients with left-limb symptoms, especially those with risk factors such as pregnancy [14] or prolonged immobilization, to exclude MTS. Failure to diagnose and treat MTS could expose patients to very serious risks to their health.
Figures
References:
1.. May R, Thurner J, The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins: Angiology, 1957; 8(5); 419-27
2.. Díaz de Santiago I, Insausti Gorbea I, De Miguel Gaztelu M, [May-Thurner syndrome, diagnosis and treatment: A case report.]: An Sist Sanit Navar, 2019; 42(1); 79-82 [in Spanish]
3.. Ankit M, Hussein H, May-Thurner syndrome: StatPearls, Treasure Island (FL), StatPearls Publishing Accessed Jan 2020
4.. Barnaby J, Martynov A, Shah S, Giant subserosal myoma causing deep venous thrombosis in a patient with pre-existing May-Thurner syndrome: Radiol Case Rep, 2020; 15(6); 644-49
5.. Yi JA, Hadley JB, Kuwayama DP, Atypical May-Thurner syndrome caused by endovascular aortic aneurysm repair: J Vasc Surg Cases Innov Tech, 2020; 6(3); 397-400
6.. Maruyama T, Miyamoto A, Endovascular strategy for deep vein thrombosis caused by a huge uterine myoma accompanied by May-Thurner syndrome: A case report: Radiol Case Rep, 2020; 15(10); 1921-26
7.. Delara R, Cornella J, Knuttinen MG, May-Thurner syndrome from spinal anterolisthesis: J Minim Invasive Gynecol, 2021; 28(2); 160-61
8.. Farina R, Foti PV, Iannace FA, May Thurner syndrome: Description of a case with unusual clinical onset: J Ultrasound, 2020 [Online ahead of print]
9.. Ghezzo A, Adri D, Ruberto J, Cerebral embolism as an atypical presentation of May Thurner syndrome: Medicina (B Aires), 2019; 79(6); 502-5
10.. Gozzo C, Giambelluca D, Cannella R, CT imaging findings of abdominopelvic vascular compression syndromes: What the radiologist needs to know: Insights Imaging, 2020; 11(1); 48
11.. Hsu YC, Huang YK, Hsu LS, Using non-contrast-enhanced magnetic resonance venography for the evaluation of May-Thurner syndrome in patients with renal insufficiency: A case report: Medicine (Baltimore), 2019; 98(52); e18427
12.. Farina R, Iannace FA, Foti PV, A Case of nutcracker syndrome combined with Wilkie syndrome with unusual clinical presentation: Am J Case Rep, 2020; 21; e922715
13.. Labropoulos N, Borge M, Pierce K, Criteria for defining significant central vein stenosis with duplex ultrasound: J Vasc Surg, 2007; 46(1); 101-7
14.. Singh N, Kaur M, Jirankali V, May-Thurner syndrome: An uncommon and incidental finding in a postpartum female: Pol J Radiol, 2019; 84; e365-67
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250