19 May 2021: Articles 
Perianal Solitary Fibrous Tumor in a Rare Anatomical Presentation: A Case Report and Literature Review
Challenging differential diagnosis, Rare disease
Daniel Paramythiotis1AG, Moysis MoysidisDOI: 10.12659/AJCR.929742
Am J Case Rep 2021; 22:e929742
Abstract
BACKGROUND: Solitary fibrous tumors (SFTs) account for <2% of all soft tissue tumors and are slow-growing neoplasms of mesenchymal origin, which have been reported in various locations. They are frequently observed at the pleura and a perianal location is extremely rare. They show no predisposition by sex, are mainly benign, and usually occur between the 5th and 7th decades of life.
CASE REPORT: We report the case of an 80-year-old man with no comorbidities except hypertension, who presented with an asymptomatic perineal mass. Magnetic resonance imaging showed a solid tumor measuring 3.5×2.5 cm identified in the perineal midline. It was very close to the anal sphincter, showing no extension to the rectum or anus. The tumor was completely excised with negative margins. The postoperative course was uneventful and he was discharged home, free of any symptoms. The pathological examination showed a benign completely excised SFT, and no further treatment was necessary. At the 6-month and 1-year follow-ups, there was no sign of recurrence.
CONCLUSIONS: A comprehensive review of all the reported cases of perianal SFTs shows that the majority of these tumors present with no symptoms and have a favorable prognosis. Diagnosis is possible only after a pathological examination. The criterion standard of treatment is complete excision with negative margins. Once excised, the tumors have low rates of recurrence and metastasis. Tumors very close to the anal sphincter and with malignant potential need to be operated on with extra care to obtain clear margins without disrupting the continence mechanism.
Keywords: Anal Gland Neoplasms, Perineum, Solitary Fibrous Tumors, Aged, 80 and over, Magnetic Resonance Imaging, Soft Tissue Neoplasms
Background
Solitary fibrous tumors (SFTs) are fibroblastic tumors of mesenchymal origin, with a predominantly pleural localization. Klemperer and Rabin first reported them in 1931 [1]; however, over the years, SFTs have been found in other extrapleural sites. SFTs have been found in the limbs, pelvic cavity, abdominal cavity, neck, and central nervous system [2,3]. A perianal location is rare for this type of tumor. SFTs account for <2% of soft tissue tumors and occur with a similar frequency in both sexes between the 5th and 7th decades of life [4,5].
Although the majority of SFTs are benign, some malignant tumors have been reported. Approximately 15% to 20% of SFTs are malignant either at the beginning of the disease or as a recurrence of a previously benign tumor [5,6]. The diagnosis of these tumors depends on histological and immunohistological findings [7]. The main treatment is surgical resection with negative margins, and embolization of the tumor-feeding arteries contributes to the best surgical result [6–8].
Case Report
An 80-year-old man presented at the Outpatient Clinic with a palpable mass on his perineum and right gluteal region (Figure 1). His past medical history was unremarkable except for hypertension. He did not report any gastrointestinal symptoms, his bowel movements were regular, and he did not notice any blood or mucus excretion. His laboratory test results were normal and the preoperative tests revealed that all tumor markers were negative. He underwent magnetic resonance imaging (MRI) of the pelvis and perineum, and a solid mass was identified in the perineal midline, measuring 3.5×2.5 cm. The mass had a mixed intermediate signal, clear margins, close affinity to the external anal sphincter, and no extension to the rectum (Figure 2A, 2B).
Based on these findings, our differential diagnosis included a lipoma or a liposarcoma, a neurogenic tumor, including a neurinoma or a schwannoma, a gastrointestinal stromal tumor, and some other rare soft tissue tumors, including a hemangiopericytoma or a spindle-cell tumor. The patient and the medical team made a shared decision to opt for an excision biopsy rather than a pre-operative fine-needle aspiration (FNA) biopsy. This decision was based on the increased risk of bleeding and biopsy track seeding that accompanies the FNA biopsy of tumors with high vascularity, along with the knowledge based on radiology that the tumor was excisable. Our proposal for an excision biopsy was backed by the patient’s wish to have the mass completely removed, regardless of whether it was benign or malignant. Depending on the results of the postoperative pathologic examination, more investigations would be undertaken to check for distant metastasis.
The patient was scheduled for an operation. He was placed in the lithotomy position and through a perineal incision we completely excised the mass with clear margins. The defect was closed with interrupted stitches using nylon 2/0. Despite the tumor being close to the external anal sphincter, it was not attached to it and we decided not to sacrifice any muscle fibers (Figure 3A–3C).
The pathological examination revealed a tumor measuring 3.4 cm at its larger dimension, with a grayish cut surface. Sections from the tumor showed a spindle-cell neoplasm with medium to high cellularity. The neoplastic cells were organized in whorls or bands. The nuclei were oval-shaped or elongated with low atypia. There were no mitoses or sites of necrosis. Immunohistochemical control showed positivity for vimentin, Bcl2 (Figure 4A), epithelial membrane antigen, and antigens CD34 (Figure 4B), CD10, and CD99. The neoplastic cells were negative for activin receptor-like kinase 1, smooth muscle actin, desmin, cytokeratins AE1/AE3, S100 protein, and antigens CD45 and CD117. The mitotic index Ki67/MIB1 was positive for 2% of neoplastic cells. Based on the morphological and immunohistochemical findings, the diagnosis of an SFT was finalized (Figure 4C). After the mass had been completely excised, no signs of malignancy were detected. The postoperative course was uneventful and he was discharged from the hospital on postoperative day 2. Since then, there have been no signs of incontinence.
At the 6-month postoperative follow-up, the wound had healed well and there was no clinical recurrence on palpation and rectal examination. We did not have the chance to use computed tomography (CT) or MRI to exclude recurrence because the patient refused these investigations. Physical examinations 1 year after surgery have revealed no recurrence to date. He does not have any symptoms or swelling related to the SFT and he reports 1 or 2 bowel movements per day with type 3 or type 4 stools according to the Bristol Stool Chart. The patient gave informed consent to publish this case report and the Ethics Board of AHEPA University General Hospital approved the publication.
Discussion
Although SFTs were initially reported only in the visceral pleura, these tumors can occur in almost every part of the human body [2]. However, a perineal location is rare, and to our knowledge, our case is the 4th reported in the literature. Suster et al, Kim et al, and de Souza Melo et al have reported similar observations [4]. Therefore, this case report is interesting and useful to avoid misdiagnosis and achieve early treatment. Our research revealed more reported cases that refer to the same condition and anatomic region under different names. In this study, we have included all reported cases of perineal, peri-anal, ischiorectal fossa, and ischioanal fossa SFTs (Table 1) [4,6,9–18]. We excluded cases of pelvic, retroperitoneal, and urinary tract SFTs from our review given the notable differences in their diagnostic and treatment strategies, including the surgical approach.
We researched the literature using PubMed, Scopus, and Embase. The keywords we used were “solitary fibrous tumor”, “perineal tumors”, and “perineum.” Our search began from 1995, when the first case of a perianal SFT was reported. We excluded articles written in languages other than English or Greek. The search produced 12 published cases (ours is the 13th). Suster et al reported the first case series about SFTs in 1995.
The patients’ ages vary from 19 years to 80 years (average 50 years). The patients in the 13 cases were 9 men and 4 women. All the patients underwent surgical intervention. Tumor sizes ranged from 1.6 cm to 23.0 cm, averaging 8.5 cm with a median of 6.5 cm. We calculated the Demicco risk score for all the cases to assess the long-term risk of metastasis [19]. Seven cases were low-risk for metastasis and the remaining 6 cases were classified as an intermediate risk for long-term metastasis. Follow-up data were available for 7 cases; metastasis recurred only in 1 case, which was the recurrence of a tumor excised 13 years ago [4,6,9–18].
The morphology of an SFT is characteristic; however, it is the staining pattern of the tumors that is unique and helps in the differential diagnosis from other spindle-cell tumors. SFT cells are spindle-shaped and ovoid, they are arranged in a patternless pattern around the hyalinized vasculature with a collagenous background, as described by Adrian Fernandez et al [8]. SFTs are positive for 4 stains (STAT6, CD34, CD99, and Bcl-2). According to the literature, although CD34 is the most commonly used stain to determine SFTs, STAT6 is the most specific and sensitive [3,6–8]. The STAT6 stain is not included in our department’s immunohistochemical panel and therefore was not available for the present case.
SFTs have no specific symptoms and their clinical behavior can be unpredictable because they tend to be slow-growing painless masses. They are diagnosed incidentally when they are large in size, as occurred in the present case. The symptoms depend on the location and size of the tumors. Intra-abdominal tumors can occur as a palpable mass causing pain and weight loss. They can lead to constipation, incontinence, and vomiting. SFTs in the urinary tract can cause dysuria, hematuria, and nocturia [3,4]. Paresthesia and other nerve symptoms can occur if the tumor affects a nerve. The literature reports that SFTs are related to 2 different paraneoplastic syndromes, which are non-islet cell tumor hypoglycemia or Doege-Potter syndrome and hypertrophic osteoarthropathy [3,4,8].
As diagnosis is difficult based on the main symptoms, CT and MRI scans in combination with histopathological and immunohistological findings are necessary for the early diagnosis of SFTs. Although MRI images can be nonspecific as the tumors can appear with necrosis, hemorrhage, and myxoid or cystic appearance, SFTs usually have heterogeneous signal intensity on T1- and T2-weighted images. On T2 sequences, intense enhancement can indicate the rich vascularity of the tumor. Both benign and malignant SFTs can show heterogeneous, isointense, and hyperintense signals on T2 images [5]. After the injection of gadolinium, the tumor shows heterogeneous enhancement. In the present case report, the tumor had a homogeneous signal intensity, which was high on T2 sequences and intermediate on T1 sequences. After the injection of an intravenous paramagnetic dye for imaging enhancement, the tumor had a heterogeneous high-intensity signal. For perineal and perirectal SFTs, MRI can provide detailed information regarding their relationships to the surrounding soft tissue structures, which is difficult to obtain via CT scans. On CT scans, SFTs demonstrate heterogeneous attenuation and calcification occurs in 20% to 30% of these tumors [5].
Preoperative biopsies, in the form of a CT, ultrasound-guided FNA, or core biopsy, are not useful in finalizing the diagnosis [4]. In our review, only 2 out of the 13 cases (including ours) had a preoperative biopsy. From these 2 cases, Bhat et al report that a CT-guided biopsy was performed; however, it was complicated with intralesional hemorrhage [16]. In the report by Morikawa et al, an ultrasound-guided biopsy was performed to assist with the management strategy, as the patient was reluctant to have an operation in case of a benign lesion. Despite the histological outcome of an SFT, the patient underwent an excision, considering the future malignant potential of the lesion [15]. In both cases, extra care was taken during the operation to remove the biopsy track on the clear margins to avoid tumor seeding. The authors believe that the decision for conducting a preoperative biopsy should be individualized.
Although the majority of SFTs are benign, studies in the literature suggest 5% to 26% of the tumors are malignant [3] and even benign tumors have malignant potential. Some important indicators that increase the malignancy potential in an SFT are necrosis, polymorphism, increased cellularity, and ≥4 mitotic figures per 10 high-power fields. A tumor >10 cm in size, hemorrhage, infiltrative margins, and anaplastic foci can have an unfavorable prognosis and point to malignancy [3,7]. Demicco et al have recently proposed a risk stratification model where patients are divided into low, intermediate, and high risk of SFT long-term metastasis, based on tumor size, mitotic count, the patient’s age at diagnosis, and tumor necrosis (Table 2) [19]. The Demicco risk score is probably the best and easiest system to use in general practice. It is used to estimate not only the overall survival but also the progression-free survival of patients. The advantage is that it can be applied to SFTs in any anatomical location.
There are several studies in the literature about the treatment for SFTs. All of them suggest complete en bloc surgical resection with negative margins as the appropriate treatment for localized tumors and for improving overall survival [2,4,7]. The study by Wang et al suggested that a piecemeal resection of the total tumor can lead to local control of the disease [2]. Embolization of the tumor before surgical treatment is useful to decrease tumor size [5]. Postoperative radiotherapy can be useful for elimination of the disease, as SFTs are considered to be chemoresistant [3]. A long-term follow-up using a clinical examination as well as CT and MRI scans of the chest and abdomen are necessary for all patients with SFTs, as the possibility of repeated recurrences or a malignant transformation of the tumor cannot be excluded due to the biological behavior of the disease [3,4,7]. It has been reported that approximately 6% of patients with benign tumors in histological exams have the possibility of recurrence [3]. In the present case, the patient underwent surgical treatment and no sign of recurrence has been detected 1 year after the operation.
Conclusions
In conclusion, SFTs of the perineal region can pose a diagnostic challenge to the clinician, as one cannot identify pathognomonic signs in any imaging modality, and in the majority of cases, a preoperative biopsy is not helpful. Complete excision is sufficient treatment in most cases. Surgery on tumors with a close relationship to the anal sphincter need extra care so as not to disrupt the continence mechanism. To obtain clear margins, a more elaborate surgical approach is needed in cases with malignant potential.
Figures
References:
1.. Klemperer P, Coleman BR, Primary neoplasms of the pleura. A report of five cases: Am J Ind Med, 1992; 22(1); 1-31
2.. Wang Y, Wei R, Ji T, Surgical treatment of primary solitary fibrous tumors involving the pelvic ring: PLoS One, 2018; 13(11); e0207581
3.. Ge X, Liao J, Choo RJ, Solitary fibrous tumor of the ilium: A case report: Medicine (Baltimore), 2017; 96(51); e9355
4.. Melo PA, Yoshino Bonifaci AM, Crochik FD, Giant perineal solitary fibrous tumor: A rare case report: Case Rep Urol, 2017; 2017; 4876494
5.. Boe J, Chimpiri AR, Liu CZ, Solitary fibrous tumor originating in the pelvis: A case report: J Radiol Case Rep, 2010; 4(7); 21-28
6.. Zheng CG, Jin C, Ye LC, A rare perianal tumor: Solitary fibrous tumor: Tech Coloproctol, 2015; 19(5); 323-24
7.. Rovegno FA, Hernandez CY, Gradin S, Solitary fibrous tumor of the pelvis involving the bladder. Case report and literature review: Urol Case Rep, 2019; 24; 100864
8.. Fernandez A, Conrad M, Gill RM, Solitary fibrous tumor in the abdomen and pelvis: A case series with radiological findings and treatment recommendations: Clin Imaging, 2018; 48; 48-54
9.. Suster S, Nascimento AG, Miettinen M, Solitary fibrous tumors of soft tissue. A clinicopathologic and immunohistochemical study of 12 cases: Am J Surg Pathol, 1995; 19(11); 1257-66
10.. Kim MY, Rha SE, Oh SN, Case report. Lipomatous haemangiopericytoma (fat-forming solitary fibrous tumour) involving the perineum: CT and MRI findings and pathological correlation: Br J Radiol, 2009; 82(974); e23-26
11.. Yoshida R, Takada H, Iwamoto S, A solitary fibrous tumor in the perianal region with a 13-year follow-up: Report of a case: Surg Today, 1999; 29(7); 642-45
12.. Occhionorelli S, Pigato I, Malvicini E, Solitary fibrous tumour of gluteus: A case report about an uncommon localization of a rare neoplasm: J Surg Case Rep, 2016; 2016; rjw111
13.. Kim K, Cha S, Yeom S, Solitary fibrous tumor of the ischiorectal fossa: CT and MRI findings: Journal of the Korean Society of Magnetic Resonance in Medicine, 2011; 15(1); 72-76
14.. Yap T, Hamzah L, Oshowo A, Myxoid solitary fibrous tumour of the ischiorectal fossa: Eur J Surg Oncol, 2003; 29(1); 98-100
15.. Morikawa K, Takenaga S, Masuda K, A rare solitary fibrous tumor in the ischiorectal fossa: a case report: Surg Case Rep, 2018; 4(1); 126
16.. Bhat A, Layfield LJ, Tewari SO, Solitary fibrous tumor of the ischio-anal fossa – a multidisciplinary approach to management with radiologicpathologic correlation: Radiol Case Rep, 2018; 13(2); 468-74
17.. Dudkiewicz M, Deschênes JL, Bloom C, Solitary fibrous tumor of the ischioanal fossa: Report of a case and review of the literature: Dis Colon Rectum, 2004; 47(4); 535-37
18.. Mourra N, Lewin M, Sautet A, Epithelioid solitary fibrous tumor in the ischioanal fossa: Virchows Arch, 2005; 446(6); 674-76
19.. Demicco EG, Wagner MJ, Maki RG, Risk assessment in solitary fibrous tumors: Validation and refinement of a risk stratification model: Mod Pathol, 2017; 30(10); 1433-42
Figures
Tables
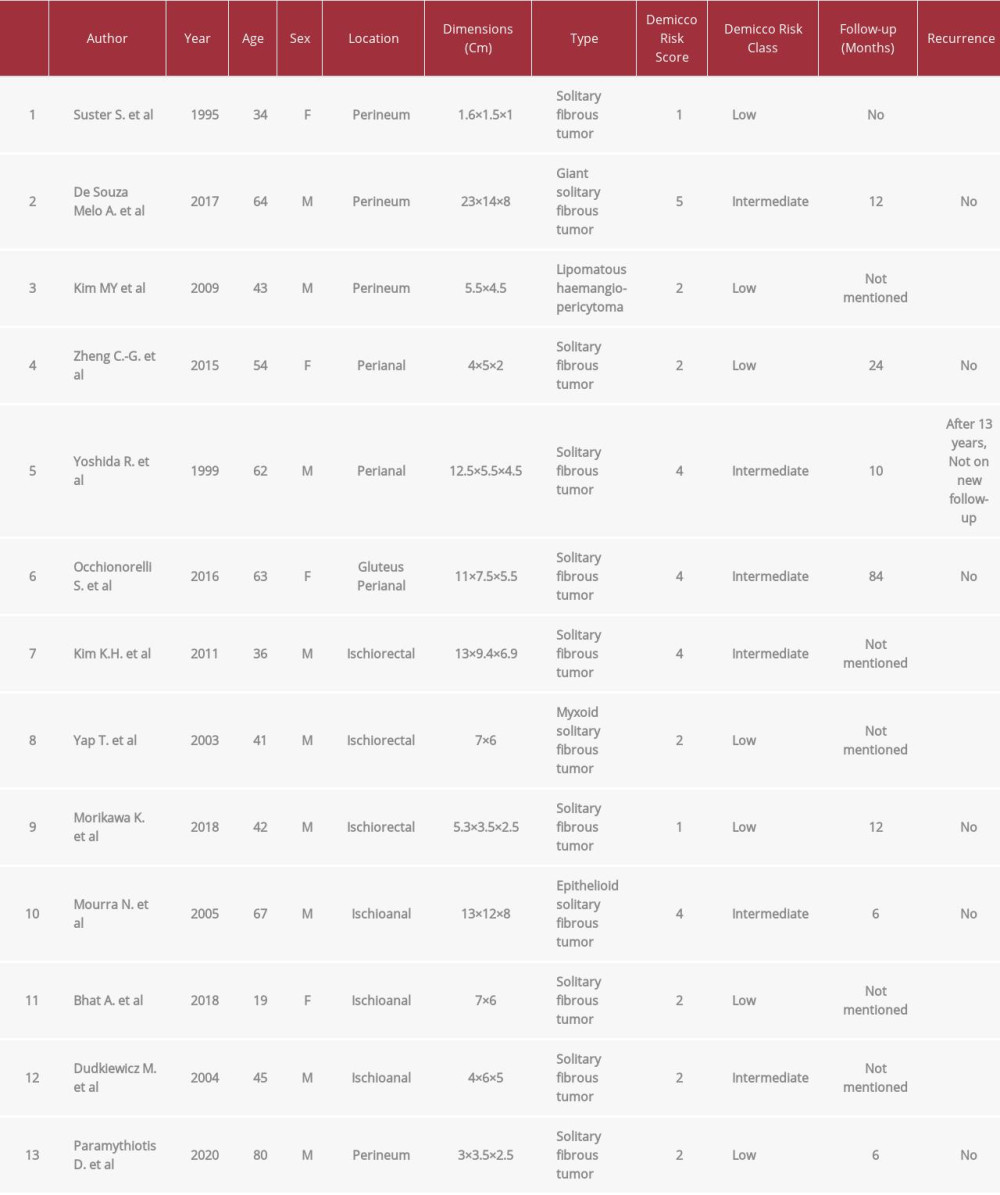 Table 1.. Clinical features of all 13 reported cases of Solitary fibrous tumor of the ischiorectal, ischioanal, perineal, perianal region [4,6,9–18].
Table 1.. Clinical features of all 13 reported cases of Solitary fibrous tumor of the ischiorectal, ischioanal, perineal, perianal region [4,6,9–18].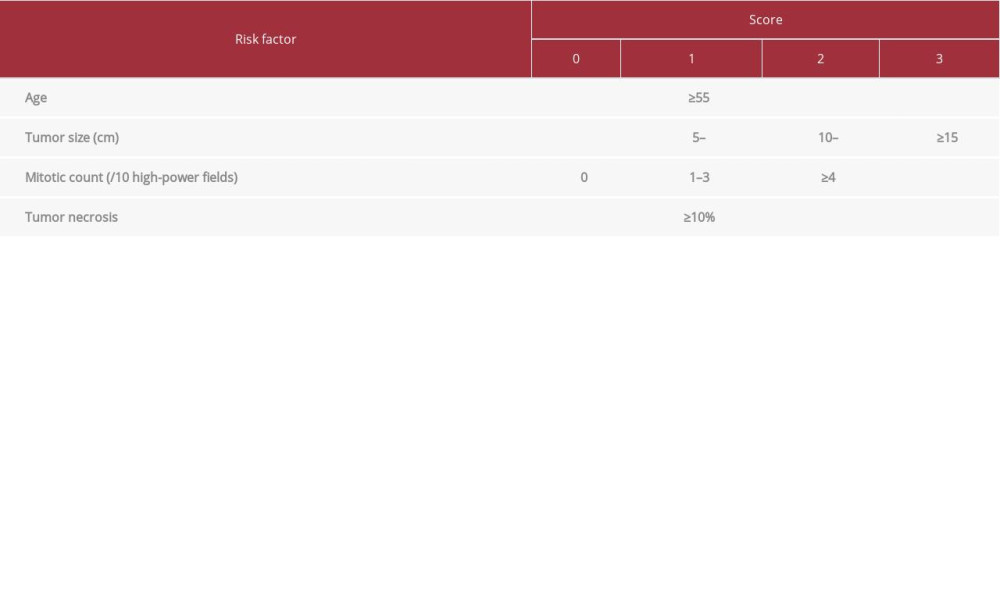 Table 2.. Risk Stratification Model proposed by Demicco et al. [19].
Table 2.. Risk Stratification Model proposed by Demicco et al. [19].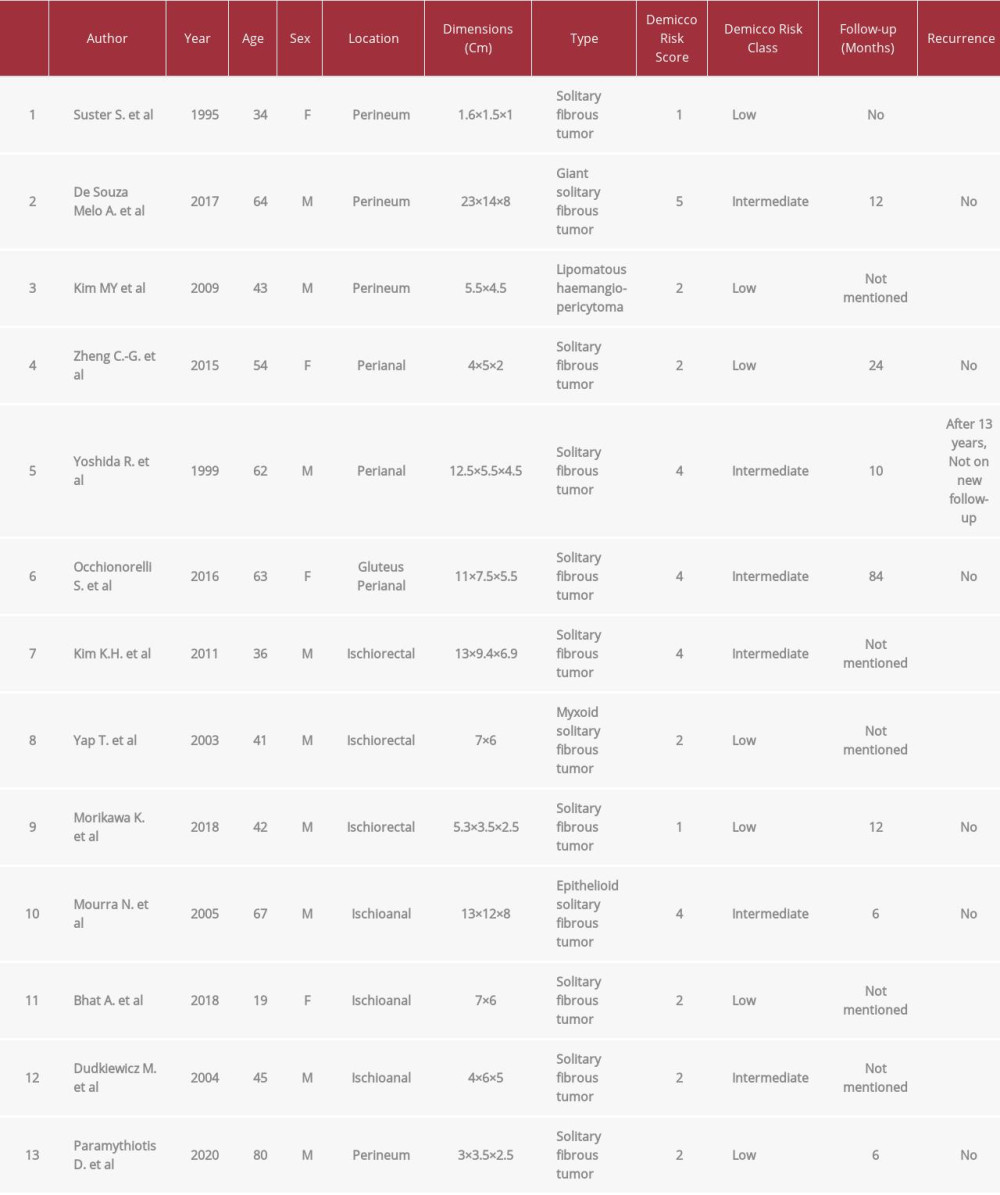 Table 1.. Clinical features of all 13 reported cases of Solitary fibrous tumor of the ischiorectal, ischioanal, perineal, perianal region [4,6,9–18].
Table 1.. Clinical features of all 13 reported cases of Solitary fibrous tumor of the ischiorectal, ischioanal, perineal, perianal region [4,6,9–18].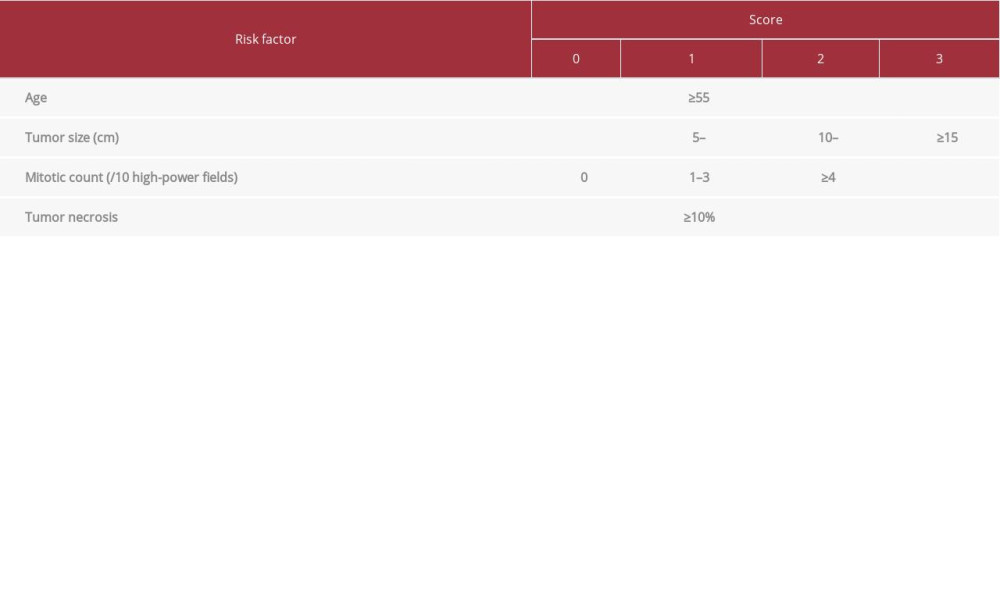 Table 2.. Risk Stratification Model proposed by Demicco et al. [19].
Table 2.. Risk Stratification Model proposed by Demicco et al. [19]. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








