20 November 2021: Articles 
A Rare Case of Bacteremia After Liver Transplantation
Rare disease
Le Thi Viet Hoa12ACDEF, Pham Dang Hai3AEF*DOI: 10.12659/AJCR.933992
Am J Case Rep 2021; 22:e933992
Abstract
BACKGROUND: Elizabethkingia meningoseptica is an emerging pathogen in hospital environments. Immunocompromised individuals have a high risk of infections caused by E. meningoseptica, especially after transplantation. E. meningoseptica is associated with prolonged hospital stays and high mortality. In addition, E. meningoseptica is commonly resistant to many antibiotics used for gram-negative bacterial infections. We introduce the first case of E. meningoseptica bacteremia in a recipient of a liver transplant in Vietnam.
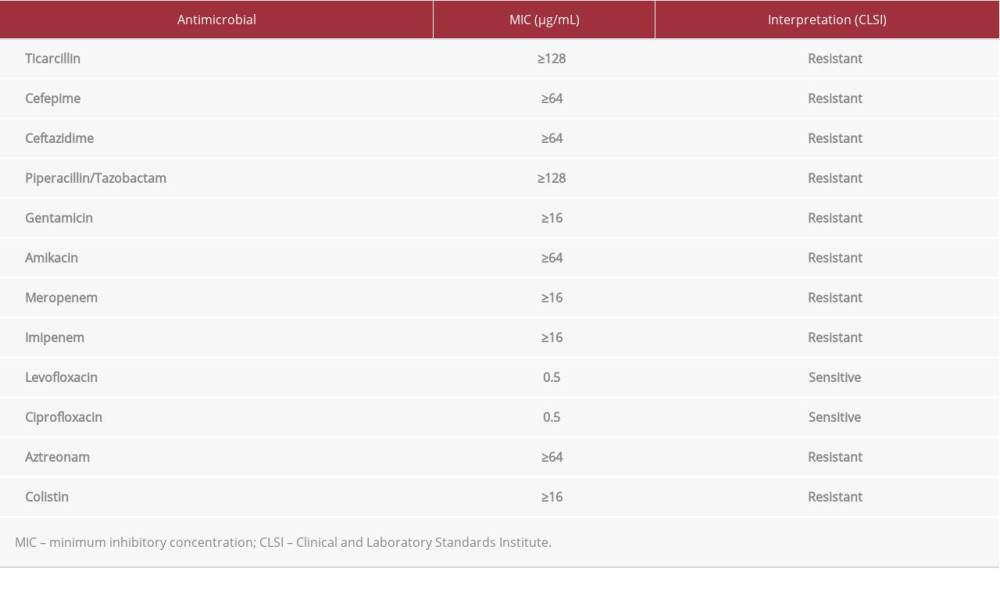
CASE REPORT: A 55-year-old woman with end-stage liver disease due to biliary cirrhosis underwent living donor liver transplantation at the 108 Military Central Hospital. On day 3 after transplantation, the patient had an acute cellular rejection, and corticosteroid pulse therapy was used. On day 7 after transplantation, the patient had a fever and an increased white blood cell count and C-reactive protein level. Blood cultures were positive for E. meningoseptica. Intravenous levofloxacin was administered for 10 days. The patient showed an excellent treatment response to the antibiotic therapy and was discharged.
CONCLUSIONS: E. meningoseptica, a multidrug-resistant gram-negative bacteria, can be considered an emerging pathogen in the hospital environment, especially in patients receiving organ transplants. Early recognition helps physicians to improve patient outcomes.
Keywords: Bacteremia, beta-Lactamase GOB-1, Elizabethkingia meningoseptica, Liver Transplantation, Anti-Bacterial Agents, Chryseobacterium, Female, Flavobacteriaceae Infections, Humans, Living Donors
Background
Approximately 5 to 10 cases of
Case Report
A 55-year-old woman presented to the 108 Military Central Hospital in Vietnam with a history of end-stage liver disease due to biliary cirrhosis. A right-lobe liver transplantation was performed from a living donor. Immunosuppressive therapy included tacrolimus, dose adapted on target trough level (12–15 ng/mL), and methylprednisolone 40 mg 4 times per day and tapered after that. On day 3 after transplantation, an acute cellular rejection occurred, and corticosteroid pulse therapy with a dose of 500 mg per day for 3 consecutive days was administered.
On day 7 after transplantation, the patient’s blood pressure was 110/70 mmHg, heart rate was 102 beats per min, respiratory rate was 20 breaths per min, and temperature was 38.5°C. A peripheral white blood cell count increased from 8.2 g/L to 26 g/L, and C-reactive protein level increased from 6 mg/L to 35 mg/L. The abdominal ultrasound was normal. The patient continued to receive meropenem 1 g every 8 h. Blood cultures were positive for
On day 14 after transplantation, the normal peripheral blood leukocyte count was 9.7 g/L, and the C-reactive protein level dropped to 4.5 mg/L. Antibiotics were continued for a total of 10 days. Repeat blood cultures were negative. The patient was first transferred to the ward and then discharged.
Discussion
There are multiple infectious sources of
Conclusions
References:
1.. King EO, Studies on a group of previously unclassified bacteria associated with meningitis in infants: Am J Clin Pathol, 1959; 31; 241-47
2.. Issack MI, Neetoo Y: J Infect Dev Ctries, 2011; 5; 834-39
3.. Bloch KC, Nadarajah R, Jacobs R: Medicine (Baltimore), 1997; 76; 30-41
4.. Musalem HM, Honjol YN, Tuleimat LM: Am J Case Rep, 2017; 18; 1014-19
5.. Hsueh PR, Teng LJ, Yang PC: Eur J Clin Microbiol Infect Dis, 1997; 16; 568-74
6.. Lin Y-T, Chiu C-H, Chan Y-J: Scand J Infect Dis, 2009; 41; 628-34
7.. Govindaswamy A, Bajpai V, Trikha V: Intractable Rare Dis Res, 2018; 7; 172-76
8.. Kirby JT, Sader HS, Walsh TR, Jones RN: J Clin Microbiol, 2004; 42; 445-48
9.. Woodford N, Palepou MF, Babini GS: Antimicrob Agents Chemother, 2000; 44; 1448-52
10.. Balm MND, Salmon S, Jureen R: J Hosp Infect, 2013; 85; 134-40
11.. Young SM, Lingam G, Tambyah PA: Antimicrob Resist Infect Control, 2014; 3; 35
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250