27 July 2021: Articles 
Laparoscopic Surgery for Diagnosis and Treatment of Acute Right Upper-Quadrant Abdominal Pain Due to Omental Infarction: A Report of a Rare Case in a Single Vietnamese Hospital
Challenging differential diagnosis, Diagnostic / therapeutic accidents, Management of emergency care, Rare disease
Tran Que Son12ABCDEF*, Tran Hieu Hoc1ACDF, Vu Duc Long2DE, Tran Thanh Tung2DF, Pham Van Tuyen3CD, Nguyen Toan Thang4CF, Tran Thu Huong5EGDOI: 10.12659/AJCR.931098
Am J Case Rep 2021; 22:e931098
Abstract
BACKGROUND: Omental infarction (OI) is an infrequent cause of acute abdominal pain, and there is no consensus on whether conservative or surgical treatment should be performed. The clinical manifestations are nonspecific, so many patients are referred for surgery because of acute abdominal signs that may indicate other diseases such as cholecystitis, appendicitis, or peptic ulcer perforation. In most cases, infarction of the greater omentum is diagnosed only during emergency surgery for other diseases of the abdomen. Currently, multisequence computed tomography is performed for acute abdomen, and this disease is increasingly diagnosed preoperatively.
CASE REPORT: We report on 2 patients who were referred to our Emergency Department for acute abdominal pain. Both were female and middle-aged. The first patient presented with vomiting and right upper-quadrant pain with thickened and right subcostal omental infiltration on computed tomography (CT). The second patient presented with right subcostal pain and fever. CT showed signs of infiltration, thickening of the omentum, and a right upper subcostal mass measuring 22×60 mm. We performed emergency laparoscopic surgery to explore the abdominal cavity. Both patients were discharged after 3 days.
CONCLUSIONS: Omentum infarction is a rare disease that causes a diagnostic dilemma, as there is a wide spectrum of causes of acute abdomen. Many patients are diagnosed only during surgery. Laparoscopic surgery should be performed as soon as possible.
Keywords: Emergency Medical Services, Laparoscopy, Omentum, Infarction, Abdominal Pain, Abdomen, Acute, Asians, Hospitals
Background
Omental infarction is a rare condition in emergency surgery. Bush described the first case in 1896 [1,2]. Since then, between 250 and 400 cases have been reported [2–4]. The omentum passes downwards and then upwards to the transverse colon, draping over most of the intestine, covering a large area. For this reason, abdominal pain caused by infarction of the greater omentum can occur in many locations of the abdomen; therefore, differential diagnoses should be considered with other common surgical diseases, such as acute cholecystitis, diverticulitis, and appendicitis, depending on the location of the pain [3,5]. A definitive diagnosis should be based on clinical characteristics and computed tomography (CT) findings, but the disease is sometimes only diagnosed during surgery [3,6]. According to the literature, omental infarction can be treated early by internal medicine (antibiotics, painkillers, anti-inflammatories) and assessment of abdominal signs on follow-up. The patient should be referred to surgery only if the clinical conditions worsen [7–9]. We present 2 patients with infarction of the greater omentum, which was treated by laparoscopic omentectomy.
Case Reports
PATIENT 1:
A 56-year-old female patient was admitted to the Emergency Department (ED) following 3 days of right and epigastric abdominal pain with nausea and vomiting, no fever, and stable hemodynamics. The patient was admitted to the Poison Control Center for treatment with a diagnosis of food poisoning and digestive disorders. The patient had no history of abdominal surgery. Physical examination showed an abdominal wall reaction in the right upper quadrant.
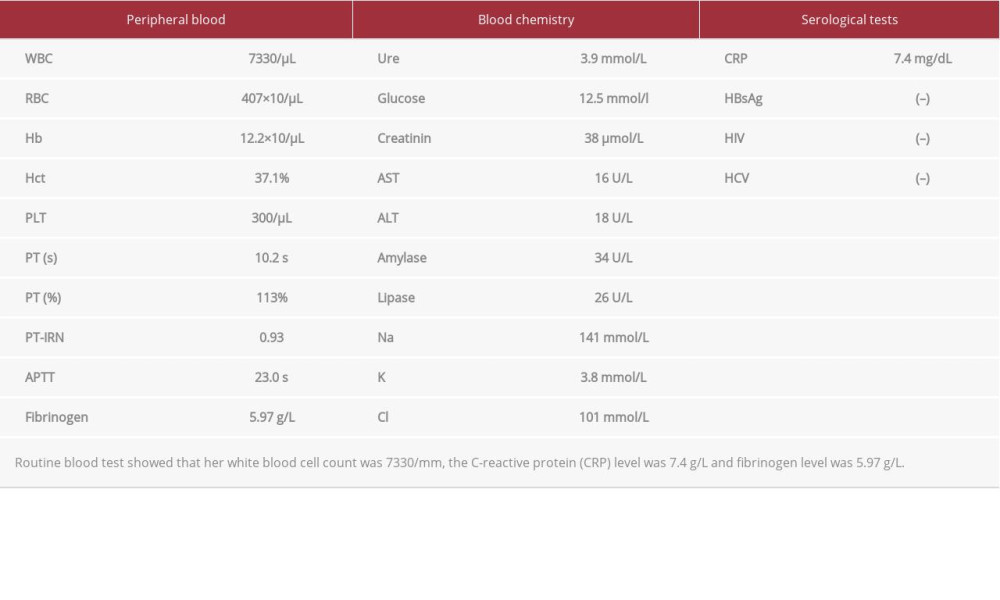
Hematologic tests showed a white blood cell (WBC) count of 7800/mL, C-reactive protein (CRP) level of 7.4 mg/dL (range, 0–1 mg/L). The other hematologic test results were normal (Table 1). Ultrasound showed high parenchymal antithesis, no masses or stones inside the bile tracts, and a gallbladder with thin walls and no stones within. No crescent sign beneath the right hemidiaphragm in the pneumoperitoneum was seen on abdominal X-ray. Computed tomography showed no free air in the abdomen, only infiltrates and thickened omentum in the right upper quadrant (Figure 1). Due to the patient’s severe pain and abdominal wall reaction, we seriously considered peptic ulcer perforation.
The patient underwent laparoscopic exploration, which revealed signs such as a small volume of fluid inside the abdomen under the liver. The gallbladder showed no signs of inflammation, and no perforation was seen inside the stomach or duodenum (Figure 2). The small intestine and colons were normal. The greater omentum was purple and black, suggesting omental necrosis approximately 4×5 cm attached to the abdominal wall and the falciform ligament (Figure 3A, 3B). These symptoms led to the final diagnosis of omental infarction. She underwent laparoscopic omentectomy to remove a portion of the necrosed greater omentum.
Histopathological results revealed necrotic inflammation of the greater omentum (Figure 4). She improved after the emergency operation. At 3-day follow-up, her symptoms had disappeared completely.
PATIENT 2:
A 58-year-old female patient with no history of surgery presented with 10 days of right-quadrant abdominal pain. She had no vomiting, no fever, and normal bowel movements. Physical examination showed an abdominal wall reaction in the right upper quadrant. There was a solid mass with a size of approximately 6×6 cm.
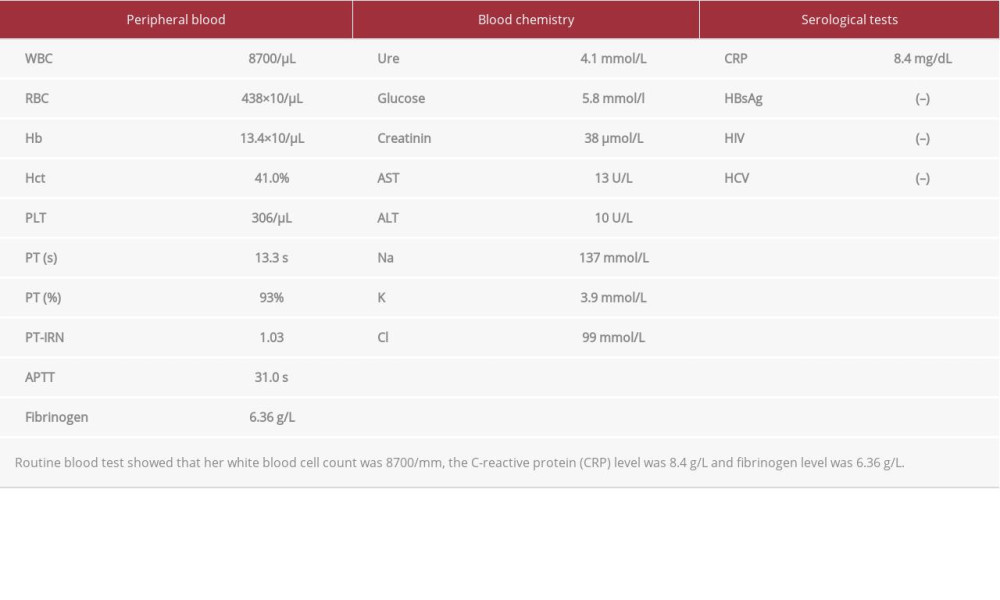
Blood tests indicated a WBC count of 8700/mL, prothrombin of 93%, fibrinogen of 6.36 g/L, and CRP of 8.4 mg/dL (Table 2). Ultrasound revealed 9-mm walls of the gallbladder, and a common bile duct with no dilation or stones. Fat had infiltrated a large area, covering almost the entire omentum in the right upper-quadrant region, with no fluid in the abdomen. A CT scan showed mass lesions measuring 22×60 mm in size, surrounded by fat inflammation and poor absorption of contrast medium, suggesting a greater omentum infarction (Figure 5). The patient was preoperatively diagnosed with greater omentum necrosis.
The patient was indicated for laparoscopic surgery. During surgery, there was no fluid in the abdomen. The greater omentum under the liver was partially necrotic. Other organs, such as the liver, stomach, duodenum, and small intestine had no abnormal signs. The patient underwent laparoscopic omen-tectomy to remove the necrotic omentum (Figure 6A, 6B).
Histopathological results showed many areas of bleeding in the greater omentum and large amounts of fibrous fatty tissues, many areas of bleeding necrosis, other necrotic tissues, and chronic invasive inflammation. Postoperative follow-up showed that she had improved after the emergency operation. She was discharged after 3 days.
Discussion
Approximately 300 cases have been reported with infarction of the greater omentum [1,2]. Approximately 85% of these cases are in adults aged 40 to 50 years, with a ratio of females to males greater than 2: 1 [1,2,4]. Infarction of the omentum is classified into 2 main types: primary and secondary infarction. Regardless of the type, the histopathological process starts with edema, inflammation, embolism, necrosis, and drainage fluid in the abdomen [4,5]. Both of the patients in this case report were female, which is also consistent with common epidemiological features.
To date, the causes of this disease remain unidentified [1,4,5]. Many authors believe that congenital abnormalities of blood vessels supplying the right lower part of the greater omentum can easily cause infarctions. Other studies have suggested that, due to differences in embryonic origins, blood vessels in the right part of the greater omentum are smaller and more fragile, making them more susceptible to elongation and obstruction [8]. Some contributing factors include trauma, excessive exercise, history of abdominal surgery, a sudden increase in abdominal pressure, and increased blood clotting, especially in obesity, which increases internal fat deposition in the blood vessels supplying the omental tissue [1,2,7]. In the 2 patients we treated, the infarctions occurred in the right part of the greater omentum. Additionally, in both of their blood analyses, the fibrinogen indexes were increased to 5.97 g/L and 6.36 g/L, showing that hypercoagulability in the 2 patients may have been the cause of the infarctions (Tables 1, 2).
The clinical symptoms of necrosis of the omentum are not significant, except for initial symptoms such as acute abdominal pain, nausea, vomiting, and loss of appetite. Clinical examination can detect some abdominal reactions in the region corresponding to the location of the infarction in the greater omentum. In most cases, there is an increase in the number of WBCs and CRP. The pain caused by omental infarction is nonspecific, so it is difficult to distinguish from other surgical diseases, such as cholecystitis, appendicitis, and diverticulitis [5–7,9]. The 2 patients underwent laparos-copy due to severe abdominal pain in the right upper quadrant. The first patient also had a digestive disorder, so the initial misdiagnosis was food poisoning and perforated viscera or acute cholecystitis.
Ultrasound and CT scans are reliable means of diagnosis. A diagnosis of acute cholecystitis can be eliminated if imaging of the mass lesion demonstrates an oval shape or increasing hyperechoic fat inflammation in the same location as the abdominal pain, and free fluid in the abdomen. Ultrasound shows images of embolism in the mass and increasing perfusion around the mass [1,6,7].
Abdominal CT scans play an important role in the diagnosis of infarction of the greater omentum and in its differential diagnosis with appendicitis, cholecystitis, diverticulitis, acute pancreatitis, or visceral perforation. Imaging shows fat inflammation and varicose veins inside the injured omentum [6,7]. The abdominal wall pain may be on the right or in the middle of the abdominal walls or the epigastric region. Many authors suggest laparoscopy to make a definitive diagnosis and simultaneously treat the patient [3,4,8]. For the 2 patients we treated, ultrasound especially revealed characteristics of fat inflammation under the liver, with a mass lesion in the omentum, which was clearer in the second patient. As the disease is uncommon, with little research on it, only 1 patient was initially diagnosed correctly.
In infarctions of the greater omentum, the imaging features change over time, starting with congestion and adipose necrosis, followed by lymphocytic and tissue infiltration, and eventually fibroblasts and scarring. Omental infarction can result in complications of abscesses, such as adhesions or abdominal infection [2,7].
There is no consensus regarding the use of surgical or medical treatment. Some authors supporting nonsurgical treatment state that infarction is a self-limited disease and that most of the symptoms will be resolved after 2 weeks. Treatment with medication should be considered (antibiotics, painkillers, anti-inflammatories). In contrast, surgeons state that early surgery can reduce the length of hospital stay and the patient’s symptoms, further limiting the complications of abscesses such as adhesions or abdominal infection. Laparoscopic surgery has some advantages: [1] it can be used to examine the entire abdomen to obtain a definitive diagnosis; [2] it can be used
to wash out infectious inflammatory fluid in the peritoneum; and [3] it has minimal invasiveness, reduces the use of pain-killers, and causes little intestinal obstruction or wound infection [1–4,8]. In laparoscopic surgery, the widely used Harmonic Scalpel (Ethicon Endo Surgery Industries, Cincinnati, OH, USA) and LigaSure (Valleylab, Tyco Healthcare Group, Boulder, CO, USA) can be useful in performing very effective resection of the conjunctiva, reducing bleeding. Our patients had to undergo surgery because of severe pain, and duodenal perforation or acute cholecystitis could not be excluded. We placed 3 trocars (a 10-mm trocar in the umbilical region for the camera and two 5-mm trocars, one each in the painful regions on the left and on the right) to remove the infarcted omentum. The outcome was good, and the patients were free of pain and were discharged after 3 days.
Conclusions
Omentum infarction is a rare condition that causes a diagnostic dilemma, given the wide spectrum of causes of acute abdomen. Many cases are diagnosed only during surgery. Laparoscopic surgery should be performed as soon as possible to achieve good treatment results.
Figures
References:
1.. Kataoka J, Nitta T, Ota M, Laparoscopic omentectomy in primary torsion of the greater omentum: Report of a case: Surg Case Rep, 2019; 5(1); 76
2.. Medina-Gallardo NA, Curbelo-Pena Y, Stickar T, Omental infarction: Surgical or conservative treatment? A case reports and case series systematic review: Ann Med Surg (Lond), 2020; 56; 186-93
3.. McMillen B, Hekman DP, Nguyen MTT, Grewal D, Idiopathic omental infarction: Managed conservatively: BMJ Case Rep, 2019; 12(3); e226978
4.. Park TU, Oh JH, Chang IT, Omental infarction: Case series and review of the literature: J Emerg Med, 2012; 42(2); 149-54
5.. Gupta R, Farhat W, Ammar H, Idiopathic segmental infarction of the omentum mimicking acute appendicitis: A case report: Int J Surg Case Rep, 2019; 60; 66-68
6.. Udechukwu NS, D’Souza RS, Abdulkareem A, Shogbesan O, Computed tomography diagnosis of omental infarction presenting as an acute abdomen: Radiol Case Rep, 2018; 13(3); 583-85
7.. McCusker R, Gent R, Goh DW, Diagnosis and management of omental infarction in children: Our 10 year experience with ultrasound: J Pediatr Surg, 2018; 53(7); 1360-64
8.. Abe T, Kajiyama K, Harimoto N, Gion T, Nagaie T, Laparoscopic omentectomy for preoperative diagnosis of torsion of the greater omentum: Int J Surg Case Rep, 2012; 3(3); 100-2
9.. Nijkamp JLG, Gerretsen SC, Stassen PM, Left-sided omental infarction: a rare cause of abdominal pain, discovered by CT scan: BMJ Case Rep, 2018; 2018; bcr2017224138
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250