12 October 2021: Articles 
A 7-Year-Old Boy and a 14-Year-Old Girl Initially Diagnosed with Toxic Shock Syndrome and Tested Positive for SARS-CoV-2 Infection, Supporting a Diagnosis of Multisystem Inflammatory Syndrome in Children (MIS-C)
Unusual clinical course, Challenging differential diagnosis, Management of emergency care
Salvatore Giordano1ABCD, Maria Concetta Failla1ABD, Maria Grazia Li Cavoli1ABD, Domenico Romano2BEF, Veronica Vanella2BE, Chiara Caruso2B, Ilenia Chillura2B, Maria Cristina Maggio2ABCDEF*DOI: 10.12659/AJCR.931570
Am J Case Rep 2021; 22:e931570
Abstract
BACKGROUND: Multisystem inflammatory syndrome in children (MIS-C) has recently been described in children infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This report describes 2 children with MIS-C who were initially diagnosed with toxic shock syndrome but who tested positive for SARS-CoV-2 infection on reverse transcription-polymerase chain reaction, supporting the diagnosis of MIS-C.
CASE REPORT: Case 1. A 7-year-old boy with fever, cough, and dyspnea was treated with oxygen, intravenous immunoglobulin (IVIG) infusion, and methylprednisolone and showed a worsening of clinical conditions, persistent fever, hypotension, and hematological parameters compatible with macrophage activation syndrome (MAS). Three intravenous boluses of methylprednisolone (30 mg/kg/day) were followed by a progressive resolution. Case 2. A 14-year-old girl with syncope, fever, diarrhea, oliguria, and increased creatinine levels required fluid infusion and correction of electrolyte imbalance. The increase of creatine phosphokinase (CPK), myoglobin, troponin, and creatine kinase-MB (CK-MB) was associated with grade I atrioventricular block and pericardial effusion. The patient showed myositis and severe muscular weakness, with hematological parameters compatible with MIS-C. She started IVIG and 3 intravenous boluses of methylprednisolone. However, bradycardia, tachypnea, severe hypotension, loss of consciousness, oliguria, bilateral ground-glass pneumonia, bilateral pleural, and peritoneal effusion, in the absence of thromboembolism, required treatment with furosemide, albumin, and enoxaparin, and was followed by a prompt resolution.
CONCLUSIONS: These 2 pediatric cases highlight the importance of SARS-CoV-2 testing in all patients with acute symptoms and signs of infection during the COVID-19 pandemic. As new variants of SARS-CoV-2 emerge, cases of MIS-C can become more prevalent, and pediatricians should be aware of diagnostic and management guidelines.
Keywords: Immunoglobulins, Intravenous, Mucocutaneous Lymph Node Syndrome, Pediatric Multisystem Inflammatory Disease, COVID-19 Related, Adolescent, COVID-19, COVID-19 Testing, Child, Female, Humans, Pandemics, SARS-CoV-2, Shock, Septic, Systemic Inflammatory Response Syndrome
Background
The rapid spread of COVID-19 caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) led to a global pandemic, with infected individuals of all ages residing in almost every country in the world. The pediatric population appears to be affected in much smaller proportions than adults, with only 2% of cases being described in patients younger than 20 years old. In an epidemiological report, authors described COVID-19 cases in the pediatric population, with 90% of patients defined as asymptomatic, mild, or moderate [1].
However, in April 2020, there was an emergence of a new multisystem inflammatory syndrome affecting children in relation to COVID-19 called “multisystem inflammatory syndrome in children” (MIS-C) or “pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2”. Comparable to clinical manifestations of severe COVID-19 in adult patients, MIS-C is characterized by hyperinflammation, secondary to cytokine storm. The predominant clinical findings are persistent fever, oral mucosal changes, conjunctivitis, abdominal pain, vomiting, diarrhea, respiratory symptoms, myocar-dial dysfunction, and cardiogenic shock with left ventricular dysfunction. Most of these patients required admission to pediatric intensive care units, necessitating input from specialists, including cardiologists, rheumatologists, immunologists, and infectious disease specialists. Patients with MIS-C exhibit symptoms that are like those of diseases such as Kawasaki disease (KD) and streptococcal and staphylococcal toxic shock syndrome (TSS) [2].
In fact, the overlapping of clinical findings of MIS-C and KD guided researchers to consider the 2 conditions as the same disease, with a specific documented trigger in MIS-C, which was otherwise supported by the evidence of the efficacy of anakinra in patients with a severe outcome, as in non-responders or in patients with high-risk of KD [3,4]. However, following observations, MIS-C was differentiated from KD on the bases of relevant epidemiological, clinical, biochemical, and imaging data. In fact, patients with MIS-C present symptoms strongly linked to TSS, typically caused by bacterial superantigens that trigger an amplification of the cytotoxic adaptive immune response. The SARS-CoV-2 spike (S) glycoprotein, in fact, shows a region at the C-terminal end whose sequence and structure match those of the bacterial superantigen
It was recently described that the immune response in patients with MIS-C as well as that in adult patients with severe COVID-19 are induced by superantigen activation.
Superantigens not only massively activate T cells but can also dysregulate B cells with a secondary autoimmune response and secretion of autoantibodies.
In Sicily, the first wave of COVID-19 showed a low epidemic impact in our pediatric population, while the second wave had a higher impact on clinical presentation of COVID-19 in children and a significantly higher severe outcome in patients with MIS-C, frequently showing a life-threatening progression.
Therefore, this report describes 2 cases of MIS-C: a 7-year-old boy and a 14-year-old girl who were initially diagnosed with TSS but who tested positive for SARS-CoV-2 infection by reverse transcription-polymerase chain reaction (RT-PCR), which supported a diagnosis of MIS-C.
Case Reports
CASE 1. A 7-YEAR-OLD BOY WHO WAS PREVIOUSLY HEALTHY AND FULLY IMMUNIZED:
At the end of August 2020, the patient returned to Italy from Romania, and he and his parents underwent a nasopharyngeal swab for SARS-CoV-2 by PCR testing, and each had a positive result. The family was subjected to quarantine, and the boy was asymptomatic and in a good general clinical condition for 14 days. At 17 days after the detection of the positive swab test, he had fever, latero-cervical lymphadenopathy, and cough. At home, he was treated with paracetamol and azithromycin without improvement. He was transported to the hospital for the worsening of his clinical condition.
When he arrived at the Infectious Diseases Unit, he had a high fever (39.7°C), latero-cervical lymphadenopathy, heart rate of 140 beats/min, blood pressure of 100/65 mmHg, tachypnea (respiratory rate of 45 breath/min), dyspnea, mild subcostal retractions, oxygen saturation of 94%, and pathological breathing sounds on chest auscultation (Table 1). Laboratory testing revealed neutrophilic leukocytosis, normocytic anemia, low platelet count, markedly elevated C-reactive protein (CRP) level of 27.99 mg/dL, procalcitonin of 176.31 ng/L, and increased levels of D-dimer. He had hyponatremia and increased levels of transaminase, gamma GT, lipase, and pancreatic amylase. The other parameters were in the reference range (Table 2). The nasopharyngeal swab for SARS-CoV-2, diagnosed by RTPCR on 2 molecular targets (E, N2) (Xpert Xpress SARS-CoV-2, Cepheid, Maurens-Scopont, France) was positive in 2 different swabs and confirmed SARS-CoV-2 infection. The chest computed tomography (CT) imaging showed signs of bilateral interstitial pneumonia with a ground-glass appearance, which was associated with areas of consolidation, for likely bacterial overlap and bilateral pleural effusion. The echocardiogram was normal, without any evidence of coronary dilation, aneurysm, or pericardial effusion, and showed normal valvular and ventricular contractility patterns.
The clinical and laboratory pictures were compatible with MIS-C, according to Center for Disease Control (CDC) criteria for the case definition of MIS-C [2]: fever ≥38.0°C for >24 h; severe illness (hospitalization); ≥2 organ systems involved; laboratory evidence of inflammation; link to SARS-CoV-2; and laboratory evidence of inflammation, including an increase of CRP, erythrocyte sedimentation rate (ESR), procalcitonin, and D-dimer and neutrophilia, lymphopenia, and hypoalbuminemia. He was treated with oxygen therapy, intravenous immunoglobulin (IVIG) infusion (2 g/kg), the dosage employed for KD and MIS-C, and intravenous steroids (methylpredniso-lone 2 mg/kg/day). In a few days, he showed the worsening of his general condition, with persistent fever, and low blood pressure (89/33 mmHg) and hematological parameters compatible with macrophage activation syndrome (MAS) (hyper-ferritinemia, hypertriglyceridemia, hypertransaminasemia, hypoalbuminemia, thrombocytopenia, and hypofibrinogenemia). Furthermore, he showed increased levels of pancreatic amylase and lipase.
Epstein-Barr virus, cytomegalovirus, and parvovirus infection were excluded by PCR testing [5].
Intravenous boluses of methylprednisolone (30 mg/kg/day) were administered for 3 consecutive days with albumin (1 g/kg), followed by defervescence, progressive resolution of tachypnea and dyspnea, normalization of blood pressure and diuresis, and the end of oxygen therapy. Lung ultrasound demonstrated the disappearance of the pleural effusion. He showed the reduction of inflammation, cytolysis, and cholestasis indexes and the normalization of coagulation, ferritin levels, and pancreatic enzymes (Table 2). In consideration of these parameters, steroid decalage was started and low-dose aspirin (5 mg/ kg/day) was added. At discharge, 35 days after the first positive swab for SARS-CoV-2, the swab test was negative. He was discharged, and the cardiologic follow-up documented normal parameters in the following months.
CASE 2. A 14-YEAR-OLD GIRL WITHOUT ANY CLINICAL RECORDS OF DISEASE:
The patient was taken to the Pediatric Emergency Department of our hospital for syncope. In a few hours, the patient had fever, tachycardia, and pharynx hyperemia, with normal neurological examination and respiratory parameters (Table 3). She was admitted to the Infectious Diseases Unit and the nasopharyngeal swab for SARS-CoV-2, diagnosed by RT-PCR diagnostic testing on 2 molecular targets (E, N2) (Xpert Xpress), was positive in 3 different swabs, confirming SARS-CoV-2 infection. In the first days after admission, diarrhea and progressive oliguria were found, with increased serum creatinine (1.29 mg/dL). Fluid infusion and correction of electrolyte alterations were initiated. The increase of myocytolysis indices (CPK, lactate dehydrogenase) and myocardial markers, namely myoglobin of 1678 ng/mL, troponin of 246 ng/L (reference value <14), and CK-MB of 11.40 µg/L (reference value 0–4.88) required serial ECGs and cardiac ultrasounds, which showed an atrioventricular block of grade I and minimal pericardial effusion.
In a few days, clinical conditions worsened, and the patient showed the presence of myositis and severe muscular weakness with the increase of the following inflammatory parameters: PCR of 13.25 mg/dL, procalcitonin of 3.58 µg/L, ferritin of 815.7 ng/mL, creatine phosphokinase of 12 542, albumin of 2.4 g/L, and hypertriglyceridemia, in association with thrombocytopenia (90 000/mm3).
The clinical and laboratory pictures in this patient were also compatible with MIS-C, according to the CDC criteria for the case definition of MIS-C [2]: fever ≥38.0°C for >24 h; severe illness (the patient was hospitalized); ≥2 organ systems involved; laboratory evidence of inflammation; link to SARS-CoV-2; laboratory evidence of inflammation including the following: increase of CRP, ESR, procalcitonin, and D-dimer and neutrophilia, lymphopenia, and hypoalbuminemia.
On suspicion of MIS-C, she started therapy with IVIG infusion (2 g/kg) and intravenous boluses of methylprednisolone (30 mg/kg/day) for 3 consecutive days. Despite this, for the sudden onset of bradycardia, tachypnea, severe hypotension, amaurosis, loss of consciousness, and oliguria, the pediatric intensive consultant, pediatric cardiologist, and pediatric nephrologist were consulted. On the suspicion of pulmonary embolism, a total-body CT angiogram was performed, which had findings of bilateral ground-glass pneumonia, bilateral pleural effusion, and peritoneal effusion in the absence of thromboembolism. Treatment with furosemide, albumin, and anti-thrombotic prophylaxis with enoxaparin was started.
She showed a prompt and significant clinical response to the treatment, with gradual and progressive normalization of vital parameters, blood chemistry tests, inflammation indices, and cardiovascular function. The treatment with enoxaparin and albumin was discontinued and prednisolone was gradually tapered (Table 4). At discharge, 11 days after the first nasopharyngeal swab, the molecular test for SARS-CoV-2 of the swab was negative.
Discussion
In children, SARS-CoV-2 infection usually causes mild symptoms, but a small subset of children and adolescents can manifest an emerging clinical presentation. In April 2020, the first manifestations resembling KD or TSS occurred in children 2 to 6 weeks after SARS-CoV-2 infection or in children with contact with infected patients; thereafter, the CDC criteria for the case definition of MIS-C were identified [2]. From the above case reports, we can learn that the appropriate management of patients with MIS-C is determined by the evaluation of the severity of the following parameters: severity of the clinical picture, risk of complications, and adequate follow-up. The clinical presentation is heterogeneous and includes the signs of classical KD (bilateral conjunctival injection, changes in the lips and oral cavity, cervical lymphadenopathy, extremity changes, and polymorphous rash), altered vital signs (tachycardia and/or tachypnea), shock, respiratory distress syndrome, cardiac involvement (arrhythmias, elevation of troponin and/ or brain natriuretic peptide (BNP) values, aneurysm or coronary artery stenosis, and left ventricular failure), neurological signs (depressed mood, seizures, and abnormal neurological objectivity), vomiting or acute abdomen, clinical or laboratory signs of dehydration, acute renal failure, acute liver failure, and coagulopathy.
Furthermore, myalgia is described as a common symptom of COVID-19, after the most common symptoms of fever, cough, and sore throat, and its extent can be related to the severity of SARS-CoV-2 infection. Few patients showed muscle weakness and increased CPK accompanied by elevated levels of CRP and ESR. Adult patients with myositis and/or rhabdomyolysis developed a severe respiratory outcome associated with COVID-19. Treatment with IVIG and/or steroids was useful in most of these patients [6]. Patient management varies according to the severity of the clinical picture at hospitalization; in fact, about 60% to 80% of patients with MIS-C required an intensive care regimen in the Pediatric Intensive Care Unit. The management of these patients involves the collaboration of various professional specialists including the pediatric infectious diseases specialist, pediatric rheumatologist, pediatric pulmonologist, pediatric intensive care physician, and pediatric cardiologist. The treatment varies according to the patient’s clinical presentation. It must be considered that these different manifestations can occur at different times of the disease or can overlap. Patients presenting in shock must be resuscitated according to latest protocols. The immunomodulatory therapeutic approach employed for TSS and refractory and high-risk KD, such as IVIG and steroids, can also be effective for MIS-C. Indeed, most patients with MIS-C respond well to aspirin (5 mg/kg/day) and IVIG, without steroids.
The SARS-CoV-2 spike protein shows a high-affinity superantigen-like sequence motif near the S1/S2 cleavage site. This region shows a high affinity to bind to T-cell receptors. This region (containing the superantigen-like motif) is very similar in sequence and 3-dimensional structure to a fragment of the superantigen SEB, which is known to link the T-cell receptors and CD28. The SEB activates and induces a high percentage of T-cell activation and proliferation, resulting in a cytokine storm with a proinflammatory profile, which is typical of TSS, KD with MAS, and severe COVID-19.
IVIG can neutralize in vitro T-cell activation by staphylococcal and streptococcal superantigens, such as SEB. As a result of the structural similarities between SEB and the SARS-CoV-2 spike superantigen-like sequence motif, it is possible that IVIG contains antibodies that neutralize SEB and cross-react with the SARS-CoV-2 spike, which in part explains the beneficial response to IVIG in MIS-C [1]. Furthermore, specific human leukocyte antigen types might enable superantigen binding and predispose patients to TSS or MIS-C.
Our patients, as was described in other patients with MIS-C, showed hypotension without signs of cardiac failure that was secondary to cytokine storm and induced vasodilatory shock. These patients do not respond to volume expansion; however, in these children, treatment with immunomodulatory drugs and epinephrine or norepinephrine is indicated. In patients with left ventricular insufficiency, adding milrinone to epinephrine is recommended. These patients require continuous cardiac monitoring. In patients with a KD-like presentation, it is recommended to start the standard therapy for KD [7] with IVIG of 2 g/kg and an antiplatelet dosage of aspirin. Glucocorticoids are useful and, when there are signs of coronary inflammation and in rapidly evolutive patients who are refractory to first-line therapy with IVIG (with or without the addition of corticosteroids), it is advisable to use anakinra or canakinumab [2,3,8]. Patients mimicking TSS or septic shock syndrome should be administered antibiotic therapy with ceftriaxone combined with vancomycin or, as an alternative, cefazolin plus piperacillin-tazobactam if the patient has an acute renal insufficiency. Antiviral therapy in children is rarely used. In fact, MIS-C can occur in a convalescent phase of the disease, and the effectiveness of current antiviral therapies is still unknown. The use of IVIG is also recommended in patients with heart involvement (left ventricular insufficiency, arrhythmias, coronary damage, troponin, and/or BNP increase) at the standard dosage of 2 g/kg [9]. In patients with severe left ventricular failure who cannot tolerate the IVIG loading volume, the dose can be divided over 3 to 5 days. The use of glucocorticoids in patients with MIS-C is still being discussed, and the dosage is not standardized. However, it is reasonable to use glucocorticoids in cases of resistance to IVIG or in patients with shock, coronary aneurysms, high levels of inflammation indices (CRP, ferritin, D-dimer, interleukin [IL]-6), and MAS. The dosage varies according to the severity of the clinical picture. It is suitable to start with methylprednisolone at a dosage of 2 mg/kg and to make a therapeutic switch with prednisone or prednisolone until day 7 or until CRP levels normalize, and then wean over 2 to 3 weeks; if the patient has a very compromised life-threatening state, or in cases of patients who fulfill the criteria for MAS, it is advisable to start boluses of methylprednisolone of 30 mg/kg (max 1000 mg/day) in a single administration for 3 consecutive days. Other effective drugs are monoclonal antibodies: anti-IL-1 receptor monoclonal antibodies (anakinra), anti-IL-1β (canakinumab) [2,8], and anti-IL-6 (tocilizumab). The efficacy of these drugs in patients with MIS-C is still under discussion, but it is advisable to use them in patients who did not respond to first-step treatment and to a high dose of glucocorticoids such as rescue therapy, which is employed in patients with MAS or cytokine release syndrome that is unresponsive to standard therapies. It is advisable to consult a pediatric rheumatologist before using these drugs.
In our patients, satisfactory clinical and hematological results with steroids, IVIG, and enoxaparin did not require the use of monoclonal antibodies, which were used in other pediatric cases described in literature [10].
Patients with MIS-C have an increased risk of thromboembolic events secondary to a state of COVID-19-related hypercoagulability and organ dysfunction. It is therefore appropriate to evaluate the possibility of adding anticoagulant therapy on a case-by-case basis. In the 14-year-old girl described in our case 2, the suspicion of pulmonary embolism was not confirmed by CT; however, enoxaparin was started and resulted in a significant clinical improvement. Furthermore, the significant CPK increase with myositis and the severe muscular weakness in this patient were in part the consequence of viral infection, as has been reported in myositis secondary to SARS-CoV-2 infection. Among patients with myositis secondary to SARS-CoV-2 infection, myalgia has been reported in 11% to 50% of patients in different studies [11,12], and muscle weakness related to COVID-19 has been reported as well. However, the association of myositis and MIS-C is in line with the hyperinflamma-tory pattern typical of MIS-C and the strict similarity of MIS-C with KD and TSS [2].
Other studies have highlighted the possible link of myositis being a severe and atypical outcome of KD [13]. In addition, TSS is a possible cause of myositis, by way of superantigen activation, as was documented in cases of streptococcic infections [14].
The use of hyperimmune (convalescent) plasma and/or hyperimmune globulins is still controversial, as there are limited data on their use in adults, while they have not yet been used in the pediatric population.
Conclusions
The initial data on SARS-CoV-2 revealed that children have a low incidence of symptomatic infection. However, the significant incidence of MIS-C in the pediatric population after a significant delay from the first positive nasopharyngeal swab, suggests a delayed hyperimmune response to SARS-CoV-2 infection. The real incidence of MIS-C following an asymptomatic or mildly symptomatic infection is unknown; however, even if this condition affects only a small part of the pediatric population, it is a concern because these patients develop serious life-treating complications, such as shock-mimicking TSS [15,16].
Recent studies suggest IVIG plus high-dose steroid resistance in some cases of MIS-C, especially in children who were affected by shock, myositis, and MAS, thereby questioning the benefit of monoclonal antibodies, such as IL-6 or IL-1 blocking agents. Therefore, it is necessary to promptly diagnose MIS-C and start the appropriate therapy by bringing together a multi-specialistic team, as required in atypical and resistant cases of KD [17,18].
Further studies assessing the predisposing factors and the pathogenesis of MIS-C are required to avoid and treat this condition. These 2 pediatric cases have highlighted the importance of SARS-CoV-2 testing in all patients of any age who present with acute symptoms and signs of infection during the COVID-19 pandemic. As new variants of SARS-CoV-2 emerge, it is possible that cases of MIS-C will become more prevalent, and pediatricians should be aware of developments in diagnostic and management guidelines.
Tables
Table 1.. Case 1. Clinical findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.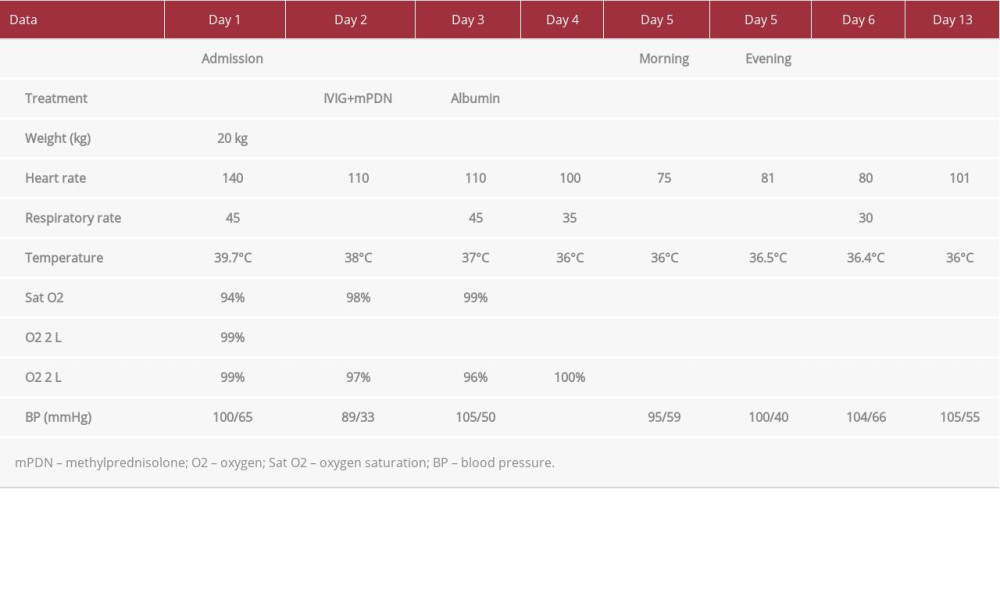 Table 2.. Case 1. Hematological findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 2.. Case 1. Hematological findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.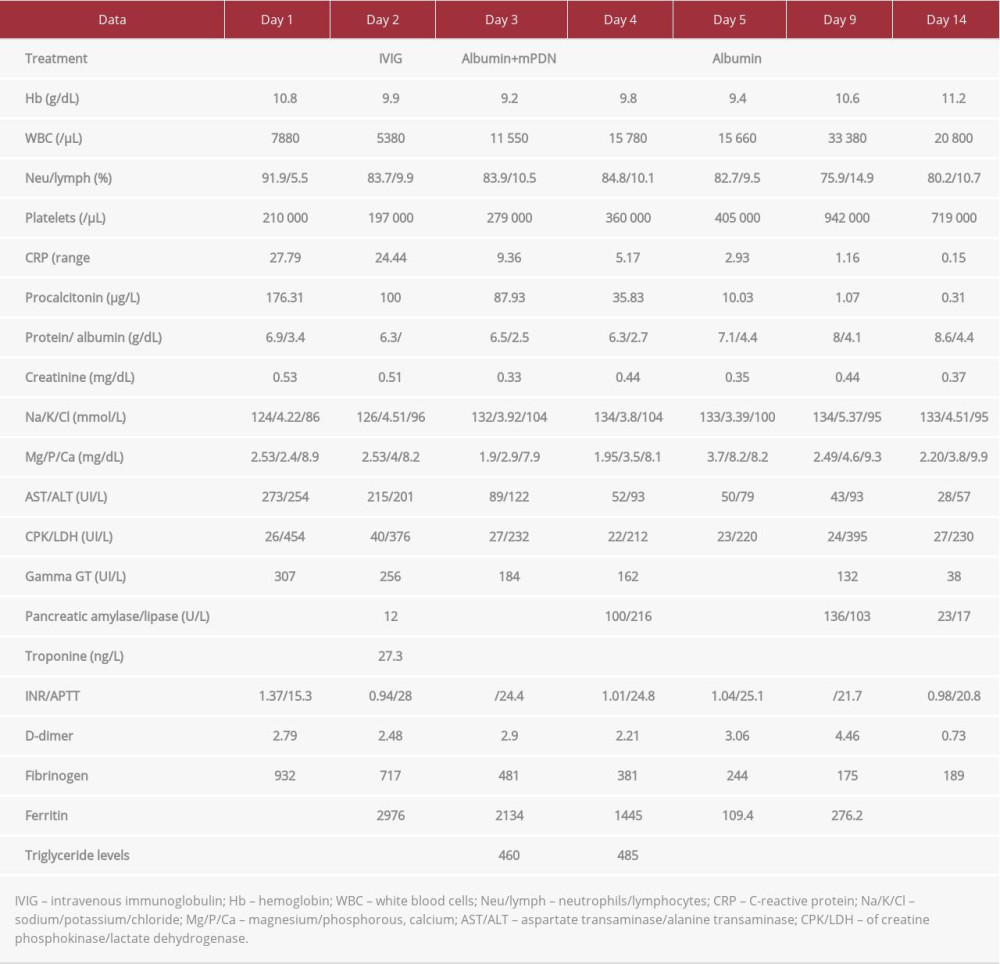 Table 3.. Case 2. Clinical findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 3.. Case 2. Clinical findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.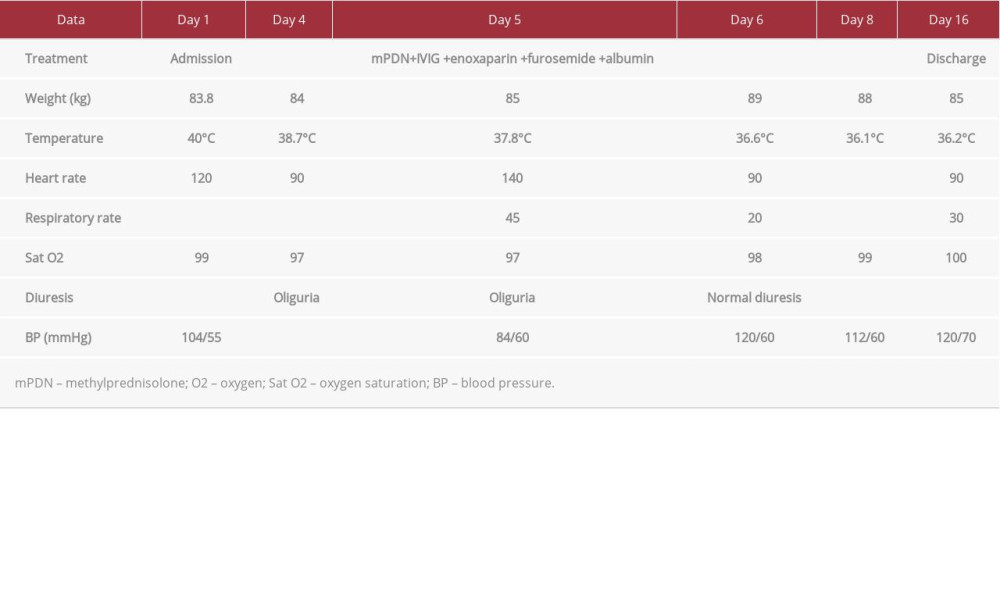 Table 4.. Case 2. Hematological findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 4.. Case 2. Hematological findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.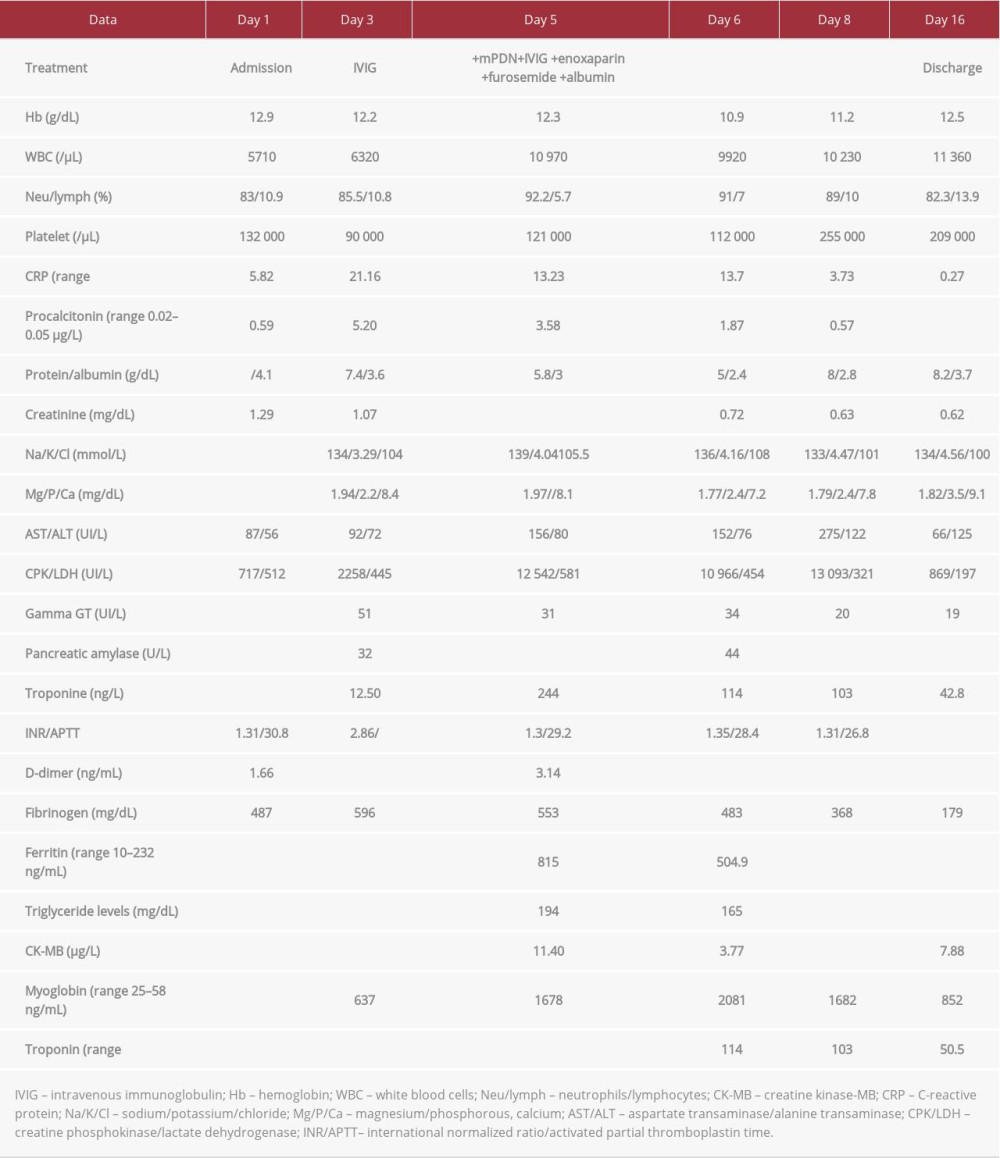
References:
1.. Noval Rivas M, Porritt RA, Cheng MH, COVID-19-associated multi-system inflammatory syndrome in children (MIS-C): A novel disease that mimics toxic shock syndrome-the superantigen hypothesis: J Allergy Clin Immunol, 2021; 147(1); 57-59
2.. Henderson LA, Canna SW, Friedman KG, American College of Rheumatology clinical guidance for multisystem inflammatory syndrome in children associated with SARS-CoV-2 and hyperinflammation in pediatric COVID-19: Version 1: Arthritis Rheumatol, 2020; 72; 1791
3.. Kone-Paut I, Cimaz R, Herberg J, The use of interleukin 1 receptor antagonist (anakinra) in Kawasaki disease: A retrospective cases series: Autoimmun Rev, 2018; 17(8); 768-74
4.. Maggio MC, Cimaz R, Alaimo A, Kawasaki disease triggered by parvovirus infection: An atypical case report of two siblings: J Med Case Rep, 2019; 13(1); 104
5.. Maggio MC, Liotta A, Cardella F, Corsello G, Stevens-Johnson syndrome and cholestatic hepatitis induced by acute Epstein-Barr virus infection: Eur J Gastroenterol Hepatol, 2011; 23(3); 289
6.. Paliwal VK, Garg RK, Gupta A, Neuromuscular presentations in patients with COVID-19: Neurol Sci, 2020; 41(11); 3039-56
7.. Marchesi A, Rigante D, Cimaz R, Revised recommendations of the Italian Society of Pediatrics about the general management of Kawasaki disease: Ital J Pediatr, 2021; 47(1); 16
8.. Cavalli G, Colafrancesco S, Emmi G, Interleukin 1α: A comprehensive review on the role of IL-1{α in the pathogenesis and targeted treatment of autoimmune and inflammatory diseases: Autoimmun Rev, 2021; 3; 102763
9.. Maggio MC, Corsello G, Prinzi E, Kawasaki disease in Sicily: Clinical description and markers of disease severity: Ital J Pediatr, 2016; 42(1); 92
10.. Fouriki A, Fougère Y, De Camaret C, Case report: Case series of children with multisystem inflammatory syndrome following SARS-CoV-2 infection in Switzerland: Front Pediatr, 2021; 8; 594127
11.. Wang D, Hu B, Hu C, Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China: JAMA, 2020; 323(11); 1061-69
12.. Huang C, Wang Y, Li X, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China: Lancet, 2020; 395; 497-506
13.. Anjani G, Johnson N, Navid A, Myositis in Kawasaki disease: Rheumatol Int, 2021 [Online ahead of print]
14.. Stevens DL, Streptococcal toxic shock syndrome associated with necrotizing fasciitis: Annu Rev Med, 2000; 51; 271-88
15.. Cattalini M, Della Paolera S, Zunica F, Defining Kawasaki disease and pediatric inflammatory multisystem syndrome-temporally associated to SARS-CoV-2 infection during SARS-CoV-2 epidemic in Italy: Results from a national, multicenter survey: Pediatr Rheumatol Online J, 2021; 19(1); 29
16.. Greene AG, Saleh M, Roseman E, Sinert R, Toxic shock-like syndrome and COVID-19: Multisystem inflammatory syndrome in children (MIS-C): Am J Emerg Med, 2020; 38(11); 2492.e5-e6
17.. Maggio MC, Cimaz R, Failla MC, Typical Kawasaki disease with atypical pneumonia: A pediatric case report: Scand J Rheumatol, 2021; 50(3); 248-49
18.. Maggio MC, Corsello G, Salvo G, Brainstem auditory evoked potentials and visual potentials in Kawasaki disease: An observational monocentric study: Front Pediatr, 2020; 8; 581780
Tables
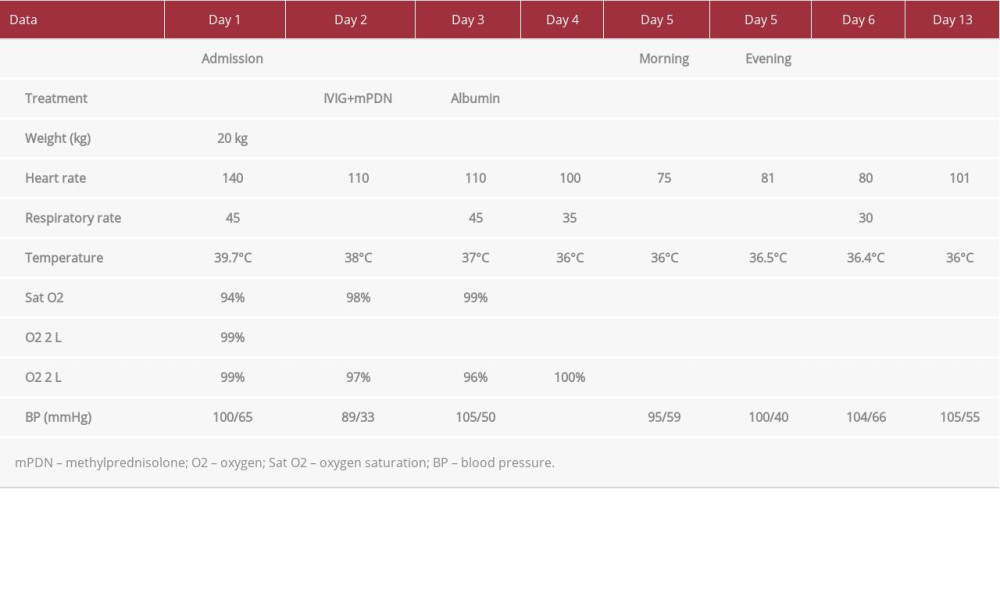 Table 1.. Case 1. Clinical findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 1.. Case 1. Clinical findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.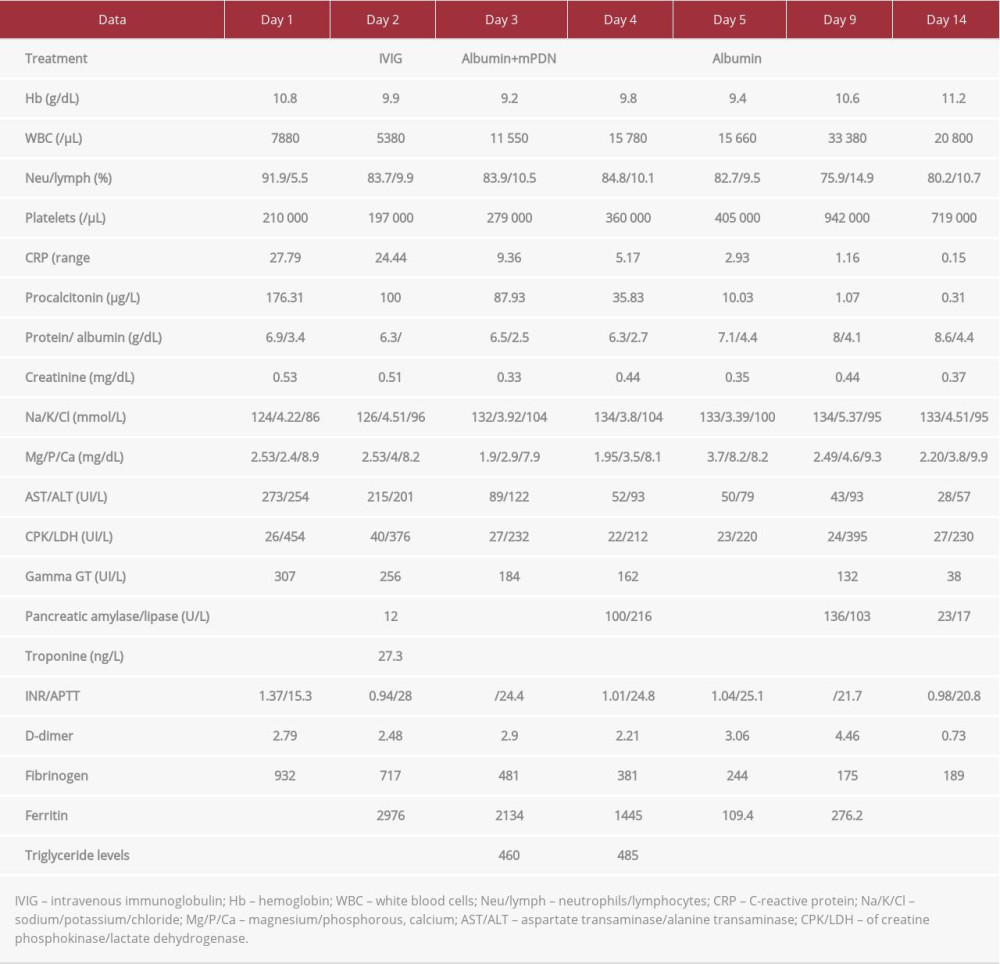 Table 2.. Case 1. Hematological findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 2.. Case 1. Hematological findings in a 7-year-old boy with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.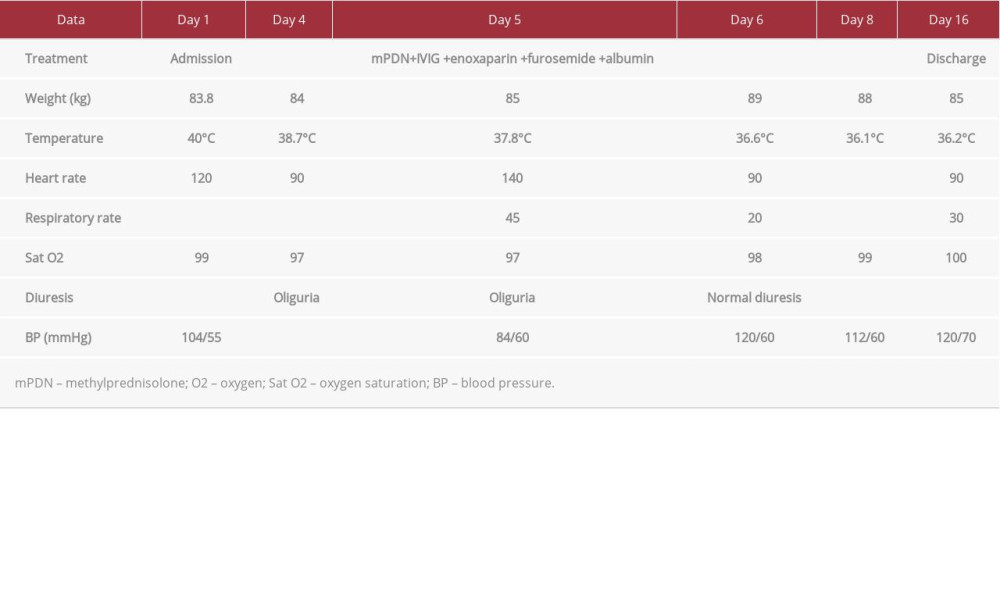 Table 3.. Case 2. Clinical findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 3.. Case 2. Clinical findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.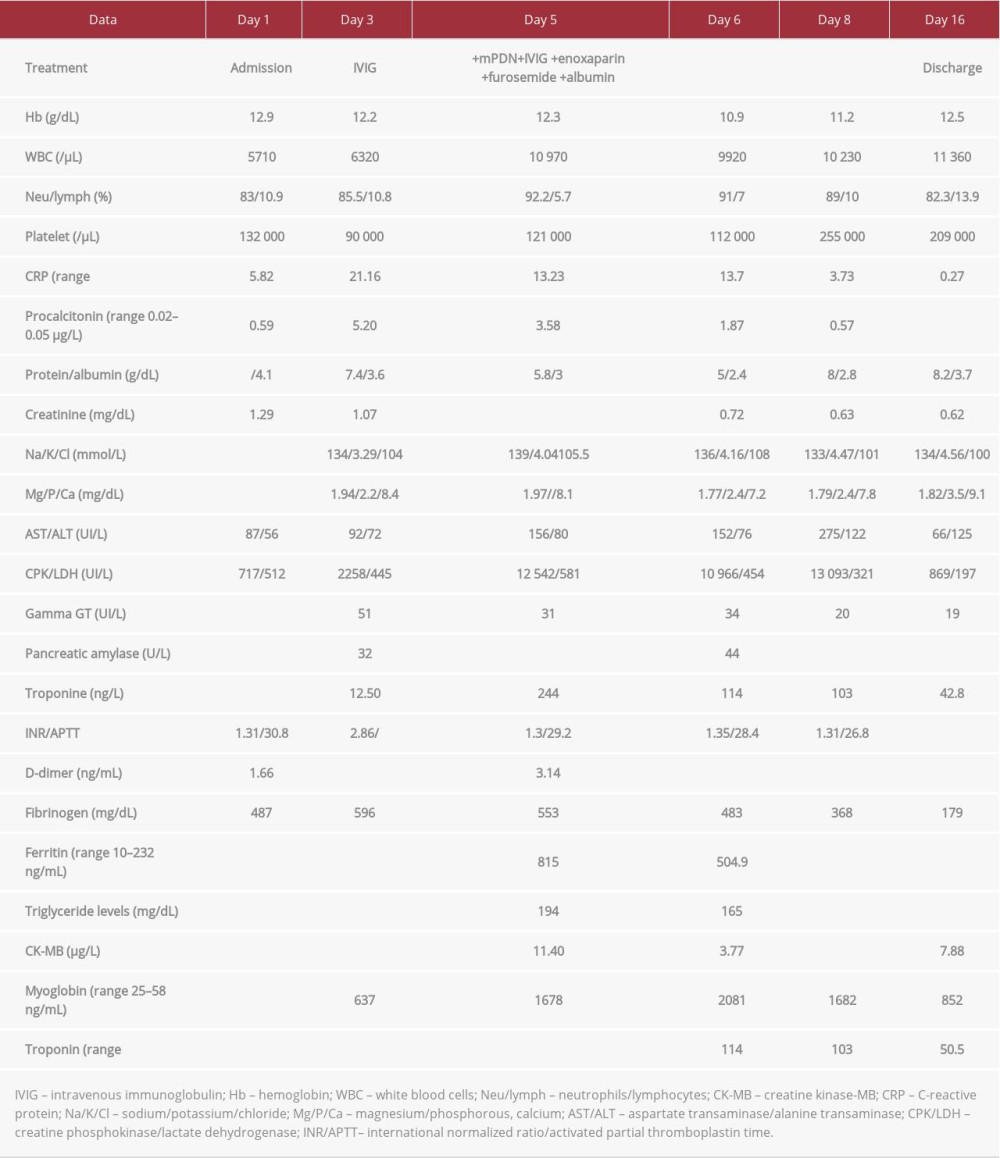 Table 4.. Case 2. Hematological findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection.
Table 4.. Case 2. Hematological findings in a 14-year-old girl with multisystem inflammatory syndrome in children (MIS-C) associated with SARS-CoV-2 infection. In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








