27 April 2022: Articles 
Total Resorption of a Chronic L4-L5 Disc Extrusion After Application of the Atlasprofilax Method: A Case Report
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Unexpected drug reaction
José G. León12AB, Lluís Manent3BCF, Kathleen Lewis4DE, Orlando AnguloDOI: 10.12659/AJCR.935208
Am J Case Rep 2022; 23:e935208
Abstract
BACKGROUND: The intervertebral disc extrusion resorption has been described in the literature by various authors. It occurs in up to 75% of patients with symptomatic extruded lumbar discs. The Atlasprofilax method favors osteo-musculo-articular rehabilitation processes, mainly impacting on 2 levels: the first is the bone anatomy of the atlanto-occipital joint, and the second is the fasciae located in the cervical region.
CASE REPORT: A 42-year-old male patient diagnosed by MRI with dehydration of L2-L3 to L5-S1 intervertebral discs, disc bulging at L2-L3 and L3-L4, and disc extrusion at L4-L5, received a one-time neuromuscular treatment, called the Atlasprofilax method, to the suboccipital region. In a repeat MRI 6 months later, the disc extrusion at L4-L5 was totally resorbed and improvement in the L3-L4 and L4-L5 disc bulges was seen. The patient’s symptoms prior to the Atlasprofilax treatment included bilateral trapezius pain, right brachialgia, constant chronic low back pain, right sciatica, gait claudication, and paresthesia and dysesthesias in the lower limbs with associated pain and numbness in the calves. These symptoms were ameliorated after the treatment. The sciatica disappeared 1 week after the treatment and did not recur. In a follow-up 5 years later, the remaining symptoms had improved even further.
CONCLUSIONS: We propose that alterations of the cervical musculature and deep fascia could predispose to the development of lumbar disc abnormalities. We therefore also propose that improvements in this patient, both in symptoms and in imaging findings, are due to a reduction of the asymmetric distribution of forces and elastic loading as a result of the Atlasprofilax treatment.
Keywords: Cervical Atlas, Intervertebral Disc Displacement, Low Back Pain, Sciatica, Adult, Animals, Cattle, Graft vs Host Disease, Humans, intervertebral disc, intervertebral disc degeneration, Lumbar Vertebrae, Male
Background
Disc pathology generally is classified according to the degree of severity. From less to most severe, they are classified as: disc bulging, disc protrusion, disc extrusion, and disc sequestration [1]. MRI studies have shown that patients with symptomatic extruded lumbar discs who undergo repeated non-surgical conservative treatments can exhibit non-regression, partial regression, or complete resolution [2]. Complete resolution or resorption of extruded discs occur in 75% of such patients [2]. The numeric rating scale (NRS) or visual analog scale (VAS), which are positively correlated [3], are commonly used to assess improvement in disc extrusion-related pain. Some authors suggest that macrophage infiltration can play an important role in the reabsorption of extruded discs through chemokine mediation and other mechanisms in the chemotaxis of the neovascularized zone [4,5]. In other studies, sequestered discs seem to have a better outcome for re-absorption when compared to extruded discs. For example, a study found 67% improvement in clinical symptoms, as measured by the Oswestry low back pain disability questionnaire, straight leg raising test, and VAS, but only a 33.3% reduction in disc size as measured on serial magnetic resonance imaging (MRI) [6]. Other studies showed a 20% size decrease in subligamentous, transligamentous, and sequestered herniations of [7]. In some studies, reduction of disc herniation-associated symptoms was correlated with a reduction in the size of the extrusion or bulging [2], while in others this correlation was not observed [8].
According to a study by Kesikburun et al [2] on 40 patients with symptomatic extruded lumbar discs diagnosed by MRI, the average time for a complete reabsorption of extruded discs with repeated conservative treatment was around 17 months and included 75% of the cases. Rates of regression and resolution for extruded lumbar discs seems to be higher over a longer follow-up period. A study of 37 patients with an average follow-up time of 23.2 months [8] found that complete and sustained recovery of conservatively treated massive prolapsed discs was observed in 83% of patients, and there was an average reduction of 64% in volumetric disc size. Interestingly, there was a poor correlation between clinical improvement and the extent of disc resolution [8]. Komori et al [9] reported no complete resolution after a mean of 6.3 months follow-up time, but a partial reabsorption or regression was observed in 30.7% (8/26) of the patients. A study on 17 patients found that all patients with extruded disc herniation had a partial regression of more than half of the disc morphological size within a 2-year follow-up [10]. Thus, it seems that higher rates of regression and resolution of extruded lumbar disc herniation are correlated and can be achieved in accordance with the follow-up time. A metanalysis on the subject [11] found that disc sequestration had the highest rates of regression (even if not total reabsorption) with 96%, followed by 70% for disc extrusion, 41% for disc protrusion, and 13% for disc bulging, with a total reabsorption rate of 43% of sequestrated discs and 15% for extruded discs.
Nevertheless, and to the best of our knowledge, the available studies on partial or total regression of extruded herniated discs contain small samples of patients. Larger samples are required to elucidate the correlation between improvement of clinical symptoms and disc morphological size and disc regression. The role of time and the body’s natural mechanisms for disc regression with regard to nonsurgical conservative treatments or spontaneous regression also require elucidation.
Relapses or recurrent lower-extremity radicular pain after conservative nonsurgical treatment of lumbar disc herniation seem to occur quite frequently. Radicular pain relapses occur in about 25% of patients over 1 year after resolution of leg pain. The recurrence of back pain is even more common, occurring at a younger age and in 43% of the patients [12].
There are several conservative nonsurgical or minimally invasive treatments for the various types of herniated discs, ranging from corticosteroid injections and intradiscal ozone therapy to all types of physical therapy and myofascial manual manipulation techniques.
The Atlasprofilax method has an innovative approach, as it focuses on improving myofascial deformities in the atlanto-occipital hinge at a structural and metabolic level, usually in a single session. Suboccipital muscle deformities have been well-reported in the scientific literature in various pathologies such as whiplash-related disorders, chronic tension headache, and musculoskeletal disorders with associated pain, including those of non-traumatic origin [13–19]. Those muscles are also connected to the myodural bridge [20,21], a membrane that links the dura with the occiput, C1–C2, and the suboccipital muscles. Overstretching or chronic tension of the myodural bridge has been suggested to cause many ailments [20,22].
The craniocervical joint (CCJ) is a key factor in human biomechanics and posture, playing an important role as a co-factor in the development of some spine-related ailments and vertebral pathologies. In humans, standing influences the biomechanics of the CCJ via transfer of forces from the head through the transitional craniocervical hinge (including its bony and soft structures). These biomechanical forces differ from those in quadruped mammals, in which straight posture, spinal alignment, and integration of physical force vectors from the skull downward are not so relevant for the CCJ.
Complex sensorimotor feedback mechanisms are involved in maintaining the human standing position [23,24]. Certain suboccipital muscles play an important role in the proprioception necessary to maintain this posture [25,26]. A forward head position can influence the activation of the rectus capitis posterior muscles [27], causing a significant load-bearing of these muscles [30]. The rectus capitis posterior minor muscle is a proprioceptive monitor [26] involved in posture and balance. Trigger points and forward head posture can activate tension-type headaches [28]. The thoracic spine’s sagittal balance parameters and anatomic angles in the region of the lumbar spine are morphological predictors for distorted disc load [29]. Some studies have described a positive correlation between disc degeneration and multifidus muscle atrophy [30,31].
Thus, subclinical abnormalities and asymmetries at the CCJ level could lead to mechanical and metabolic alterations of the muscle and fascial continuum, affecting posture, muscle chains (such as the deep paravertebral muscles), vertebrae, and discs. This is because the deep posterior cervical fascia is interconnected with the thoracolumbar fascia in a structural and metabolic tridimensional network and, if deformed, can contribute to alterations and asymmetrical loads on muscle chains. This deformation could be a co-factor in predisposing certain discs to herniation.
All structures of the human body have a certain level of elasticity. Bones, cartilage, muscles, fascia, tendons, and ligaments have coefficients of elasticity. The coefficient of elasticity refers to the ability of a tissue to stretch and then return to its original length (hysteresis). Forward head posture changes the center of gravity of the skull and can result in irregular downward distribution of load. Structural asymmetries and metabolic abnormalities in the upper cervical myofascia due to this forward head translation or other factors also can contribute to distal muscle dysfunction and myofascial imbalance, including lumbar intervertebral discs. An MRI study found that lower lumbar level discs such as L4–L5 are more likely to present disc collapse and disruption [32], but their higher viscoelastic capacity compared to other intervertebral discs provides them with a higher capacity for resorption.
Thus, we preliminarily hypothesized that alteration of the suboccipital musculature and deep cervical fascia could be an important co-factor that predisposes to the development of lumbar disc herniations. Such alterations are little-considered and understudied (probably being subclinical in most cases). The principle of fascintegrity explains how such alterations at the cervical and suboccipital level could be transferred distally [33–35]. From this perspective, the extracellular matrix and its metabolism [36] could contribute to fascial deformities and abnormalities, affecting not only movement abilities of the spine and the limbs, but also leading to muscle and vertebral joint imbalance. Chronic asymmetrical overload and improperly directed downward vector forces could therefore predispose discs to bulging or even herniation.
Case Report
INTERVENTION:
The patient underwent the intervention by means of the Atlasprofilax method in a single session. The method involves working the myofascial structures of the neck with a device that uses the principles of mechano-transduction by vibropres-sure at specific frequencies.
The intervention consisted of a non-invasive neurostimulation with a special device that used controlled percussion vibropressure at special frequency with an adapted head that was applied during 8 min on several key points of the suboccipital area to stimulate certain muscle and fascial receptors aiming at a deep mechano-transduction effect on the suboccipital muscles.
ENDPOINTS:
The objective of the study had 2 purposes: observing imaging improvement reduction of the size and morphology of the herniated disc by means of MRI, and the associated clinical manifestations.
At the imaging level, variations in size and morphology of affected extruded discs were analyzed and taken as endpoints, to see if an improvement such as disc reabsorption was achieved.
At the clinical level, the differential result of pain according to the VAS was used as an endpoint to determine improvement of pain in trapezius, right brachialgia, lower back pain, right sciatica, and pain in both lower limbs. The PGIC scale was used to determine improvement in life quality and therapy outcome satisfaction for associated ailments such as pain in the trapezius, right brachialgia, lower back pain, right sciatica, pain in both lower limbs, paresthesia and dysesthesia in lower limbs, as well as numbness and stiffness in the calves.
RADIOLOGICAL FINDINGS:
Radiologist’s diagnosis prior to the application of the Atlasprofilax method was:
At L4, annular ligament tear and right posterolateral cephalic migrated disc extrusion, which contacts and compresses the thecal sac and probably the left L5 root in its lateral portion. At L5–S1, small diffuse disc bulge.”
The radiologist’s diagnosis 6 months after the application of the Atlasprofilax method was (Figure 2):“There is bulging of the annulus fibrosus of the intervertebral discs of L3–L4 and L4–L5 with presence of tearing of the annulus fibrosus in the posterior aspect of the intervertebral disc of L4–L5, this bulging associated with fascicular degenerative changes moderately decreases the width of the spinal canal in these locations, without relevant associated narrow, central, or lateral canal. The right paracentral disc herniation visualized in the previous study is not observed and the width of the spinal canal has improved for this reason in this location. Currently, the right paracentral disc herniation L4–L5 visualized in the previous study is not observed. In the present study there is bulging of the fibrous ring L3–L4 and L4–L5 with moderate decrease in the amplitude of the spinal canal, which, however, has improved with respect to the previous study.”
CLINICAL FINDINGS:
A clear improvement was observed in the reduction of pain using the VAS as well as in the perception of the favorable impact of the intervention on quality of life according to the PGIC scale as presented in Tables 1 and 2.
Discussion
The case described here reports a rapid resorption of a disc extrusion after the application of the neuromuscular Atlasprofilax method (Figure 3). The resorption of this disc extrusion could be due to spontaneous remission within the parameters observed in other studies of similar cases of disc extrusion. However, it is interesting to note that despite the chronicity and severity of the patient’s described symptoms – correlated and consistent with the disc herniation, with an onset of more than 5 years – such spontaneous regression would have occurred much earlier, since spontaneous regressions occur at 4 months to 2 years after herniation. It is therefore feasible to conclude that the Atlasprofilax therapy could have contributed to the reabsorption. Further studies with larger sample sizes are required to answer this question. From a clinical point of view, it is noteworthy that none of the patient’s symptoms had improved in the 5 years prior to the Atlasprofilax therapy. The sciatica disappeared within 1 week after the treatment, and symptoms not directly related to the disc herniation (eg, brachialgia and trapezius pain) improved significantly shortly after therapy. The symptoms associated with the disc extrusion and those with other origins were greatly reduced, and mostly disappeared, over a period of 5 years. No relapse or recurrence occurred within the 5 years of the study, despite the patient regularly practicing high-impact activities such as Taekwondo. This is interesting since recurrence of radicular pain (25%) and lower back pain (43%) associated with a herniated disc are relatively common after nonsurgical conservative treatment. These recurrences are common and persist in younger people, as in the age group of this patient. The Atlasprofilax method has been shown to be an effective method in reducing pain and improving quality of life in patients with fibromyalgia [41], temporo-mandibular joint-associated disorders, and cervico-brachialgia disorders [42,43]. This case report agrees with previous studies and case reports, broadening preliminary the use of the Atlasprofilax method for herniated discs and their associated ailments.
Conclusions
The hypothesis that abnormalities in the deep suboccipital musculature, deep cervical fascia, and upper cervical spine soft structures that exhibit morpho-pathologic correlations with many other pathologies are probable preliminary co-factors that may predispose to or cause disc herniations should be a candidate for further clinical consideration and extensive studies. The involvement of the fascial continuum and its downward impact on paravertebral muscle chains with possible chronic asymmetrical overload on intervertebral discs should also be investigated in the case of lumbar disc herniations to elucidate its role and, if applicable, its probable pathophysio-logic mechanism. The Atlasprofilax method, being an innovative, non-invasive, and conservative approach, could be preliminarily proposed as a candidate for further study and more clinical therapeutic attention.
Figures
References:
1.. Fardon DF, Milette PC, Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology: Spine (Phila Pa 1976), 2001; 26(5); E93-113
2.. Kesikburun B, Eksioglu E, Turan A, Spontaneous regression of extruded lumbar disc herniation: Correlation with clinical outcome: Pak J Med Sci, 2019; 35(4); 974-80
3.. Shafshak TS, Elnemr R, The Visual Analogue Scale versus Numerical Rating Scale in measuring pain severity and predicting disability in low back pain: J Clin Rheumatol, 2021; 27(7); 282-85
4.. Haro H, Shinomiya K, Komori H, Upregulated expression of chemokines in herniated nucleus pulposus resorption: Spine (Phila Pa 1976), 1996; 21(14); 1647-52
5.. Kato T, Haro H, Komori H, Shinomiya K, Sequential dynamics of inflammatory cytokine, angiogenesis inducing factor and matrix degrading enzymes during spontaneous resorption of the herniated disc: J Orthop Res, 2004; 22(4); 895-900
6.. Ahn SH, Park HW, Byun WM, Comparison of clinical outcomes and natural morphologic changes between sequestered and large central extruded disc herniations: Yonsei Med J, 2002; 43(3); 283-90
7.. Ahn SH, Ahn MW, Byun WM, Effect of the transligamentous extension of lumbar disc herniations on their regression and the clinical outcome of sciatica: Spine (Phila Pa 1976), 2000; 25(4); 475-80
8.. Benson RT, Tavares SP, Robertson SC, Conservatively treated massive prolapsed discs: A 7-year follow-up: Ann R Coll Surg Engl, 2010; 92(2); 147-53
9.. Komori H, Okawa A, Haro H, Contrast-enhanced magnetic resonance imaging in conservative management of lumbar disc herniation: Spine (Phila Pa 1976), 1998; 23(1); 67-73
10.. Takada E, Takahashi M, Shimada K, Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome: J Orthop Surg (Hong Kong), 2001; 9(1); 1-7
11.. Chiu CC, Chuang TY, Chang KH, The probability of spontaneous regression of lumbar herniated disc: A systematic review: Clin Rehabil, 2015; 29(2); 184-95
12.. Suri P, Rainville J, Hunter DJ, Recurrence of radicular pain or back pain after nonsurgical treatment of symptomatic lumbar disk herniation: Arch Phys Med Rehabil, 2012; 93(4); 690-95
13.. Fernández-de-Las-Peñas C, Cuadrado ML, Arendt-Nielsen L, Association of cross-sectional area of the rectus capitis posterior minor muscle with active trigger points in chronic tension-type headache: A pilot study: Am J Phys Med Rehabil, 2008; 87(3); 197-203
14.. Andary MT, Hallgren RC, Greenman PE, Rechtien JJ, Neurogenic atrophy of suboccipital muscles after a cervical injury: A case study: Am J Phys Med Rehabil, 1998; 77(6); 545-49
15.. Elliott J, Jull G, Noteboom JT, Darnell R, Fatty infiltration in the cervical extensor muscles in persistent whiplash-associated disorders: A magnetic resonance imaging analysis: Spine (Phila Pa 1976), 2006; 31(22); E847-55
16.. Elliott JM, Pedler AR, Jull GA, Differential changes in muscle composition exist in traumatic and nontraumatic neck pain: Spine (Phila Pa 1976), 2014; 39(1); 39-47
17.. Yuan XY, Yu SB, Liu C, Correlation between chronic headaches and the rectus capitis posterior minor muscle: A comparative analysis of cross-sectional trail: Cephalalgia, 2017; 37(11); 1051-56
18.. McPartland JM, Brodeur RR, Hallgren RC, Chronic neck pain, standing balance, and suboccipital muscle atrophy – a pilot study: J Manipulative Physiol Ther, 1997; 20(1); 24-29
19.. Hallgren RC, Greenman PE, Rechtien JJ, Atrophy of suboccipital muscles in patients with chronic pain: A pilot study: J Am Osteopath Assoc, 1994; 94(12); 1032-38
20.. Enix DE, Scali F, Pontell ME, The cervical myodural bridge, a review of literature and clinical implications: J Can Chiropr Assoc, 2014; 58(2); 184-92
21.. Kahkeshani K, Ward P, Connection between the spinal dura mater and sub-occipital musculature: Evidence for the myodural bridge and a route for its dissection – a review: Clin Anat, 2012; 25; 415-22
22.. Hallgren RC, Hack GD, Lipton JA, Clinical implications of a cervical myodural bridge: American Osteopathic Association Journal, 1997; 7(4); 30-34
23.. Martin JP, A short essay on posture and movement: J Neurol Neurosurg Psychiatry, 1977; 40(1); 25-29
24.. Peterka RJ, Loughlin PJ, Dynamic regulation of sensorimotor integration in human postural control: J Neurophysiol, 2004; 91(1); 410-23
25.. Hallgren RC, Rowan JJ, Implied evidence of the functional role of the rectus capitis posterior muscles: J Am Osteopath Assoc, 2020; 120(6); 395-403
26.. McPartland JM, Brodeur RR, Rectus capitis posterior minor: A small but important suboccipital muscle: Journal of Bodywork and Movement Therapies, 1999; 3(1); 30-35
27.. Hallgren RC, Pierce SJ, Sharma DB, Rowan JJ, Forward head posture and activation of rectus capitis posterior muscles: J Am Osteopath Assoc, 2017; 117(1); 24-31
28.. Fernández-de-las-Peñas C, Alonso-Blanco C, Cuadrado ML, Trigger points in the suboccipital muscles and forward head posture in tension-type headache: Headache, 2006; 46(3); 454-60
29.. Keller TS, Colloca CJ, Harrison DE, Influence of spine morphology on intervertebral disc loads and stresses in asymptomatic adults: Implications for the ideal spine: Spine J, 2005; 5(3); 297-309
30.. Sun D, Liu P, Cheng J, Correlation between intervertebral disc degeneration, paraspinal muscle atrophy, and lumbar facet joints degeneration in patients with lumbar disc herniation: BMC Musculoskelet Disord, 2017; 18(1); 167
31.. Liu C, Xue J, Liu J, Is there a correlation between upper lumbar disc herniation and multifidus muscle degeneration? A retrospective study of MRI morphology: BMC Musculoskelet Disord, 2021; 22(1); 92
32.. Gutiérrez RAG, Alonso VR, Rosas JGZ, Biomechanics of the intervertebral disc in compression: Experimental and numerical study: Journal of Mechanics Engineering and Automation, 2015; 5(1); 39-44
33.. Schleip R, Huijing P, Findlay TW: Fascia: The Tensional Network of the Human Body: The science and clinical applications in manual and movement therapy, 2012, London, UK, Churchill Livingstone
34.. Adstrum S, Hedley G, Schleip R, Defining the fascial system: J Bodyw Mov Ther, 2017; 21(1); 173-77
35.. Pilat A: Myofascial therapies: Myofascial induction, 2003, Madrid, Spain, Mcgraw Hill Interamericana De Espana SL [in Spanish]
36.. Wang HQ, Li XK, Wu ZX, The effect on the extracellular matrix of the deep fascia in response to leg lengthening: BMC Musculoskelet Disord, 2008; 9; 101
37.. Mahmoud W, Effect of neural mobilization versus spinal manipulation in patients with radicular chronic low back pain: European Journal of Scientific Research, 2015; 131; 122-32
38.. Rampakakis E, Ste-Marie PA, Sampalis JS, Real-life assessment of the validity of patient global impression of change in fibromyalgia: RMD Open, 2015; 1(1); e000146
39.. Leemann S, Peterson CK, Schmid C, Outcomes of acute and chronic patients with magnetic resonance imaging-confirmed symptomatic lumbar disc herniations receiving high-velocity, low-amplitude, spinal manipulative therapy: A prospective observational cohort study with one-year follow-up: J Manipulative Physiol Ther, 2014; 37(3); 155-63
40.. Peterson CK, Pfirrmann CW, Hodler J, Are Modic changes related to outcomes in lumbar disc herniation patients treated with imaging-guided lumbar nerve root blocks?: Eur J Radiol, 2014; 83(10); 1786-92
41.. Malagón J, Villaveces M, Manent L, A therapeutic alternative in the management of fibromyalgia: Revista Cuarzo, 2017; 23; 30
42.. León JG, Manent L, Lewis K, Angulo O, Clinical and imaging improvement after the atlasprofilax method in a patient with cervicobrachial syndrome and temporomandibular joint disorders. A case report: Acta Scientific Orthopaedics, 2021; 4(10); 92-102
43.. Gutiérrez Navas VE, [Effect of Atlasprofilax® therapy on symptoms related to temporomandibular dysfunction, bruxism and the relationship of dental midlines]: UstaSalud, 2013; 12(2); 124-33 [in Spanish]
Figures
Tables
 Table 1.. VAS results for pain pre-treatment, 6 months after treatment and 60 months after treatment.
Table 1.. VAS results for pain pre-treatment, 6 months after treatment and 60 months after treatment.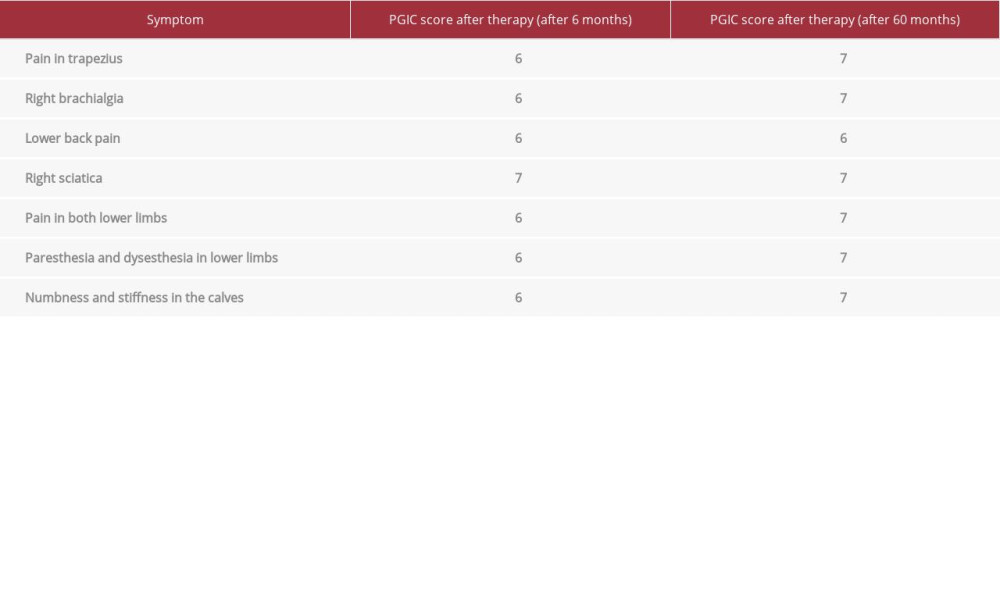 Table 2.. PGIC scores 6 months and 60 months after therapy.
Table 2.. PGIC scores 6 months and 60 months after therapy. Table 1.. VAS results for pain pre-treatment, 6 months after treatment and 60 months after treatment.
Table 1.. VAS results for pain pre-treatment, 6 months after treatment and 60 months after treatment.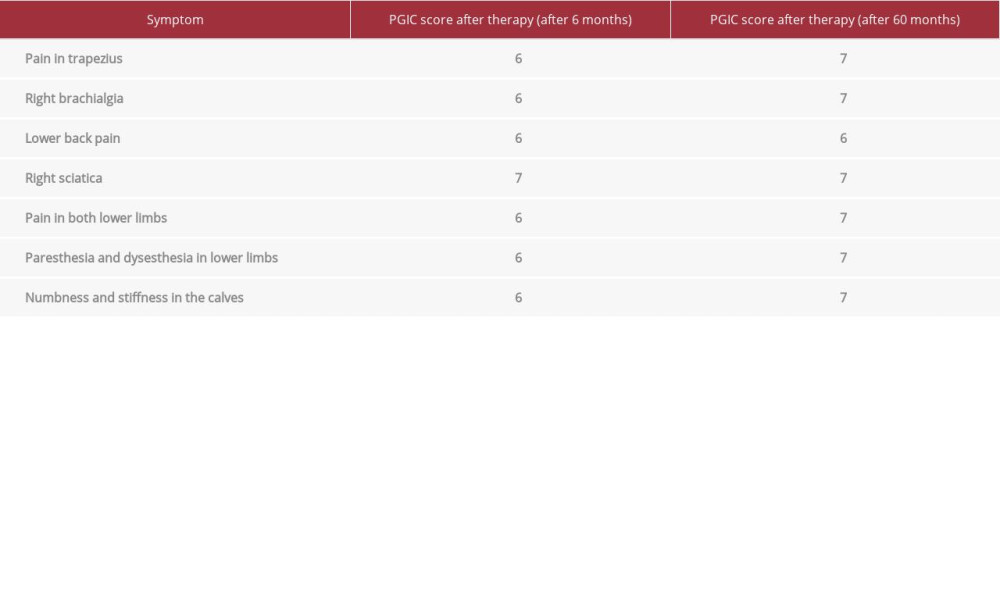 Table 2.. PGIC scores 6 months and 60 months after therapy.
Table 2.. PGIC scores 6 months and 60 months after therapy. In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








