01 September 2021: Articles 
A Coronary Artery Anomaly Presenting as Acute Coronary Syndrome: A Case Report
Challenging differential diagnosis, Congenital defects / diseases
Mariana S. de A. Chaud1ABCDEF, Camila A. Agostinho1AB, Felipe L. Malafaia1ACDE, Márcio C. Sampaio1BD, Paulo Chaccur1ABC, Pedro Gabriel Melo de Barros e SilvaDOI: 10.12659/AJCR.931561
Am J Case Rep 2021; 22:e931561
Abstract
BACKGROUND: Coronary artery anomalies (CAAs) are rare congenital malformations with different clinical presentations and pathophysiological mechanisms. These anomalies are frequently the cause of sudden death in young patients. Most CAAs are incidental findings owing to the lack of symptoms; however, they may be associated with acute coronary syndrome in rare cases.
CASE REPORT: We describe the case of a 47-year-old man who presented with a 1-day history of progressive typical chest pain and elevated troponin levels. The patient underwent a coronary angiography, which unveiled the anomalous origin of the left main coronary artery arising from the right coronary artery, with an interarterial course between the ascending aorta and the pulmonary artery, without coronary artery disease. Coronary computed tomography angiography confirmed the CAA and its relationship with the symptoms. An uneventful coronary artery bypass graft was undertaken, and at the 1-year follow-up, the patient was asymptomatic, with a normal stress test.
CONCLUSIONS: This case depicts the presentation of atypical acute coronary syndrome in a young patient with a rare CAA. In such patients, coronary angiography and coronary computed tomography angiography are essential tools to confirm the diagnosis and to determine treatment. Although controversial, in young individuals presenting CAA with an interarterial course, such as the left main coronary artery arising from the right coronary artery, coronary artery bypass graft may be an important treatment option to avoid sudden death in the future.
Keywords: acute coronary syndrome, Coronary Angiography, Coronary Artery Disease, Death, Sudden, Cardiac, Coronary Vessel Anomalies, Humans
Background
Coronary artery anomalies (CAAs) are rare congenital malformations with a wide variance of incidence reported in the literature, ranging from 1% to 6% of the population undergoing a coronary angiography procedure and 0.3% of all autopsies [1–3]. Although these anomalies are present at birth, most CAA are found incidentally later, owing to the lack of symptoms or because symptoms may be unrecognized. Clinical findings can vary according to the subtype of the anomaly and its trajectory in the heart, yet a potential malignant course can lead to myocardial ischemia, myocardial infarction, and sudden death, particularly in young people and athletes [4]. Still, the clinical presentation as acute coronary syndrome is unusual with very few cases reported in the literature.
Case Report
We report the case of a 47-year-old male patient with recurrent and progressive typical chest pain, which started 1 day earlier and resolved spontaneously. The patient was later admitted at the Emergency Department with sudden worsening of the chest discomfort. He had a past medical history of hypertension, hyperlipidemia, and obesity, in addition to a family history of myocardial infarction in his mother and father at ages 50 and 45 years, respectively. He had no prior history of smoking, alcohol, or other substance abuse.
On admission, the patient’s vital signs were a heart rate of 68 beats/min, blood pressure of 110/70 mm Hg, oxygen saturation of 98% on room air, and a respiratory rate of 12 breaths/min. His physical examination was otherwise unremarkable. A resting electrocardiogram (Figure 1) showed a normal sinus rhythm with T wave abnormality in the inferolateral leads (I, II, III, aVL), without ST segment depression. Serial troponin T concentrations increased from 41 to 197 ng/L (reference value: <14 ng/L). Other findings from blood analysis were within normal ranges.
An acute non-ST-segment elevation myocardial infarction was diagnosed, and aspirin, clopidogrel, and enoxaparin were initiated. A coronary angiography (Figure 2, Video 1) was undertaken and revealed an anomalous origin of the left main coronary artery (LMCA) arising from the right coronary artery (RCA) and an interatrial course, leading to compression of the proximal segment of the LMCA. To further evaluate the CAA and determine the treatment, a coronary computed tomography angiography (CCTA) was performed (Figure 3). It confirmed the abnormal origin of the LMCA from the RCA, with a malignant trajectory of the LMCA between the ascending aorta and the pulmonary trunk. In addition, the LMCA had an intramyocardial pathway and origins in 2 branches, the left circumflex and the ramus intermedius. The anomaly was managed surgically with coronary artery bypass grafting (CABG). A median sternotomy was performed, followed by anterior pericardiectomy. The heart had a normal aspect and the LMCA was found to rise from the RCA, with an interarterial course, passing between the aorta and the pulmonary trunk. Dissection of the left internal thoracic artery was executed, followed by aorta and right atrium cannulation for cardiopulmonary bypass. An aortic cross-clamp was applied and cardiac arrest was induced by Custodiol cardioplegic solution. A cross-section of the pulmonary artery was performed to visualize the entire LMCA trajectory. It had an extramural and intramyocardial pathway. Three branches rose from the LMCA: the left circumflex, the ramus intermedius, and the left anterior descending artery. Importantly, the left anterior descending artery was hypoplastic and only 1 mm in diameter. Thus, CABG was performed with the left internal thoracic artery grafted to the ramus intermedius. Ligation of the LMCA was performed. An end-to-end pulmonary artery suture was executed, after which the air was removed from the heart cavities, recovering the heartbeat. Cross-clamping time was 37 min and the patient was weaned from cardiopulmonary bypass after 50 min.
Postoperative hemodynamics including blood pressure and cardiac output were stable, and no ischemic changes were observed. Enhanced Recovery After Surgery (ERAS) protocols were used for the patient, and he was discharged 3 days after CABG without systolic dysfunction. At the 1-year follow-up, the patient was asymptomatic, with a normal nuclear stress test (Figure 4).
Discussion
Congenital CAAs are rare abnormalities in the origin, course, or structure of these arteries. CAAs have a wide reported incidence in the population undergoing coronary angiography procedures [1-3], and owing to the association of CAAs with ischemia, arrhythmias, and sudden death, they have been increasingly evaluated in case reports and small case series [5,6].
There are several classification schemes for CAAs, and the following classification based on hemodynamic significance has recently been suggested: (1) hemodynamically significant anomalies, which may be associated with shunting, ischemia, or sudden death, and (2) anomalies that are usually not hemodynamically significant (Table 1) [7]. One of the rarest CAAs is the entire LMCA arising from the right sinus of Valsalva, with a reported incidence of 0.017% to 0.15% [1,8]. In such an anomaly, 4 variants of the arterial pathway are possible: (1) an anterior course, (2) between the ascending aorta and the pulmonary trunk, (3) through the supraventricular crest portion of the septum, and (4) a posterior course [9]. In our case, the LMCA arising from the RCA with an interarterial course was detected and was classified as hemodynamically significant. This subtype has the worst prognosis because the LMCA passes between the aorta and the pulmonary artery and it is associated with myocardial ischemia and sudden death, especially in young adults and athletes [3].
Most CAAs are asymptomatic and are usually detected incidentally during angiography. When CAAs are symptomatic, the modes of presentation include episodic chest pain, syncope, dyspnea, heart failure, ventricular arrhythmias, acute coronary syndrome, and sudden death. The symptoms are usually associated with the anomalous trajectory due to the coronary artery originating from the opposite sinus [10]. Of note, data from other case series show that a CAA presenting with acute coronary syndrome, such as in our patient, is a rare finding and is more frequently associated with the malignant trajectory of the LMCA between the ascending aorta and the pulmonary trunk. Approximately half of the patients with this anomaly experience fatal events before 20 years of age [11]. The mechanisms responsible for ischemia in this variant include a smaller size and a slit-like opening of the anomalous coronary artery ostium, an intramural course, and the expansion of great vessels during exercise, which can dynamically occlude the LMCA [12,13]. Similarly, some authors suggest that anomalous pathways may result in endothelial damage and dysfunction leading to coronary artery spasm contributing to other mechanisms [13].
The management of patients with suspected CAA is controversial, and it is crucial to determine the exact anatomical features of the anomalous artery and then identify the proper treatment. Coronary angiography and CCTA provide important concurrent information on coronary anatomical findings. Importantly, given that coronary angiography provides only 2-dimensional views of a vessel’s complex 3-dimensional path, the exact anatomic course of the anomalous vessel may be difficult to determine [14,15]. Therefore, some authors advocate using CCTA as the first-line investigation when CAAs are suspected, so the exact position and course of the anomalous artery can be viewed with regard to the aortic root and the pulmonary artery [10,16].
Once the diagnosis has been made, the next step is to decide on the management of the CAA, in view of the absence of official guidelines addressing the optimal approach [17]. The decision should be tailored for the individual based on the type of the anomaly. Patients with an anomalous origin of a coronary artery from the opposite sinus should first be prevented from participating in competitive sports because of the potential risk of sudden death [10]. In symptomatic patients with a CAA, surgical repair has generally been the standard of practice [18,19]. The goal of surgery is to limit the risk of myocardial ischemia.
The surgical techniques used to treat CAAs have advanced over the years. Currently, 3 surgical procedures are used: unroofing, reimplantation of the coronary artery, and CABG (Table 2). The line of incision for unroofing an intramural LMCA is indicated for vessels with an extensive intramural course; reimplantation involves the direct placement of the coronary artery in the correct sinus of Valsalva with the native vessel or grafting material; and CABG involves using the internal mammary artery, or vein grafts, as conduits to the anomalous artery. It has been argued that reimplantation may be risky, especially when dissecting and relocating this pathway with regard to various structures nearby. Therefore, CABG has been preferred in recent years [20–24]. In the current case, CABG was performed with an excellent clinical course and midterm follow-up. A review of the literature supports our aggressive approach, given that our patient presented with a myocardial infarction and had a potentially life-threatening CAA and the midterm follow-up showed good clinical outcomes [23,25]. Likewise, according to the most recent European Society of Cardiology Guidelines for the management of adult congenital heart disease, surgery is recommended for the anomalous aortic origin of a coronary artery in symptomatic patients who present evidence of stress-induced myocardial ischemia in a matching territory or high-risk anatomy, such as our case [26].
Conclusions
CAAs are uncommon findings but can be of significant clinical importance. Most CAAs are benign and not hemodynamically significant; however, some are potentially severe and can lead to myocardial ischemia and even death. The current case presented an unusual form of coronary artery malformation. Furthermore, it had a combination of different anomalies and initially presented as acute coronary syndrome. Due to the severity of the patient’s anomaly and the evidence of myocardial ischemia, the surgical decision was to proceed with CABG, as recommended by guidelines, to avoid the risk of sudden cardiac death. The surgery was successfully performed with a single-vessel coronary bypass. There is considerable variation in treating an atypical coronary artery, reinforcing the need for further investigation into a more standardized approach. This report confirms the need for angiography and CCTA in establishing diagnosis and treatment.
Figures
References:
1.. Angelini P, Villason S, Chan AV, Diez G, Normal and anomalous coronary ar-teries in humans: Coronary artery anomalies: A comprehensive approach, 1999; 27-150, Baltimore, MD, Lippincott Williams & Wilkins
2.. Zeppilli P, dello Russo A, Santini C, In vivo detection of coronary artery anomalies in asymptomatic athletes by echocardiographic screening: Chest, 1998; 114(1); 89-93
3.. Taylor AJ, Rogan KM, Virmani R, Sudden cardiac death associated with isolated congenital coronary artery anomalies: J Am Coll Cardiol, 1992; 20(3); 640-47
4.. Basso DC, Thiene G, Congenital coronary artery anomalies at risk of myocardial ischaemia and sudden death: Eur Cardiol, 2005; 1(1); 1-5
5.. Basso C, Maron BJ, Corrado D, Thiene G, Clinical profile of congenital coronary artery anomalies with origin from the wrong aortic sinus leading to sudden death in young competitive athletes: J Am Coll Cardiol, 2000; 35(6); 1493-501
6.. Frescura C, Basso C, Thiene G, Anomalous origin of coronary arteries and risk of sudden death: A study based on an autopsy population of congenital heart disease: Hum Pathol, 1998; 29(7); 689-95
7.. Shriki JE, Shinbane JS, Rashid MA, Identifying, characterizing, and classifying congenital anomalies of the coronary arteries: Radiographics, 2012; 32(2); 453-68
8.. Yamanaka O, Hobbs RE, Coronary artery anomalies in 126,595 patients undergoing coronary arteriography: Cathet Cardiovasc Diagn, 1990; 21(1); 28-40
9.. Roberts WC, Shirani J, The four subtypes of anomalous origin of the left main coronary artery from the right aortic sinus (or from the right coronary artery): Am J Cardiol, 1992; 70(1); 119-21
10.. Ali M, Hanley A, McFadden EP, Vaughan CJ, Coronary artery anomalies: A practical approach to diagnosis and management: Heart Asia, 2011; 3(1); 8-12
11.. Kim D, Jeong MH, Lee KH, Successful primary percutaneous coronary intervention in a patient with acute myocardial infarction and single coronary artery ostium: Korean Circ J, 2012; 42(4); 284-87
12.. Cheitlin MD, De Castro CM, McAllister HA, Sudden death as a complication of anomalous left coronary origin from the anterior sinus of Valsalva, a not-so-minor congenital anomaly: Circulation, 1974; 50(4); 780-87
13.. Barriales-Villa R, Morís de la Tassa C, [Congenital coronary artery anomalies with origin in the contralateral sinus of Valsalva: Which approach should we take?]: Rev Esp Cardiol, 2006; 59(4); 360-70 [in Spanish]
14.. Basso C, Corrado D, Thiene G, Congenital coronary artery anomalies as an important cause of sudden death in the young: Cardiol Rev, 2001; 9(6); 312-17
15.. Serota H, Barth CW, Seuc CA, Rapid identification of the course of anomalous coronary arteries in adults: The “dot and eye” method: Am J Cardiol, 1990; 65(13); 891-98
16.. Khouzam R, Marshall T, Lowell D, Siler JR, Left coronary artery originating from right sinus of Valsalva with diagnosis confirmed by CT – a case report: Angiology, 2003; 54(4); 499-502
17.. Nesheiwat Z, Eid J, Soni R, A single, shared origin for all three coronary arteries from the right coronary cusp: A case report: J Med Case Rep, 2020; 14(1); 94
18.. Frommelt PC, Frommelt MA, Tweddell JS, Jaquiss RD, Prospective echocardiographic diagnosis and surgical repair of anomalous origin of a coronary artery from the opposite sinus with an interarterial course: J Am Coll Cardiol, 2003; 42(1); 148-54
19.. Gersony WM, Management of anomalous coronary artery from the contra-lateral coronary sinus: J Am Coll Cardiol, 2007; 50(21); 2083-84
20.. Wolf T, Bolotin G, Ammar R, Uretzky G, Anomalous origin of the left main coronary artery: Anatomical correction and concomitant LIMA-to-LAD grafting: Eur J Cardiothorac Surg, 1999; 15(2); 209-12
21.. Van Son JA, Haas GS, Anomalous origin of left main coronary artery from right sinus of Valsalva: Modified surgical treatment to avoid neo-coronary ostial stenosis: Eur J Cardiothorac Surg, 1996; 10(6); 467-69
22.. Cohen AJ, Grishkin BA, Helsel RA, Head HD, Surgical therapy in the management of coronary anomalies: Emphasis on utility of internal mammary artery grafts: Ann Thorac Surg, 1989; 47(4); 630-37
23.. Reul RM, Cooley DA, Hallman GL, Reul GJ, Surgical treatment of coronary artery anomalies: Report of a 37 1/2-year experience at the Texas Heart Institute: Tex Heart Inst J, 2002; 29(4); 299-307
24.. Schubert SA, Kron IL, Surgical unroofing for anomalous aortic origin of coronary arteries: Oper Tech Thorac Cardiovasc Surg, 2016; 21; 162-77
25.. Khan MS, Idris O, Shah J, Anomalous origin of left main coronary artery from the right sinus of Valsalva: A case series-based review: Cureus, 2020; 12(4); e7777
26.. Baumgartner H, De Backer J, Babu-Narayan SV, 2020 ESC Guidelines for the management of adult congenital heart disease: Eur Heart J, 2021; 42(6); 563-645
27.. Turner II, Turek JW, Jaggers J, Anomalous aortic origin of a coronary artery: Preoperative diagnosis and surgical planning: World J Pediatr Congenit Heart Surg, 2011; 2(3); 340-45
28.. Fabozzo A, DiOrio M, Newburger JW, Anomalous aortic origin of coronary arteries: A single-center experience: Semin Thorac Cardiovasc Surg, 2016; 28(4); 791-800
29.. Nees SN, Flyer JN, Chelliah A, Patients with anomalous aortic origin of the coronary artery remain at risk after surgical repair: J Thorac Cardiovasc Surg, 2018; 155(6); 2554-64e3
30.. Mainwaring RD, Murphy DJ, Rogers IS, Surgical repair of 115 patients with anomalous aortic origin of a coronary artery from a single institution: World J Pediatr Congenit Heart Surg, 2016; 7(3); 353-59
31.. Krasuski RA, Magyar D, Hart S, Long-term outcome and impact of surgery on adults with coronary arteries originating from the opposite coronary cusp: Circulation, 2011; 123(2); 154-62
Figures
Tables
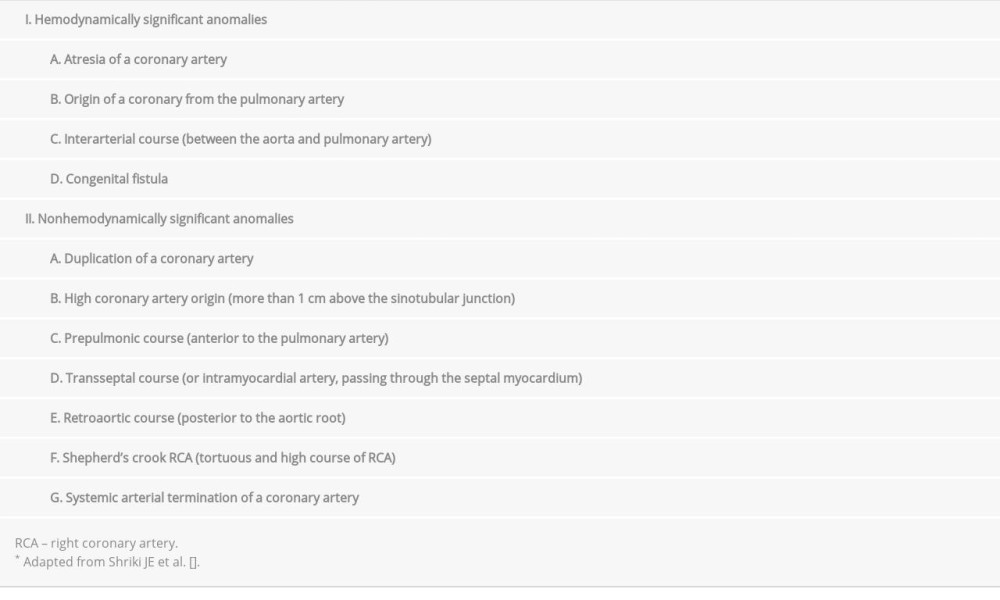 Table 1.. Classification scheme of coronary artery anomalies*.
Table 1.. Classification scheme of coronary artery anomalies*.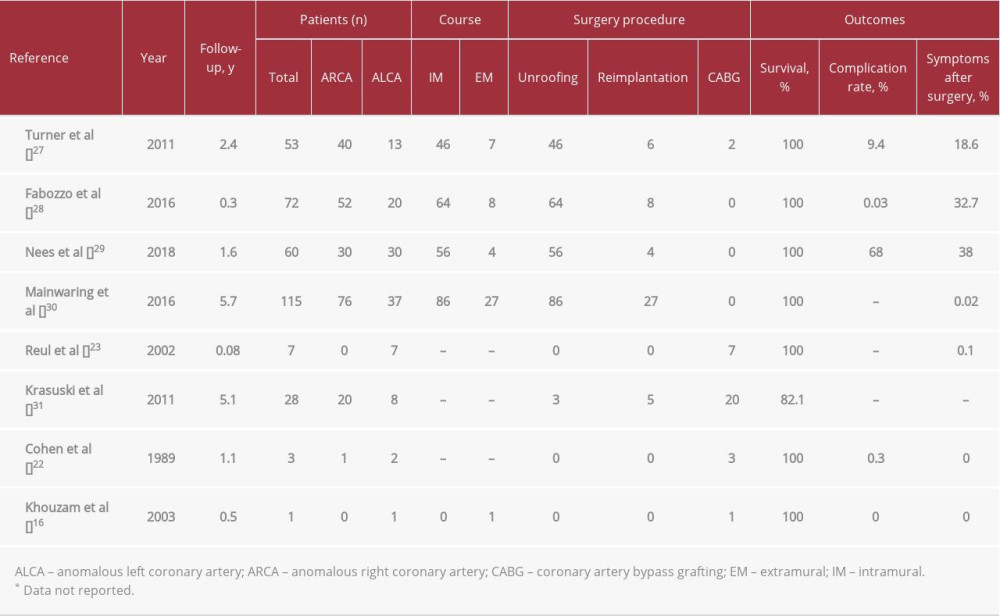 Table 2.. Literature review of coronary artery origin anomalies, management, and outcomes.
Table 2.. Literature review of coronary artery origin anomalies, management, and outcomes.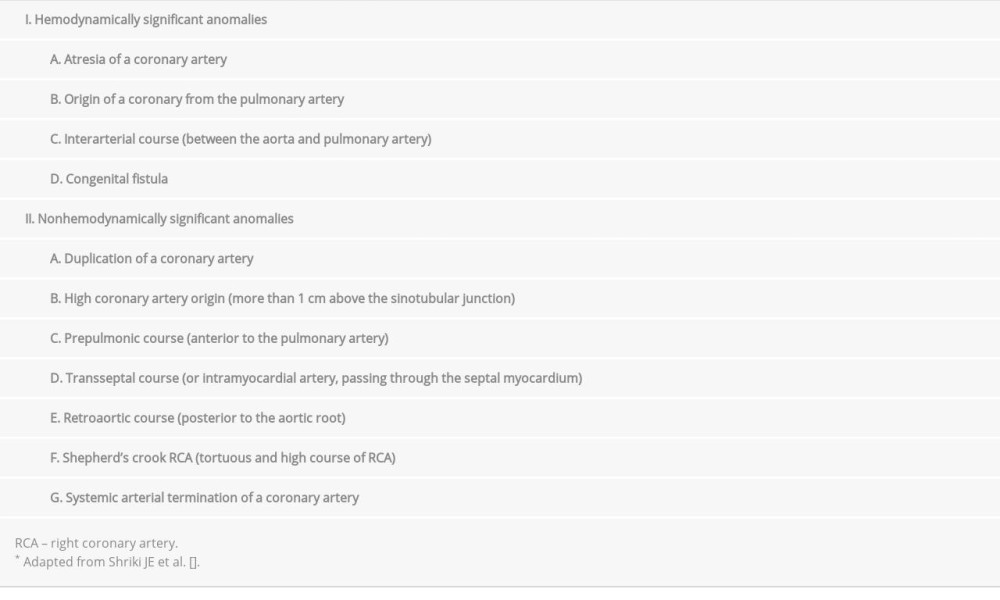 Table 1.. Classification scheme of coronary artery anomalies*.
Table 1.. Classification scheme of coronary artery anomalies*.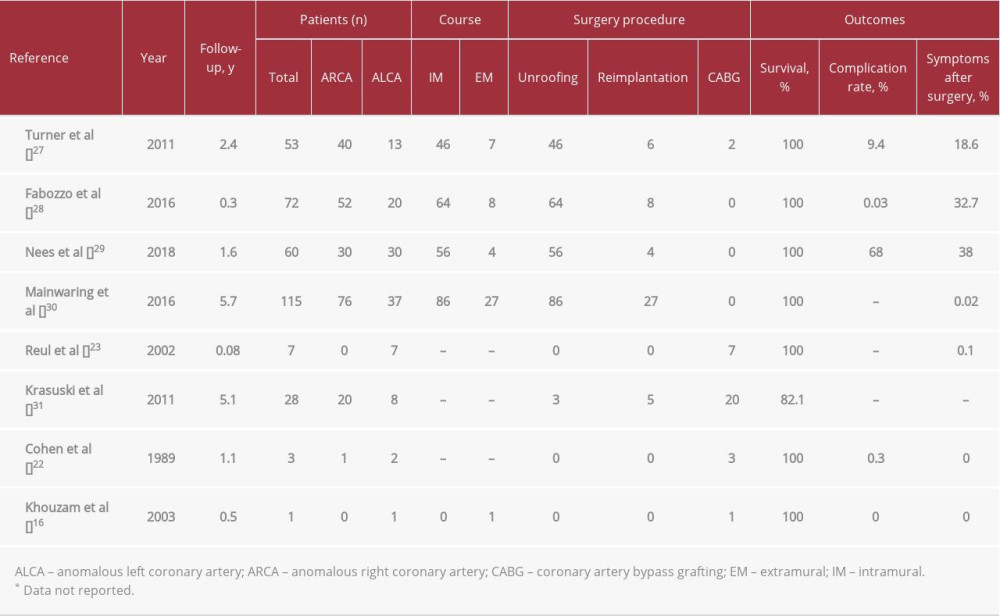 Table 2.. Literature review of coronary artery origin anomalies, management, and outcomes.
Table 2.. Literature review of coronary artery origin anomalies, management, and outcomes. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








