26 November 2021: Articles 
Early Low Level of Procalcitonin Is Associated with a Favorable Outcome in a Case of a Surviving Patient with 80% Body Surface Area Thermal Burn
Unusual clinical course, Diagnostic / therapeutic accidents, Management of emergency care
Bogdan Pavel- A Study design/planning
- B Data collection/entry
- E Preparation of manuscript
- *Corresponding author: [email protected]
- *Corresponding author: [email protected]
- B Data collection/entry
- D Data interpretation
- E Preparation of manuscript
- C Data analysis/statistics
- F Literature analysis/search
- E Preparation of manuscript
- F Literature analysis/search
- A Study design/planning
- D Data interpretation
- E Preparation of manuscript
DOI: 10.12659/AJCR.934052
Am J Case Rep 2021; 22:e934052
Abstract
BACKGROUND: Burns covering a large skin surface area represent a life-threatening condition due to the release of cytokines and the activation of a systemic inflammatory response, as well as the potential for septic complications. Outcome for these patients is related to the burn surface, age, and coexisting diseases. Although some severity scores are available, such as the Abbreviated Burn Severity Index (ABSI), Baux score, R-Baux score, Boston score, and Belgian Outcome Burn Injury (BOBI) score, none can provide a solid picture of the final outcome. Recent studies claim that procalcitonin, a known sepsis marker, can assist in estimating a burn patient’s chance of survival from the time of admission, and can also assist in estimating the chance of sepsis occurrence during hospitalization.
CASE REPORT: In this manuscript we report the case of a 28-year-old man who suffered burn injuries on approximately 80% of his body surface due to poor handling of a gasoline can in August 2018. Despite high severity index scores and early high values of C-reactive protein, we noticed a low level of early procalcitonin. In this case, as well in our previous experience, early low procalcitonin was associated with a favorable outcome.
CONCLUSIONS: Early procalcitonin values might prove to be a promising prognosis marker in some cases of extensive burns.
Keywords: Burns, Injury Severity Score, procalcitonin, Adult, Body Surface Area, Humans, Male, Sepsis
Background
Burns have been mentioned in medical documents since antiquity; the first writings about how to address this issue appeared in 1600 BCE, recommending resin, honey, tinctures, wine, and myrrh. Ambroise Pare performed the first burn wound excision, but 2 centuries passed before Reverdin made the first burn excision followed by skin grafting, in 1869 [1]. Burns are caused by physical factors such as thermic agents (scalds, flame, contact), electrocution, radiation, or chemical factors such as acids or bases. A systemic inflammatory response induced by the cytokines released from the burn lesion takes place in response to the burn. The magnitude of this response is influenced by the patient’s previous health condition. A systemic inflammatory response generally occurs in the case of a burn on >30% of the total body surface area (TBSA). Systemic reactions include: depressed cardiac contractility, decreased preload due to the leakage of water into the interstitium, increased capillary permeability, impaired lung function (including acute respiratory distress syndrome-ARDS) by direct or secondary hit, decreased immune response, and hypermetabolism (Figure 1).
Another feature of burns is the potential for septic complications, due to loss of the skin barrier coupled with depressed immune function.
At the root of these systemic reactions are certain cytokines, especially TNFα and IL-1β, which produce tissue lesions, as well as secretion of some biomarkers, such as procalcitonin. Although procalcitonin is a validated sepsis marker, it is induced by the same cytokines in both inflammatory reactions and septic ones. Procalcitonin has proven to be a good, specific marker for bacterial infection, with no relevance to viral infection (due to IFNγ inhibition of IL-1β secretion) or fungal infection (similarly due to IFNγ inhibition of IL-1β secretion) [2–5]. Moreover, there are some reports describing elevated procalcitonin levels in non-septic conditions such as pancreatitis or trauma, as well as burns [6]. Procalcitonin has a rapid kinetic course, with an early increase within the first few hours after sepsis onset, reaching a maximum at 24-48 h after the injury [7,8].
In septic burn patients, procalcitonin has a cut-off value ranging from 0.5–1.5 ng/ml [7,9,10] although some debate still exists about the utility of procalcitonin in diagnosing septic complications in burns [11]. Early high values of procalcitonin in non-septic conditions seem to be associated with an unfavorable outcome, possibly related to future sepsis occurrence in these patients. A solid correlation between early procalcitonin value and sepsis occurrence has been observed [7,12–14].
It is generally accepted that the severity and prognosis depend on the burn surface area, the patient’s age, the preexistence of coexisting diseases, and the presence or absence of airway burns. However, procalcitonin, a sepsis-dedicated bio-marker with a rapid kinetic profile (onset at 24–48 h), might play a role in prognosis prediction even in non-septic condition, such as burns. Consequently, we have chosen an extensive burn case to illustrate this observation.
Case Report
The Ethics Committee of the Clinical Emergency Hospital of Plastic Surgery and Burns approved the publication of this case (Notice 3/19.06.2020) after informed consent was obtained.
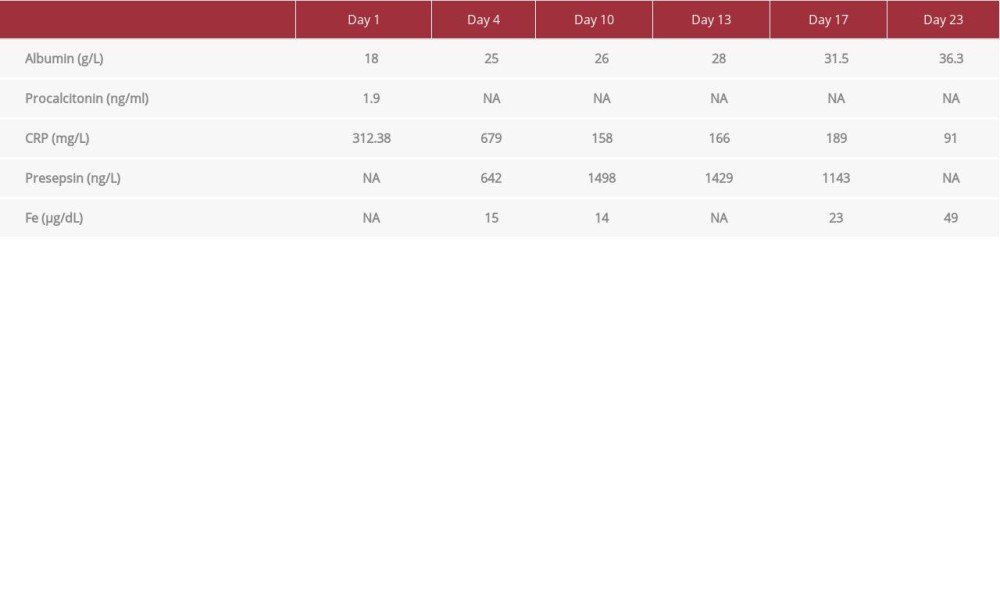
A 28-year-old man experienced a thermal burn due to improper handling of a gasoline can within a house outbuilding. The patient was initially transported to Bacau Emergency Hospital with superficial, deep partial-thickness burns (grade IIA, IIB) and full-thickness burns (grade III on approximately 3% total body surface area), resulting in a total of approximately 80% body surface area lesions (Figure 2A–2C). He was treated with chest and abdominal debridement and decompression incisions. The patient also underwent protective tracheal intubation in the context of suspicion of airway burns. Initial blood tests revealed increased C-reactive protein (CRP) (312.38 mg/L), moderately elevated procalcitonin (1.9 ng/ml), and severe hypoproteinemia (total protein=29.1 g/L; albumin=18 g/L). The severity scores amounted to the following values: ABSI=12 points, Baux=108 points, R-Baux=85 points.
Upon being transferred to the Clinical Hospital of Plastic, Reparatory, and Burn Surgery (48 h after the fire incident), local conservative nonsurgical treatment for superficial burns was performed. This treatment consisted of lavage and dressing with silver-containing products, followed by admission of the patient to the Intensive Care Unit where respiratory support using mechanical ventilation was continued. The patient presented with signs of an extremely aggressive burn-induced inflammatory reaction, reflected in the values for CRP (679 mg/L), albumin (25 g/L), presepsin (642 ng/L), and serum iron (Fe; 15 µg/dL) on admission to our department. In our department, sepsis was monitored via presepsin as opposed to procalcitonin levels.
The patient’s respiratory function was stabilized, and because the patient showed no signs of inhalation injury (judging by the oxygenation index, ventilator parameters, and chest X-ray image), he was extubated the next day.
The standard procedure for the management of large mixed-type second-degree burns includes conservative local treatment methods (removing devitalized tissue and application of special topical antimicrobial agents). Superficial and deep partial-thickness burns were treated conservatively by use of silver-containing products and full-thickness burns were excised and grafted with expanded meshed autografts. An unfavorable evolution of the burn lesions would require a more complex approach, such as allogenic grafts, xenografts, or synthetic skin.
The patient received burn-protocol treatment consisting of: proton-pump inhibitor (pantoprazole 40 mg), thromboprophylaxis with enoxaparin (40 mg per day), analgesics (paracetamol 4 g/day, morphine on request), antioxidants (acetylcysteine), oligoelements, and enteral and parenteral nutrition followed by normal feeding (to provide adequate nutrition in accordance with the Toronto formula estimation for caloric intake) [15]. Adequate tissue perfusion was achieved with the help of crystalloid solutions, maintaining MAP >65 mmHg and diuresis >0.5 ml/bw/h, lactate <2 mmol/L, and ScVO2 >70% (in the absence of anemia or desaturation) [16].
From the 8th day of hospitalization and after colonization of the wound with
The evolution of the intermediary burn injuries was favorable and resulted in complete recovery. On the 21st day, the patient was transferred to the burn unit where he stayed for another 3 weeks. On the 35th day the full-thickness burn was excised and grafted with expanded meshed (3: 1) autograft harvested from the right forearm and the anterior side of the thigh. In the case of our patient, during the recovery process, the second-degree (IIA/IIB) lesions, treated conservatively, did not deepen, and had a favorable evolution towards spontaneous epithelialization. After healing of the second-degree lesions (more precisely, on the 35th day after the accident), we excised and grafted the deep lesions that remained unhealed and that covered 3% TBSA. The patient was discharged on the 44th day from the initial injury.
Discussion
The main concern in a patient with extensive burn lesions is the event of a cytokine storm, which induces multiple organ dysfunction syndrome, when the body becomes frail and more susceptible to infections due to impairment of the skin barrier and presence of immunosuppression [18–26]. This inflammatory reaction is induced by skin burn lesions and is aggravated by their unfavorable evolution (burn deepening). In our patient, CRP and total protein values (based on samples collected upon admission) suggested an extremely severe inflammatory disorder secondary to the burn injury. An ABSI score of 12 points (the score for our patient) is associated with an 80–90% mortality rate. Nonetheless, procalcitonin values lower than 1.9 ng/mL after 48 h signify a favorable prognosis [14,27].
In our case, we observed a discrepancy between CRP value (312.38 mg/L) and procalcitonin value (1.9 ng/ml) at 24 h. The CRP value of 312.38 is a high value that is theoretically associated with a high inflammatory response and should indicate a poor outcome. Nevertheless, the procalcitonin value was not similarly elevated, and both previous reports and our own experience led us to believe that procalcitonin could be a more reliable marker of inflammatory response and outcome. This may be due to the fact that CRP is induced by IL-6 and procalcitonin by TNFα and IL-1β. On the other hand, increased procalcitonin values in the initial days following a burn are reported to be associated with an increased risk for sepsis [3,8]. This was also the case for our patient, who started presenting signs of sepsis on the eighth day of hospitalization.
Aiming to prevent a poor outcome, our first intention was to combat deepening of the intermediate burn lesions, which represented 77% of his body surface area [28]. To accomplish this, 3 principles should be complied with: proper blood flow for tissue perfusion of the burn lesions, adequate caloric intake, and the prevention of infection of the burn lesions. Adequate tissue perfusion was monitored using mean arterial pressure, diuresis, lactate, and central venous oxygen saturation values. Caloric intake was initially ensured by means of enteral and parenteral nutrition solution, followed by normal feeding in accordance with the Toronto formula for burns. Parenteral nutrition was added at the beginning, to supplement enteral nutrition to target the caloric requirement according to the Toronto formula. Parenteral nutrition was continued for no more than a week after the injury; until his gastric tolerance was ascertained. Although enteral nutrition using nasojejunal tube would have been preferred, unfortunately, such a device was not available at that time. Instead, gastric nutrition with prokinetics supplements was used.
In our present case, clinical monitoring (mean arterial pressure, urine output, and SCvO2) and a nutrition plan according to the Toronto formula proved to be sufficient for the patient’s improvement despite the lack of calorimetry or invasive cardiac output monitoring.
Regarding the second-degree burn lesions, although recent studies suggest that silver can delay the wound-healing process and should not be used in a routine manner, we considered that in this case of a patient with extensive burns and treated under conditions of high risk of nosocomial infections, the efficacy of a local antimicrobial treatment should be of high priority in burn wound care. This is why we used silver-containing products for our patient during the healing process.
Regarding the management of the third-degree burns, we considered that later excisions and grafting were reasonable because we anticipated the possibility of burn wounds deepening during the wound evolution (a progression of a superficial partial-thickness burn to a deep partial-thickness or full-thickness burn), as well as the lack of homologous donor areas. In addition, there was a lack of other possibilities to cover the excised areas with homographs or temporary skin substitutes.
Burn lesion infection prevention was achieved by isolating the patient and performing daily wound dressing after debridement with bactericidal solutions [29]. Despite these measures, the patient presented signs of infection on the eighth day after the accident (sixth day from admission to our hospital). Wound cultures detected colonization with
Despite the poor severity score, other factors were encouraging: his age, low procalcitonin values within the first 48 h of the incident, and no vasopressor requirement [30–34]. As we have previously observed in our burn victims, young patients with vasopressor necessity and high levels of procalcitonin within 48 h after the injury are at risk of a poor outcome and increased mortality [27]. In their cases, procalcitonin levels were in accordance with the severity score, while low levels of procalcitonin correlated well with survival, as in our present case.
Conclusions
Procalcitonin values within 48 h after burn injury (in non-septic patients) currently do not constitute a standardized marker for injury severity scores. However, the aforementioned observation in our patients, previous reports, and this particular case urge us to take procalcitonin into consideration as a credible severity outcome marker in connection with other severity predictors and vasopressor requirement. The correlation of early isolated procalcitonin values, as an endogenous marker of inflammatory response and outcome, should be investigated in future studies to be validated. For the moment, we can merely notice the association between low early values and favorable outcome.
Figures
References:
1.. Lee KC, Joory K, Moiemen NS, History of burns: The past, present and the future: Burns Trauma, 2014; 2(4); 169-80
2.. Linscheid P, Seboek D, Nylen ES, In vitro and in vivo calcitonin I gene expression in parenchymal cells: A novel product of human adipose tissue: Endocrinology, 2003; 144(12); 5578-84
3.. Leli C, Ferranti M, Moretti A, Procalcitonin levels in gram-positive, gram-negative, and fungal bloodstream infections: Dis Markers, 2015; 2015; 701480
4.. Cortegiani A, Misseri G, Ippolito M, Procalcitonin levels in candidemia versus bacteremia: a systematic review: Crit Care, 2019; 23(1); 190
5.. Srinivasamurthy BC, Sannappa MN, Pathogenesis in fungal infection: Fungal infections of the Central Nervous System, 2019; 31-42, Springer
6.. Meisner M, Adina H, Schmidt J, Correlation of procalcitonin and C-reactive protein to inflammation, complications, and outcome during the Intensive Care Unit course of multiple-trauma patients: Crit Care, 2006; 10(1); R1
7.. Cabral L, Afreixo V, Meireles R, Procalcitonin kinetics after burn injury and burn surgery in septic and non-septic patients – a retrospective observational study: BMC Anesthesiol, 2018; 18(1); 122
8.. Meisner M, Update on procalcitonin measurements: Ann Lab Med, 2014; 34(4); 263-73
9.. Lavrentieva A, Kontakiotis T, Lazaridis L, Inflammatory markers in patients with severe burn injury. What is the best indicator of sepsis?: Burns, 2007; 33(2); 189-94
10.. Mokline A, Garsallah L, Rahmani I, Procalcitonin: A diagnostic and prognostic biomarker of sepsis in burned patients: Ann Burns Fire Disasters, 2015; 28(2); 116-20
11.. Azzini AM, Dorizzi RM, Sette P, A 2020 review on the role of procalcitonin in different clinical settings: An update conducted with the tools of the Evidence Based Laboratory Medicine: Ann Transl Med, 2020; 8(9); 610
12.. Xu L, Jin J, Wu G, Elevated serum procalcitonin early after extensive burn: Influencing factors and clinical significance: Burns, 2021; 47(6); 1399-407
13.. Kim HS, Yang HT, Hur J, Procalcitonin levels within 48 hours after burn injury as a prognostic factor: Ann Clin Lab Sci, 2012; 42(1); 57-64
14.. Yang XJ, Jin J, Xu H, [Prognostic significance of serum procalcitonin in patients with extremely severe burn and sepsis.]: Zhonghua Shao Shang Za Zhi, 2016; 32(3); 147-51 [in Chinese]
15.. Allard JP, Pichard C, Hoshino E, Validation of a new formula for calculating the energy requirements of burn patients: J Parenter Enteral Nutr, 1990; 14(2); 115-18
16.. , Surviving Sepsis Campaign International Guidelines: Pediatrics, 2020; 145(5); e20200629
17.. Xia JJ, Wang F, Jiang XN, Serum iron levels are an independent predictor of in-hospital mortality of critically ill patients: A retrospective, single-institution study: J Int Med Res, 2019; 47(1); 66-75
18.. Nielson CB, Duethman NC, Howard JM, Burns: Pathophysiology of systemic complications and current management: J Burn Care Res, 2017; 38(1); e469-81
19.. Nguyen LN, Nguyen TG, Characteristics and outcomes of multiple organ dys-function syndrome among severe-burn patients: Burns, 2009; 35(7); 937-41
20.. Huang YS, Yang ZC, Liu XS, Serial experimental and clinical studies on the pathogenesis of multiple organ dysfunction syndrome (MODS) in severe burns: Burns, 1998; 24(8); 706-16
21.. Kim HS, Kim JH, Yim H, Kim D, Changes in the levels of interleukins 6, 8, and 10, tumor necrosis factor alpha, and granulocyte-colony stimulating factor in Korean burn patients: Relation to burn size and postburn time: Ann Lab Med, 2012; 32(5); 339-44
22.. Dehne MG, Sablotzki A, Hoffmann A, Alterations of acute phase reaction and cytokine production in patients following severe burn injury: Burns, 2002; 28(6); 535-42
23.. Hidalgo F, Mas D, Rubio M, Garcia-Hierro P, Infections in critically ill burn patients: Med Intensiva, 2016; 40(3); 179-85
24.. Church D, Elsayed S, Reid O, Burn wound infections: Clin Microbiol Rev, 2006; 19(2); 403-34
25.. Mace JE, Park MS, Mora AG, Differential expression of the immunoinflammatory response in trauma patients: Burn vs. non-burn: Burns, 2012; 38(4); 599-606
26.. Heideman M, Bengtsson A, The immunologic response to thermal injury: World J Surg, 1992; 16(1); 53-56
27.. Pavel BI, Vatasoiu LMV, Stanculea AT, High values of procalcitonin in non-septic patients with thermal and airway burns – an early severity predictor?: Romanian J Mil Med, 2019; 122(3); 22-28
28.. Sheng Z, Prevention of multiple organ dysfunction syndrome in patients with extensive deep burns: Chin J Traumatol, 2002; 5(4); 195-99
29.. Wasiak J, Cleland H, Burns: Dressings: BMJ Clin Evid, 2015; 2015; 1903
30.. Prasad A, Thode HC, Singer AJ, Predictive value of quick SOFA and revised Baux scores in burn patients: Burns, 2020; 46(2); 347-51
31.. , Development and validation of a model for prediction of mortality in patients with acute burn injury: Br J Surg, 2009; 96(1); 111-17
32.. Brusselaers N, Agbenorku P, Hoyte-Williams PE, Assessment of mortality prediction models in a Ghanaian burn population: Burns, 2013; 39(5); 997-1003
33.. Tahir S, Memon AR, Kumar M, Ali SA, Prediction of mortality after major burn: Physiological versus biochemical measures: Wounds, 2009; 21(7); 177-82
34.. Karimi H, Motevalian SA, Rabbani A, Prediction of mortality in pediatric burn injuries: R-baux score to be applied in children (pediatrics-baux score): Iran J Pediatr, 2013; 23(2); 165-70
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250