04 August 2021: Articles 
Jejunal Volvulus Around Gastrostomy Tube: An Exceptional Complication in Cerebral Palsy
Challenging differential diagnosis, Management of emergency care, Rare disease
Hind S. Alsaif1ABEF, Ali HassanDOI: 10.12659/AJCR.932075
Am J Case Rep 2021; 22:e932075
Abstract
BACKGROUND: Cerebral palsy may be accompanied by gastrointestinal disorders. Percutaneous endoscopic gastrostomy (PEG) tube placement is an increasingly performed procedure in these patients. While PEG tube feeding can result in weight gain and a decrease in aspiration episodes, this insertion of a PEG tube is not without complications. Specifically, intestinal volvulus following PEG tube insertion is an exceedingly rare complication.
CASE REPORT: A 34-year-old man with cerebral palsy was brought to the emergency department with a history of recurrent vomiting. He had a history of PEG tube insertion 2 months prior to his presentation. The physical examination was non-contributory. Abdominal computed tomography was suggestive of an intestinal volvulus around the PEG tube. Subsequently, the patient underwent an exploratory laparotomy, which confirmed the diagnosis and enabled successful management. Unexpectedly, the patient suffered cardiac arrest 5 days following the operation. Cardiopulmonary resuscitation was performed with pharmacological intervention and defibrillation in accordance with the advanced cardiac life support guidelines. He recovered successfully and was discharged after a 4-day observation.
CONCLUSIONS: Clinicians should have a high index of suspicion for small bowel volvulus in patients who had a PEG tube inserted, along with intestinal obstruction. Furthermore, caregivers should be educated to recognize the early signs of intestinal obstruction and seek medical attention, since a delay can result in fatal outcomes.
Keywords: Cerebral Palsy, Gastrostomy, Volvulus of Midgut, Enteral Nutrition, Intestinal Volvulus, Intubation, Gastrointestinal
Background
Cerebral palsy is often accompanied by heterogeneous conditions that negatively influence the quality of life of patients and their caregivers. Gastrointestinal disorders are seen in up to one third of these patients and include oropharyngeal dys-function, gastroesophageal dysmotility, delayed gastric emptying, and chronic constipation [1]. The insertion of a percutaneous endoscopic gastrostomy (PEG) tube has been increasingly performed in patients with cerebral palsy [1]. PEG tube feeding is associated with weight gain and a decrease in aspiration episodes. However, this procedure is not without complications.
Intestinal volvulus refers to an abnormal torsion of a segment of an intestinal loop around the axis of its mesentery, causing bowel obstruction with vascular compromise, which may lead to bowel gangrene. Early diagnosis and management define the outcome of volvulus. The small bowel volvulus is often diagnosed intra-operatively due to the lack of specific signs and symptoms [2]. Additionally, plain abdominal X-ray and ultra-sound do not provide any specific signs. Some studies have shown that the diagnostic yield of computed tomography (CT) is approximately 50% [2,3]. Herein, we describe the case of a patient who developed a volvulus around the PEG tube, which is an exceptional complication.
Case Report
A 34-year-old man with cerebral palsy and kyphoscoliosis was brought to the emergency department with a history of recurrent vomiting for 1 day prior to the presentation. He was not able to tolerate feeding and had 8–10 episodes of non-projectile, non-bloody, and non-bilious vomiting. He was given a trial of domperidone, which did not improve his condition. He had 3 bowel movements and his stools were watery, non-foul smelling, and did not contain mucus or blood. Notably, he did not have abdominal distension or fever.
The patient was non-verbal and had severe cognitive impairment. He had a history of severe gastroesophageal reflux with recurrent episodes of aspiration pneumonia, for which he underwent a PEG tube insertion 2 months before the presentation. He did not have any prior abdominal surgery.
Upon presentation, he was afebrile, and his blood pressure, pulse rate, and respiratory rate were observed to be 120/75 mmHg, 110 beats per minute, and 18 breaths per minute, respectively. The abdominal examination revealed a soft abdomen with no clinical signs of peritonitis. The skin surrounding the PEG tube had a normal appearance. The rest of the physical examination was non-contributory. Furthermore, the patient’s blood analysis revealed a hemoglobin level of 15.2 g/dL, a leukocyte count of 8.5×103 cells/μL, and a platelet count of 345×103 platelets/μL. His levels of urea, electrolytes, and liver enzymes were found to be within the normal limits.
Abdominal CT was performed for further evaluation of the patient’s condition. However, the CT images were difficult to interpret due to breathing artifacts as well as the presence of scoliosis, which displaced the bowel loops. An experienced abdominal radiologist was consulted, who suggested the presence of an abnormal twisting of the small intestinal loops around the PEG tube, causing a dilatation of the proximal bowel loops with a complete collapse of the bowel distal to the presumed point of obstruction. Furthermore, the stomach was distended and the PEG tube was in place (Figure 1).
In view of the clinical and radiological findings, the patient was prepared for an emergency laparotomy that confirmed the diagnosis of volvulus around the PEG tube and enabled successful management (Figure 2). The jejunal volvulus was untwisted and a 10-cm segment of the jejunum, which was 100 cm from the duodenojejunal flexure, was resected and primarily anastomosed. Additionally, an appendectomy was carried out during the same procedure. Thereafter, the incisions were closed in a standard fashion and the patient was transferred to the intensive care unit for postoperative care.
Unexpectedly, the patient suffered cardiac arrest 5 days following the operation. Cardiopulmonary resuscitation was performed with pharmacological intervention and defibrillation in accordance with the advanced cardiac life support guidelines. After 6 min, his sinus rhythm was restored. The patient required an emergency tracheostomy because of difficult intubation due to deformed airway anatomy. He recovered and was discharged after a 4-day observation.
Discussion
Here, we described the case of a patient with cerebral palsy who was found to have jejunal volvulus around a PEG tube. While volvulus may involve various parts of the gastrointestinal tract, small bowel volvulus is very rare [2].
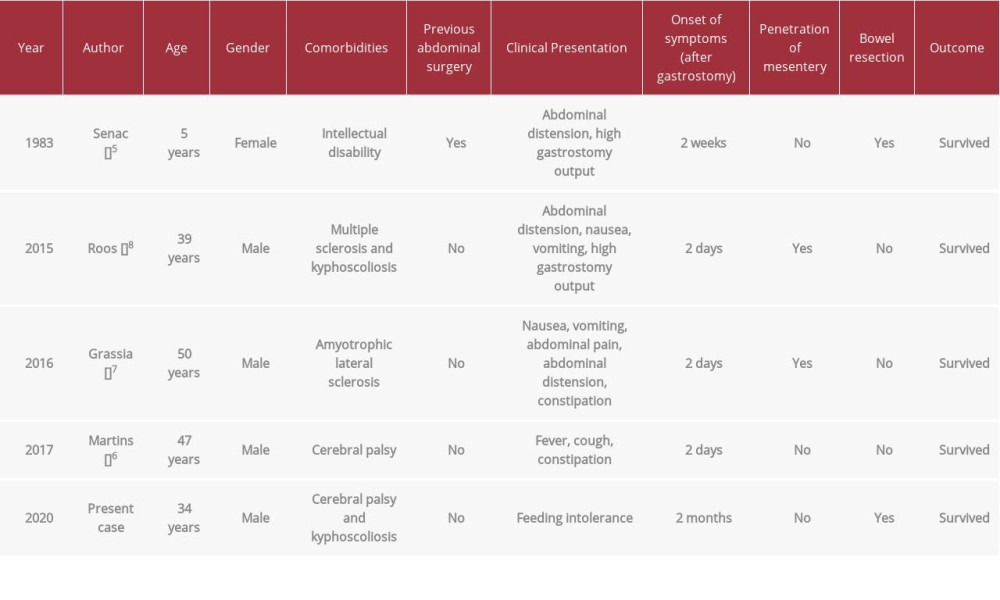
Patients with cerebral palsy seem to have an increased risk of volvulus [4], which might be related to immobility and gastrointestinal dysmotility. However, there have been a few reported cases of small bowel volvulus in patients with a PEG tube (Table 1) [4–8]. The first case of intestinal volvulus with a PEG tube was reported by Senac and Lee in 1983 in a girl with a previous abdominal surgery [5]. The postoperative adhesive bands interposed the small intestine between the stomach and the anterior abdominal wall. It has been also suggested that a thin omentum could be a potential risk factor for intestinal volvulus, as the omentum is essential to keep the small intestine in place [8]. Skeletal abnormalities, such as kyphoscoliosis, could predispose the patient to the development of volvulus by displacing the intestinal loops.
The PEG tube probably creates a fixation point for the volvulus to develop. The development of a volvulus may occur within a few days after the insertion of the PEG tube [6–8]. In contrast to some previous cases [7,8], the intestinal mesentery was not penetrated during the insertion of the PEG tube in the present case. The clinical presentation of volvulus is nonspecific and includes nausea, vomiting, abdominal pain, abdominal distension, and constipation. Additionally, patients with a PEG tube may have an increased gastrostomy output [5,8]. It should be noted that volvulus involving other organs, such as the stomach and transverse colon, have also been described in patients with a PEG tube [9,10].
The introduction of the PEG tube by Gauderer et al [11] in 1980 has replaced conventional open gastrostomy. While the insertion of the PEG tube is considered a safe and feasible procedure, the rate of complications ranges from 0.4% to 22.5% of cases [12]. Such complications may develop at any time following the placement of the tube. These complications include minor and major complications; however, minor complications are 3 times more common [13]. The major complications include bleeding, injury to internal organs, buried bumper syndrome, necrotizing fasciitis, ileus, and volvulus [14]. However, these complications have become relatively uncommon due to technical advancements in the insertion procedures [1]. Furthermore, minor complications include granuloma, wound infection, tube dislodgement and blockade, hernia, peristomal leakage, and persistent gastric fistula after removal [14]. Early recognition of complications enables prompt diagnosis and management.
The occurrence of volvulus in patients with cerebral palsy poses additional clinical and radiological challenges in making the diagnosis. First, patients with cerebral palsy can have cognitive impairment and communication difficulties, making them unable to express pain, which is the first symptom of intestinal volvulus. Second, patients with cerebral palsy often have associated anatomic deformities such as kyphoscoliosis, as in the present case, which may contribute to the difficulty in recognizing the volvulus through imaging. Hence, intestinal volvulus can be life threatening and fatal in these patients [4,15].
Conclusions
This case report sheds light on an unusual complication of the PEG tube. Clinicians should have a high index of suspicion for small bowel volvulus in patients who had a PEG tube along with intestinal obstruction. Furthermore, caregivers should be educated to recognize the early signs of intestinal obstruction and seek medical attention, since a delay can result in fatal outcomes.
Figures
References:
1.. Sullivan PB, Andrew MJ, Gastrointestinal problems in children with cerebral palsy: Cerebral palsy, 2018; 309-17, Cham, Springer https://link.springer.com/chapter/10.1007%2F978-3-319-67858-0_30
2.. Li X, Zhang J, Li B, Diagnosis, treatment and prognosis of small bowel volvulus in adults: A monocentric summary of a rare small intestinal obstruction: PLoS One, 2017; 12(4); e0175866
3.. Huang JC, Shin JS, Huang YT, Small bowel volvulus among adults: J Gastroenterol Hepatol, 2005; 20(12); 1906-12
4.. Krishnamurthy K, El Hussein S, Omarzai Y, The lethal twist – a story of un-spoken pain: small intestinal volvulus in cerebral palsy: Autops Case Rep, 2018; 8(3); e2018037
5.. Senac M, Lee F, Small-bowel volvulus as a complication of gastrostomy: Radiology, 1983; 149(1); 136
6.. Martins D, Sousa P, Pinho J, Midgut volvulus after percutaneous endoscopic gastrostomy: ACG Case Rep J, 2017; 4; e59
7.. Grassia R, Capone P, Bianchi G, Jejunal volvulus: An exceptional PEG adverse event: Gastrointest Endosc, 2016; 84(4); 748-50
8.. Roos J, A case of small-bowel obstruction after insertion of a percutaneous endoscopic gastrostomy tube due to mesenteric penetration: Ann R Coll Surg Engl, 2015; 97(5); e79-80
9.. Al-Homaidhi HS, Tolia V, Transverse colon volvulus around the gastrostomy tube site: J Pediatr Gastroenterol Nutr, 2001; 33(5); 623-25
10.. Sookpotarom P, Vejchapipat P, Chongsrisawat V, Mahayosnond A, Gastric volvulus caused by percutaneous endoscopic gastrostomy: A case report: J Pediatr Surg, 2005; 40(9); e21-23
11.. Gauderer MW, Ponsky JL, Izant RJ, Gastrostomy without laparotomy: A percutaneous endoscopic technique: J Pediatr Surg, 1980; 15(6); 872-75
12.. Itkin M, DeLegge MH, Fang JC, Multidisciplinary practical guidelines for gastrointestinal access for enteral nutrition and decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with endorsement by Canadian Interventional Radiological Association (CIRA) and Cardiovascular and Interventional Radiological Society of Europe (CIRSE): Gastroenterology, 2011; 141(2); 742-65
13.. McClave SA, Chang WK, Complications of enteral access: Gastrointest Endosc, 2003; 58(5); 739-51
14.. Hucl T, Spicak J, Complications of percutaneous endoscopic gastrostomy: Best Pract Res Clin Gastroenterol, 2016; 30(5); 769-81
15.. Rogers AP, Peterson JC, Wilhelm M, Nichol PF, Silent and deadly: Abdominal catastrophe in the nonverbal adolescent patient: Journal of Pediatric Surgery Case Reports, 2016; 8; 1-2
Figures
In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250