03 December 2021: Articles 
Early, Bilateral Re-Rupture of Quadriceps Tendon After Previous Bone-Anchor Repair for Simultaneous, Low-Energy, Bilateral Quadriceps Rupture: A Case Report and Literature Review
Unusual clinical course, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents
Andreas Panagopoulos1ABCEF*, Dimitrios KalavrytinosDOI: 10.12659/AJCR.932723
Am J Case Rep 2021; 22:e932723
Abstract
BACKGROUND: Bilateral simultaneous quadriceps tendon rupture is a relatively rare injury, more commonly seen in patients older than 50 years and is usually associated with underlying metabolic or inflammatory diseases.
CASE REPORT: We report the case of an otherwise healthy, 42-year-old man who sustained a bilateral, quadriceps tendon rupture while he was trying to pound a branch of an olive tree into the ground. On clinical examination, a defect in both proximal patella poles was found on palpation, with complete discontinuity of the extensor apparatus. A meticulous surgical repair was performed using 3 bone anchors with an uneventful postoperative rehabilitation. A biopsy specimen taken at surgery showed evidence of chronic inflammation. He had a second episode while walking fast on the beach 3.5 months postoperatively, and presented again with bilateral quadriceps rupture. He was successfully managed with bilateral allograft reconstructions, showing a very good outcome at 18 months of follow-up. Our systematic literature review covering a 20-year period (2000-2020) revealed 10 articles on bilateral quadriceps ruptures in 14 healthy patients without comorbidities. All these injuries occurred in males, with a mean age of 56.8 years, during walking, descending stairs, or participating in recreational sports; the functional outcome was good to excellent in most cases, without any reported re-ruptures. To the best of our knowledge, no similar case has been reported in the literature.
CONCLUSIONS: Bilateral quadriceps tendons rupture is a rare injury, especially in young patients without associated comorbidities. The risk of recurrence is low, but when it occurs, more complex techniques of reconstruction are needed.
Keywords: Allografts, Quadriceps Muscle, Reconstructive Surgical Procedures, Rupture, Wounds and Injuries, Humans, Male, Suture Anchors, Tendon Injuries, Tendons
Background
Bilateral rupture of the quadriceps tendons is a very rare injury, more commonly seen in mild-aged men after a minor traumatic event in the presence of an underlying systematic condition such as chronic renal failure, diabetes mellitus, hyperparathyroidism, systemic lupus erythematosus, rheumatoid arthritis, gout, severe vitamin D deficiency, osteogenesis imperfecta, alkaptonuria, and amyloidosis [1–4]. Other predisposing factors include inherited conditions like sickle cell trait and collagen type V polymorphism, as well as obesity and the use of fluoroquinolones, corticosteroids, anabolic steroids, and simvastatin [4–7]. Surgical repair using holes drilled into the patella or bone anchors is usually successful, with a very low (2–6%) incidence of recurrence [8,9]. We report a case of an otherwise healthy, 42-year-old man, who sustained a low-energy, bilateral, quadriceps tendon rupture, complicated early with bilateral re-rupture during fast walking, that was successfully managed with allograft reconstructions.
The patient was informed that data concerning the case would be submitted for publication, and he provided consent.
Case report
A 42-year-old White man, without any medical illness, presented to our department with inability to walk and extend his knees after a simple fall while harvesting olives. He was 1.72 m tall and weighed 87 Kg. The injury had occurred 4 h earlier when he was trying to pound a branch of an olive tree into the ground. He felt a sharp pain in both knees and fell down, suddenly being unable to bear weight on his legs. He was physically fit and he had never received any medication or surgical treatment. On clinical examination, he had moderate swelling over both knees, tenderness at the suprapatellar region, and a complete inability to perform a straight leg raise on both sides. A defect in both proximal patella poles was found on palpation, with complete discontinuity of the extensor apparatus (Figure 1A). Plain lateral radiographs of both knees revealed patella baja (Figure 1B) without evidence of avulsion fractures or bony spurs. An ultrasound examination of both knees confirmed the clinical diagnosis, demonstrating complete rupture of both quadriceps and no evidence of severe degeneration. The patient was informed in detail and consented for surgical exploration and repair of both his ten-dons with bone anchors.
The patient was positioned supine with a high thigh tourniquet applied on both legs and received general anesthesia. After proper preparation and draping of both limbs, a second dose of cephalosporin was administered for infection prophylaxis, the limbs were exsanguinated, and the tourniquets were simultaneously inflated to 350 mmHg. Two surgical teams performed the operations, located on either side of the patient. A longitudinal midline incision was made over the anterior aspect of both knees, extending from the upper pole of the patella to 7 cm above its proximal pole. After hematoma drainage, the quadriceps tendons were found to be retracted, frayed, and completely torn at the patella bone–tendon interface (Figure 1C). Both tendons were firmly re-attached to the patella bone using 3 bone anchors, placed in the center (two 5.5-mm IntraLine, Stryker) and at either side of the patella (three 3.5-mm IntraLine, Stryker and 1 Mitec GII, Depuy-Synthes). One limb of each anchor was whipstitched to a total length of 5 cm within the corresponding side of the quadriceps tendon, while the other free limb was free to slide through the anchor, giving the appropriate tension during tendon approximation and knot tying (Figure 2A). Before closure, a tendon specimen was taken for histopathologic examination to investigate possible underlying pathologic conditions. The knees were checked to allow for at least 90 degrees of passive flexion, without any compromise of the repair (Figure 2B). Suction drainage was applied in both knees and was removed on the second postoperative day. Lateral postoperative radio-graphs showed proper patella position and height (Figure 2C). Postoperatively, the patient was immobilized with a brace and he was not allowed full weight bearing for a period of 8 weeks. After a 2-week period, he received passive knee joint movement at 0°–30°, increasing by 30° every second week. The passive flexion could reach 110° until the 8th week, and after that he started active flexion and was able to bear weight on his knees with crutches. The histopathological examination of both tendons showed an acute, non-specific, inflammatory response. Biochemical, rheumatological, and endocrine laboratory tests were also normal. At 3 months, he was back at his sedentary job and he had started to receive special rehabilitation to build strength.
Three and a half months later, he had a sudden fall while walking fast on the beach and sustained another bilateral rupture of his quadriceps tendons. The clinical presentation was similar to the first, with effusion, suprapatellar gap, and inability to walk or perform a straight leg raise. Radiological examination revealed decreased patella height, mild tendon ossification in both knees, and pull-out of one of the anchors in both knees (Figure 3A, 3C). After informed consent was obtained, the patient was transferred to the operating room for allograft tendon reconstruction. Again, 2 surgical teams performed the operations utilizing a split Achilles tendon allograft whipstitched at both ends, similar to the ACL graft preparation. The ACL guide wire (2.7 mm) and a cannulated ACL drill (7 mm diameter) were used for bone tunnel preparation at the midline of the patella; the allograft was then passed through the patella tunnel. After adequate debridement, we microfractured the patella and made 3 parallel bone tunnels (with the ACL guide) from the superior to the inferior pole. Three parallel interlocking fiberwire sutures were placed in the quad-riceps tendon and their free ends were passed through the bone tunnels using the ACL guide wire. The quadriceps ten-dons were reapproximated while pulling the sutures, and each limb of the middle tunnel was firmly tied with the ipsilateral pair of the medial and lateral side (Figure 3B, 3D). The allograft was then passed through the quadriceps tendon and sutured to itself at 60 degrees of flexion; sided sutures were placed as well. The reconstruction was checked for uncompromising flexion up to 60–70 degrees. The patient was immobilized in bilateral long leg casts for 3 weeks, followed by hinged brace immobilization for another 8 weeks. His physiotherapy regimen was very slow, being able to perform active knee flexion at 10 weeks and full weight bearing at 3 months. At his last follow-up, 18 months postoperatively, he had a Lysholm knee score of 90 in both knees, a Tegner scale of 3, and he was able to perform light recreational activities. Both patellae had a good height in the lateral radiograph (Figure 4).
Discussion
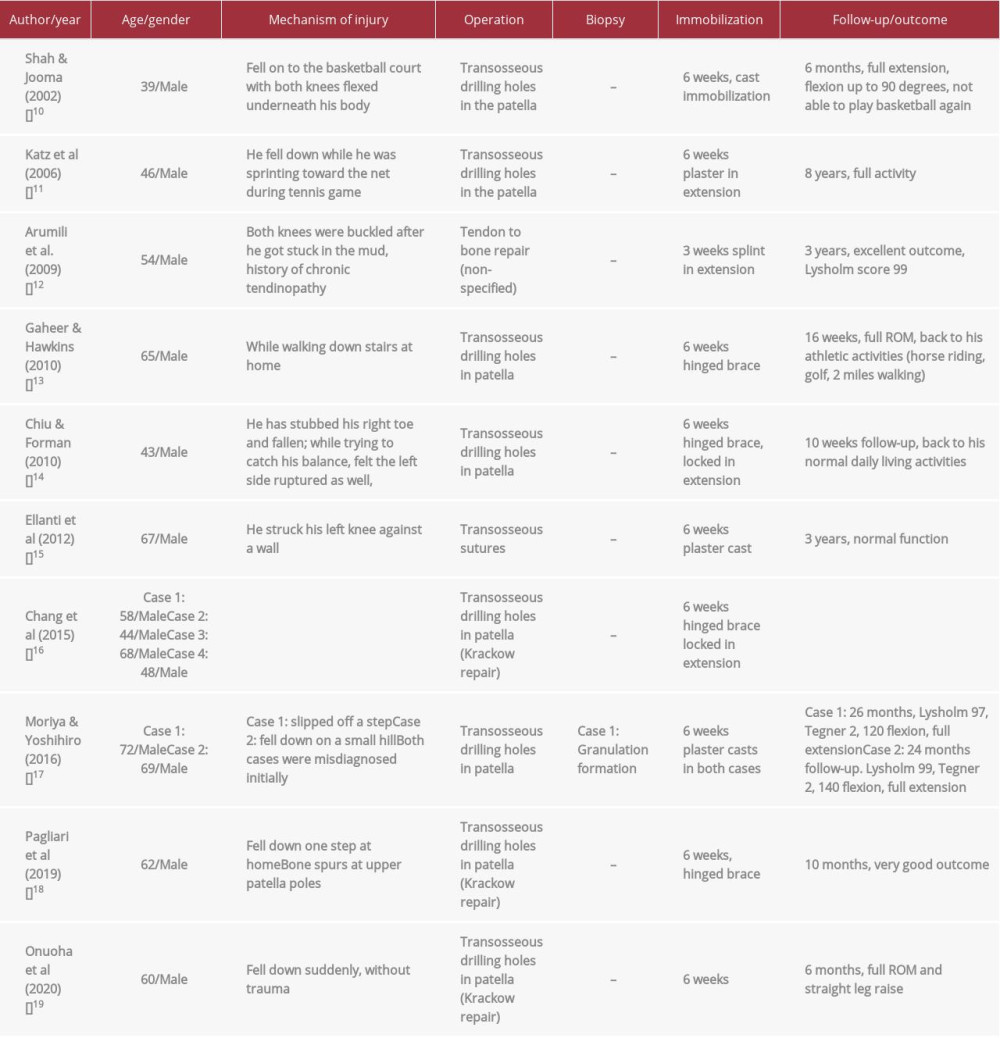
Bilateral quadriceps tendon ruptures are relatively rare, with most of the patients having more than one of the aforementioned predisposing factors [2,4]. In a systematic review by Neubauer et al [3] in 2007, 105 cases were retrieved in a 50-year period (1949–2004); interestingly, 30% of these patients had a delayed diagnosis or no diagnosis at all. Camarda et al [9], in their systematic review of bilateral extensor mechanism ruptures (excluding single case reports), found that: a) spontaneous tears occur twice as frequently than with trauma, b) quadriceps ruptures were 5 times more common than patella tendon ruptures, and c) chronic renal disease is the most common comorbidity, followed by diabetes mellitus and obesity. Our systematic literature review (Table 1) within a 20-year-old-period (2000–2020) revealed a total of 244 articles on bilateral quadriceps ruptures (using the terms bilateral AND quadriceps AND rupture). We were able to identify 10 articles reporting on 14 healthy patients without comorbidities [10–19], including 1 case of chronic tendinitis and another with spurs in the lateral radiograph. All these injuries occurred in males, with a mean age of 56.8 years (range, 39–72 years), during walking, descending stairs, or participating in recreational sports. Repair of the tendons was made through transosseous drilling of holes in the patella, followed by immobilization in extension utilizing a cast, splint, or hinged brace for at least 6 weeks in all cases except 1. A biopsy specimen was obtained in only 1 case, which showed formation of granulated tissue without evidence of chronic tendinitis, as in our case. The functional outcome was good to excellent in most cases, without any reported re-ruptures. We found no cases of recurrent bilateral quadriceps ruptures in healthy patients in the literature, but Camarda et al [9] reported 2 such cases in patients with history of chronic renal disease. Our case is unique, not only because of the absence of an underlying disease, obesity or medications, but also due to the early bilateral and low-energy re-rupture that happened as soon as the patient returned to his daily living activities (3.5 months postoperatively). The reason for this failure may have been the use of bone anchors, but they have been proved equal to or superior to transosseous suturing in terms of pull-out strength in both cadaveric and clinical studies; they also allow less surgical time, smaller incision, absence of non-absorbable material at the apex of the patella, less incidence of patella fractures, and smaller dead-length of sutures, thus facilitating early rehabilitation [20–24]. In our patient, we used fully threaded titanium anchors (except for 1 Mitec GII), showing high pull-out strength and resistance to failure in various studies. Petri et al [20] performed a comparative study in 30 tenotomized cadaveric quadriceps tendons between titanium (TA) or peek (HA) anchors vs classic transosseous suture (TS) repair; both anchors demonstrated less gap formation during cyclic loading (20th–250th cycle: TA 1.9±0.1, HA 1.5±0.5, vs TS 33.3±1.9 mm,
Conclusions
Bilateral simultaneous rupture of quadriceps tendons is a rare injury, especially in patients without associated disease. Repair of the tendons using transosseous drills or bone anchors is usually successful, with a very low incidence of recurrence. When recurrence happens, more complex techniques of reconstruction are necessary.
Figures
References:
1.. Reito A, Paloneva J, Mattila VM, The increasing incidence of surgically treated quadriceps tendon ruptures: Knee Surg Sports Traumatol Arthrosc, 2019; 27; 3644-49
2.. Shah MK, Simultaneous bilateral rupture of quadriceps tendons: Analysis of risk factors and associations: South Med J, 2002; 95(8); 860-66
3.. Neubauer T, Wagner M, Potschka T, Riedl M, Bilateral, simultaneous rupture of the quadriceps tendon: A diagnostic pitfall? Report of three cases and meta-analysis of the literature: Knee Surg Sports Traumatol Arthrosc, 2007; 15(1); 43-53
4.. Pope JD, El Bitar Y, Plexousakis MP, Quadriceps tendon rupture: StatPearls, 2020, Treasure Island (FL), StatPearls Publishing
5.. Sherman N, Sandberg R, Hardy J, Recurrent, bilateral quadriceps tendon rupture due to indirect trauma in a patient with sickle cell trait: A case report: J Orthop Sci, 2020; 25(1); 197-200
6.. Lodha S, Pal R, Bhadada SK, Spontaneous simultaneous bilateral quadriceps tendon rupture associated with severe vitamin D deficiency: Clin Endocrinol (Oxf), 2019; 91(4); 580-82
7.. Kelly BM, Rao N, Louis SS, Bilateral, simultaneous, spontaneous rupture of quadriceps tendons without trauma in an obese patient: A case report: Arch Phys Med Rehabil, 2001; 82(3); 415-18
8.. Ciriello V, Gudipati S, Tosounidis T, Clinical outcomes after repair of quadriceps tendon rupture: A systematic review: Injury, 2012; 43(11); 1931-38
9.. Camarda L, D’Arienzo A, Morello S, Bilateral ruptures of the extensor mechanism of the knee: A systematic review: J Orthop, 2017; 14(4); 445-53
10.. Shah M, Jooma N, Simultaneous bilateral quadriceps tendon rupture while playing basketball: Br J Sports Med, 2002; 36(2); 152-53
11.. Katz T, Alkalay D, Rath E, Bilateral simultaneous rupture of the quadriceps tendon in an adult amateur tennis player: J Clin Rheumatol, 2006; 12(1); 32-33
12.. Arumilli B, Adeyemo F, Samarji R, Bilateral simultaneous complete quadriceps rupture following chronic symptomatic tendinopathy: A case report: J Med Case Rep, 2009; 3; 9031
13.. Gaheer RS, Hawkins A, Rapid recovery from spontaneous and simultaneous bilateral quadriceps tendon rupture in an active, healthy individual: Orthopedics, 2010; 33(7); 512
14.. Chiu M, Forman ES, Bilateral quadriceps tendon rupture: A rare finding in a healthy man after minimal trauma: Orthopedics, 2010; 33(3); 01477447-20100129-32
15.. Ellanti P, Davarinos N, Morris S, Rice J, Bilateral synchronous rupture of the quadriceps tendon: Ir J Med Sci, 2012; 181(3); 423-25
16.. Chang ES, Dodson CC, Tjoumakaris F, Functional results following surgical repair of simultaneous bilateral quadriceps tendon ruptures: Phys Sportsmed, 2014; 42(2); 114-18
17.. Moriya T, Yoshihiro A, Bilateral simultaneous rupture of the quadriceps ten-dons in healthy individuals: Trauma Cases Rev, 2016; 2; 1510043
18.. Pagliari M, Menna CR, Migliorini A, Molinari M, Atraumatic acute bilateral quadriceps tendon rupture in a patient with bilateral patella spurs. A case report and review of literature: Acta Biomed, 2018; 90(1–S); 203-8
19.. Onuoha KM, Ajiboye OK, Kumar R, Spontaneous bilateral quadriceps tendon rupture: A case report: Pan Afr Med J, 2020; 37; 84
20.. Petri M, Dratzidis A, Brand S, Suture anchor repair yields better bio-mechanical properties than transosseous sutures in ruptured quadriceps tendons: Knee Surg Sports Traumatol Arthrosc, 2015; 23(4); 1039-45
21.. Sherman SL, Black B, Mooberry MA, Biomechanical evaluation of suture anchor versus transosseous tunnel patellar tendon repair techniques: J Knee Surg, 2019; 32(8); 825-32
22.. Plesser S, Keilani M, Vekszler G, Clinical outcomes after treatment of quadriceps tendon ruptures show equal results independent of suture anchor or transosseus repair technique used – a pilot study: PLoS One, 2018; 13(3); e0194376
23.. Tucker JE, Jones CR, Bilateral quadriceps tendon repair with suture anchors: Case series: Perm J, 2020; 24; 19.098
24.. Mehta AV, Wilson C, King TS, Gallo RA, Outcomes following quadriceps tendon repair using transosseous tunnels versus suture anchors: A systematic review: Injury, 2021; 52(3); 339-44
25.. Trobisch PD, Bauman M, Weise K, Histologic analysis of ruptured quad-riceps tendons: Knee Surg Sports Traumatol Arthrosc, 2010; 18(1); 85-88
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250