23 October 2020: Articles 
Amiodarone Toxicity Presenting with Acute Onset of Systemic Inflammatory Response Syndrome and Multiorgan Failure Mimicking Sepsis
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Adverse events of drug therapy, Rare coexistence of disease or pathology
Irfanali R. Kugasia1ABCDEF*, Mohsin Ijaz1CDE, Ahsan Khan1BC, Yashwanth Jasti2FGDOI: 10.12659/AJCR.926929
Am J Case Rep 2020; 21:e926929
Abstract
BACKGROUND: Amiodarone, an anti-arrhythmic medication, has been associated with the development of multiple organ toxicities. Most of these toxicities develop insidiously. However, in rare cases, these toxicities manifest with more acute symptoms. We present an unusual case of amiodarone toxicity which manifested with multiorgan failure and systemic inflammatory response syndrome that mimicked sepsis.
CASE REPORT: A 73-year-old man who was being treated with chronic oral amiodarone for atrial fibrillation presented with flu-like symptoms and fever, pulmonary infiltrate, acute kidney injury, and thrombocytopenia. The patient did not improve with antibiotics and fluid resuscitation. The results of an extensive infectious and non-infectious workup were negative. His symptoms worsened during hospitalization, which correlated with the loading of intravenous amiodarone given for his acute worsening of atrial fibrillation. Amiodarone-induced drug toxicity was contemplated by the treating medical team. Amiodarone was stopped, and the patient was treated with steroids, which improved his symptoms and organ dysfunctions. Subsequent bronchoscopy with lung biopsy showed foamy macrophages with organizing pneumonia and fibrinoid changes.
CONCLUSIONS: This case highlights an atypical and rare presentation of a complication of chronic amiodarone use that presented with acute onset of fever, systemic inflammatory response syndrome, and multiorgan failure masquerading as sepsis. The patient’s symptoms and organ dysfunctions improved with the discontinuation of amiodarone and institution of steroids.
Keywords: amiodarone, Fever, Multiple Organ Failure, Anti-Arrhythmia Agents, Sepsis, Systemic Inflammatory Response Syndrome
Background
Amiodarone is one of the most effective anti-arrhythmic medications used to treat a wide range of arrhythmias. It was introduced in the 1960s and is now the most popular anti-ar-rhythmic drug in use [1]. Amiodarone has been commonly associated with the development of various organ toxicities. Onset of these toxicities is typically insidious and correlates with the cumulative dose of amiodarone [2]. Although rare, the acute onset of toxicities has been described with either the chronic use or initiation of amiodarone [3–7]. Herein, we describe an unusual case of amiodarone toxicity that presented with acute onset of fever, multiorgan failure, and systemic inflammatory response syndrome that masqueraded as sepsis from a low cumulative dose of approximately 75 g.
Case Report
A 73-year-old man presented to our hospital in February 2020 with fever and flu-like symptoms of body aches, fatigue, and malaise for 10 days. This was associated with diffuse non-localized abdominal pain with nausea and vomiting for 3 days prior to hospitalization. The patient denied dyspnea or cough. He also denied any recent travel, family gatherings, or sick contacts. He endorsed an active lifestyle and attended the gym daily prior to getting sick.
The patient’s past medical history was significant for a difficult-to-control atrial flutter/fibrillation, which had been treated with dronedarone since 2016. The dronedarone was switched to amiodarone in March 2019 after the recurrence of atrial fibrillation with a rapid ventricular rhythm. The patient was started on a loading dose of oral amiodarone of 400 mg daily for 1 month, and after undergoing direct current cardioversion, he was switched to oral amiodarone 200 mg daily; he had a cumulative dose of approximately 75 g at the time of hospitalization. The patient denied smoking or any history of lung disease. His other oral medications included apixaban 5 mg orally twice daily, tamsulosin 0.4 mg once daily, and finasteride 5 mg once daily. The patient denied any recent change in his amiodarone dose. He also denied taking any over-the-counter medications or herbal supplements.
On initial presentation, the patient was noted to have fever, atrial fibrillation with rapid ventricular rate, warm extremities, and low systolic blood pressure, but with a mean arterial pressure consistently greater than 65 mmHg. He was mildly tachypneic, with stable oxygen saturation at more than 95% on room air. The patient’s significant laboratory findings on presentation are summarized in Table 1. In brief, laboratory evaluation showed a negative rapid influenza antigen test, normal absolute white blood cell count with significant bandemia of 35%, severe lymphopenia with an absolute lymphocyte count 50/uL, and thrombocytopenia of 50 000/uL. Urinalysis results showed moderate bacteriuria without leukocyte esterase or nitrites. Blood chemistry results showed elevated BUN/creatinine levels of 13.5/0.16 mmol/L, elevated AST and ALT levels of 193 U/L and 186 U/L, respectively, and total bilirubin of 27.4 µmol/L. The procalcitonin level was 3.65 ng/ml, and TSH was 2.27 uIU/ml. The other laboratory values were non-contributory. The chest X-ray showed a new consolidation of the left upper lung (Figure 1A, 1B).
The patient was started on intravenous ceftriaxone 2 g daily for presumed sepsis of pulmonary origin and fluid resuscitation with a total of 3 L of crystalloids. His oral amiodarone was continued to help control his atrial fibrillation and apixaban was discontinued because of his thrombocytopenia.
Over the next 48 h, the patient continued to have high-grade fever without much improvement in clinical status (Figure 2, Table 2). Repeated laboratory test results showed increasing BUN and creatinine levels, increasing leukocytosis, persistent bandemia ranging from 38% to 58%, and persistent thrombocytopenia (Figure 2, Table 1). The patient’s 2 sets of peripheral blood cultures, respiratory multiplex real-time polymerase chain reaction (RT-PCR, Table 3), urine culture, and HIV test were negative. A chest computed tomography (CT) scan without contrast showed dense consolidation with surrounding ground-glass opacification in the left upper lobe of the lung with small bilateral pleural effusions and mediastinal lymphadenopathy, favoring reactive enlargement. Radiographic findings favored pneumonia (Figure 1C). A CT scan of the abdomen and pelvis without contrast showed mild nonspecific splenomegaly, minimal sludge in the gallbladder without evidence of acute cholecystitis, colonic diverticulosis without evidence of acute diverticulitis, and no other acute abnormalities. No hyperdensity or increased attenuation of the liver or spleen was reported.
Due to the patient’s persistent fevers and nonresolving symptoms after 48 h of presentation, the antibiotic regimen was escalated to intravenous piperacillin/tazobactam 4.5 g every 6 h and a nasal swab for a SARS-CoV-2 was sent for PCR testing. At 72 h after admission, the patient was given a loading dose of amiodarone with a 150-mg intravenous push followed by an intravenous infusion of 1 mg/h for 6 h and 0.5 mg/h for 18 h, to control his worsening tachycardia with atrial fibrillation. Beta blockers and calcium channel blockers were avoided owing to his hypotension. Subsequently, his fevers, leukocytosis, and creatinine levels worsened exponentially (Figure 2A, 2B), with a Tmax of 39.9°C. This was associated with worsening nausea and vomiting, along with an increasingly toxic appearance and delirium.
After consultation with an infectious disease specialist and ruling out of other differential diagnoses as mentioned in Table 4, drug-induced fever and pulmonary toxicity from amiodarone was considered as the potential cause of the patient’s symptoms. Amiodarone and piperacillin/tazobactam infusions were discontinued. Bronchoscopy was planned but delayed because the patient’s SARS-CoV-2 PCR test results were pending. In the interim, the patient was started on 1 mg/kg of intravenous methylprednisolone empirically because of his severe symptoms.
Within 12 h of starting systemic steroids, the patient’s fever, tachypnea, delirium, platelet count, and creatinine level started improving, and normalized in the next 48 h (Figure 2). The SARS-CoV-2 PCR test result was negative. Because of the improving blood pressure, metoprolol was started orally at 25 mg twice daily to control the ventricular rate from atrial fibrillation. On day 6 of hospitalization, the patient underwent bronchoscopy with bronchoalveolar lavage from the left upper lobe with transbronchial lung biopsies to obtain a definitive diagnosis and rule out malignancy and atypical fungal, mycobacterial, and viral infection. The cell count on bronchoalveolar lavage showed 26% lymphocytes and 13% neutrophils, with the rest being monocyte-histiocytes. Lung biopsies revealed focal organizing fibrin in air spaces, consistent with organizing pneumonia and foamy macrophages (Figure 3). All cultures from the bronchoscopy and biopsies were negative for bacteria, fungus, and acid-fast bacilli. Biopsies from the consolidation were negative for any malignant cells. The bronchoalveolar lavage specimen was also negative for respiratory multiplex RT-PCR.
The patient was discharged home on oral prednisone 40 mg once daily, metoprolol 100 mg twice daily, and apixaban 5 mg twice daily. Amiodarone was discontinued. Over the next 6 weeks, prednisone was slowly tapered off without any recurrence of symptoms, and a follow-up chest CT scan at week 6 showed complete resolution of the consolidation. The patient’s atrial fibrillation remained well controlled with oral metoprolol.
Discussion
The adverse effects of amiodarone include corneal microdeposits (seen in >90% of patients), optic neuritis (1%), photosensitivity (25–75%), skin discoloration (<10%), hypothyroidism (4– 22%), hyperthyroidism (2–12%), pulmonary toxicity(2%), and hepatotoxicity ranging from elevated transaminase levels in 15–30% of patients to the development of hepatitis and cirrhosis in <3% of patients [1]. Most of these complications develop insidiously. The primary determinants for the development of severe toxicities to amiodarone are the daily dose, duration of treatment, and cumulative dose of the drug [2]. For example, clinically significant amiodarone-induced pulmonary toxicity is commonly seen in patients who are on 400 mg of amiodarone daily for more than 2 months, 200 mg daily for more than 2 years [2,8], or have a cumulative dose of approximately 140–230 g [9]. Due to its high lipid solubility, amiodarone has a large volume of distribution and tends to accumulate in tissues with high lipid content and high blood flow such as the lungs, liver, spleen, skin, and adipose tissue [8]. This gives amiodarone a prolonged half-life that can range from 15 to 142 days and depends on factors including the age of the patient, total cumulative dose, and fat content of the body. As a result, amiodarone’s toxicities can persist long after the discontinuation of exogenous intake [2,10,11]. There is also a poor correlation between blood amiodarone levels and development of toxicities due to its tendency to accumulate in certain tissues and subsequent slow continuous release from those tissues [1,2]. The development of amiodarone toxicity is thought to be through direct toxicity from the accumulation of phospholipids due to its inhibition of lysosomal phospholipase A. It can also directly increase oxidative free radical production in the organs in which it accumulates. Amiodarone is also proposed to cause systemic toxicity indirectly through the activation of an inflammatory response, but the mechanism of activation of the inflammatory response is not known [12,13].
Amiodarone-induced toxicities are primarily identified by diagnosis of exclusion. In the presented case, a multitude of other etiologies for the patient’s symptoms and organ dysfunctions were considered and ruled out by extensive, systematic evaluation before amiodarone drug toxicity was presumed. These are summarized in Table 4. Although the patient clinically improved with the discontinuation of amiodarone and administration of empiric systemic steroids, there was a lack of a definitive diagnosis of amiodarone toxicity. As a result, the decision was made to perform bronchoscopy since there remained a remote possibility of atypical infections and non-infectious etiologies, such as lymphoma and lung malignancy, which could potentially have a similar presentation. Additionally, a presumptive diagnosis of amiodarone-induced drug toxicity would have long-term implications on the choice of future anti-arrhythmic medications for the patient. The patient underwent bronchoscopy with bronchoalveolar lavage and biopsies which were all negative for any alternate diagnosis.
Organizing pneumonia diagnosed on transbronchial lung biopsies is a rare manifestation of amiodarone-induced pulmonary toxicity, which can be associated with fevers and malaise [14]. However, the patient’s fever curve acutely worsened with intravenous amiodarone, which should not have occurred if the fevers were only secondary to the organizing pneumonia (Figure 1). Also, the other organ dysfunctions seen in this case have not been previously reported with organizing pneumonia [14,15]. This portends a systemic inflammatory response in which organizing pneumonia was one of its manifestations rather than its cause.
Acute toxicities from amiodarone are rare, but have been documented [3–7,9–11]. In the case of our patient, acute toxicity from amiodarone was the most likely explanation for the constellation of fever, organizing pneumonia, acute kidney injury, thrombocytopenia, and the other clinical symptoms seen. Systemic steroids, although nonspecific, have been described in the literature for treating severe amiodarone-induced pulmonary toxicities, with a good response in most cases [2,10,11]. The conventional wisdom is to taper the systemic steroids over weeks to months to avoid recurrence of toxicity symptoms due to amiodarone’s extended half-life [2,10,11].
From a review of the English-language literature in PubMed from 1980 to 2020, we believe the presented case report is the first amiodarone toxicity presenting with acute onset of systemic inflammatory response syndrome with constellations of fever and multiple organ dysfunctions.
Conclusions
This case highlights a novel presentation of acute toxicity from long-term amiodarone therapy. Through this case, we would like to inform other clinicians that chronic low-dose amiodarone can cause toxicities that present acutely with multiple organ dysfunctions, which could masquerade as sepsis. And if these toxicities are severe, we recommend clinicians consider using systemic steroids to help reverse such toxicities.
Figures
Tables
Table 1.. Pertinent laboratory values with reference ranges.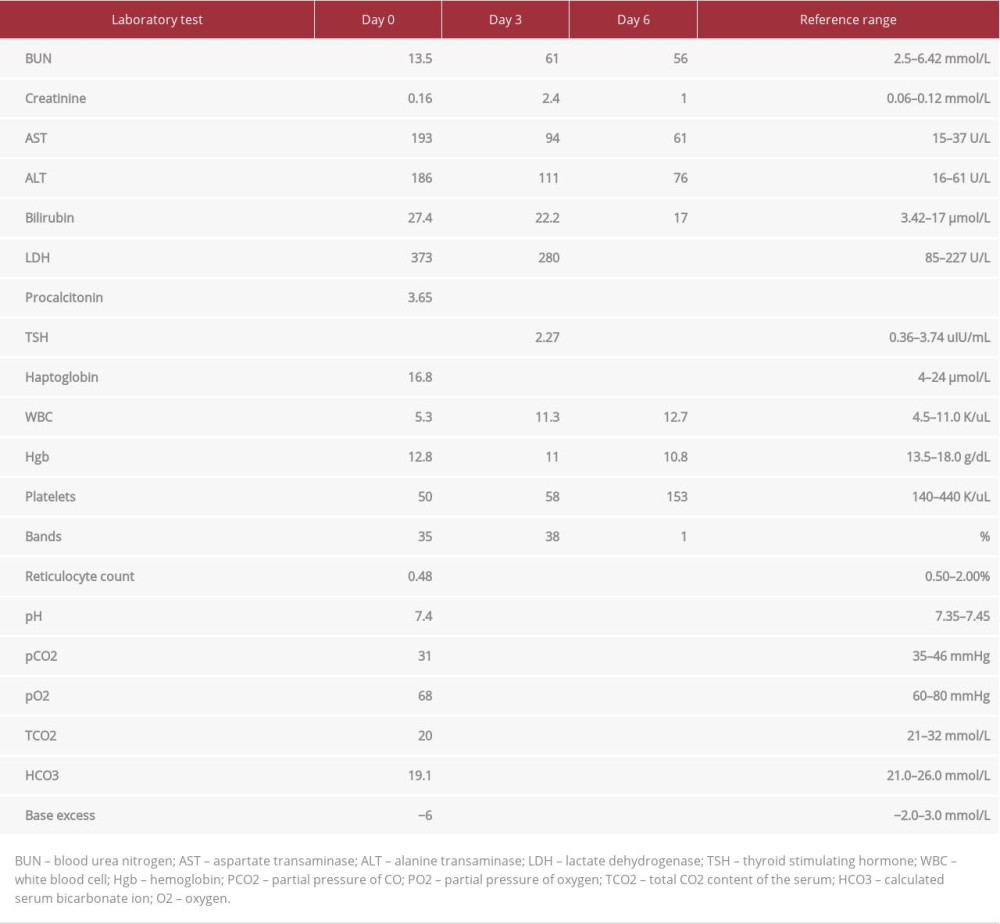 Table 2.. Vital signs during the first 5 days.
Table 2.. Vital signs during the first 5 days. Table 3.. Respiratory infective organism ruled out with the respiratory multiplex real-time polymerase chain reaction.
Table 3.. Respiratory infective organism ruled out with the respiratory multiplex real-time polymerase chain reaction.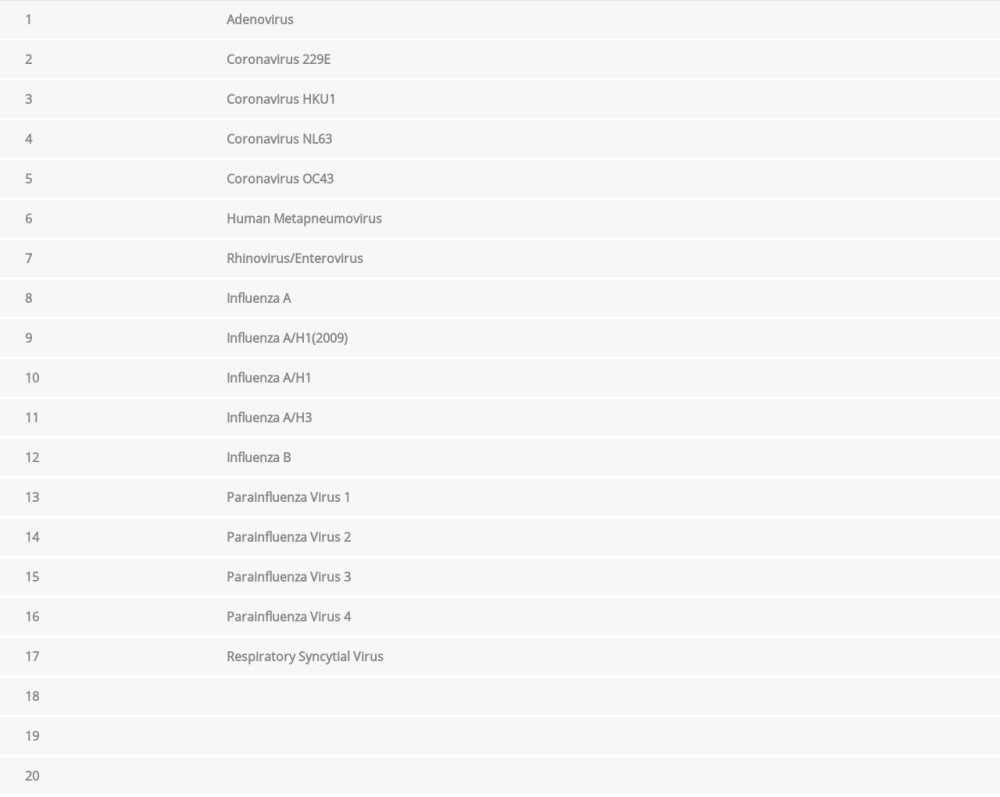 Table 4.. Differential diagnoses considered as the possible cause of patient’s clinical symptoms and tests done to rule them out.
Table 4.. Differential diagnoses considered as the possible cause of patient’s clinical symptoms and tests done to rule them out.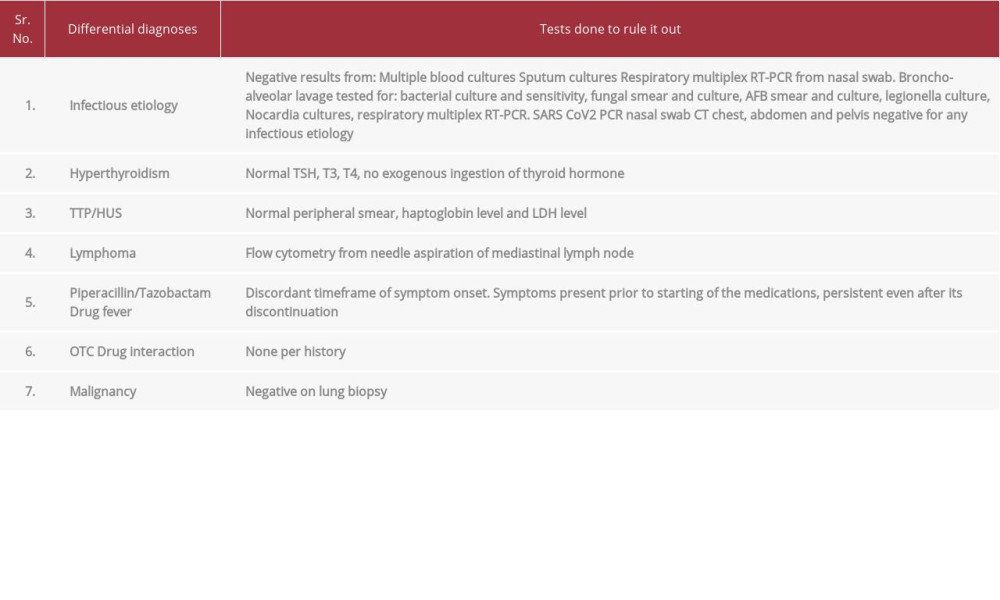
References:
1.. Epstein AE, Olshansky B, Naccarelli GV, Practical management guide for clinicians who treat patients with amiodarone: Am J Med, 2016; 129(5); 468-75
2.. Colunga Biancatelli RM, Congedo V, Calvosa L, Adverse reactions of Amiodarone: J Geriatr Cardiol, 2019; 16(7); 552-66
3.. Ott MC, Khoor A, Leventhal JP, Pulmonary toxicity in patients receiving low-dose amiodarone: Chest, 2003; 123(2); 646-51
4.. Lardinois D, Handschin A, Weder W, Acute amiodarone-induced pulmonary toxicity after lung operation: Ann Thorac Surg, 2002; 73(6); 2033-34
5.. Kaushik S, Hussain A, Clarke P, Lazar HL, Acute pulmonary toxicity after low-dose amiodarone therapy: Ann Thorac Surg, 2001; 72(5); 1760-61
6.. Abuzaid A, Saad M, Ayan M, Acute amiodarone pulmonary toxicity after drug holiday: A case report and review of the literature: Case Rep Cardiol, 2015; 2015; 927438
7.. Paudel R, Dogra P, Suman S, Acute liver and renal failure: A rare adverse effect exclusive to intravenous amiodarone: Case Rep Crit Care, 2016; 2016; 5232804
8.. Wolkove N, Baltzan M, Amiodarone pulmonary toxicity: Can Respir J, 2009; 16(2); 43-48
9.. Cheng HC, Wang JH, Wang ML, Adverse effect of low-dose amiodarone mimicking pulmonary malignancy: Int J Angiol, 2010; 19(1); e51-53
10.. Nacca N, Bhamidipati CM, Yuhico LS, Severe amiodarone induced pulmonary toxicity: J Thorac Dis, 2012; 4(6); 667-70
11.. Ashrafian H, Davey P, Is amiodarone an underrecognized cause of acute respiratory failure in the ICU?: Chest, 2001; 120(1); 275-82
12.. Martin WJ, Rosenow EC, Amiodarone pulmonary toxicity. Recognition and pathogenesis (Part I): Chest, 1988; 93(5); 1067-75
13.. Martin WJ, Rosenow EC, Amiodarone pulmonary toxicity. Recognition and pathogenesis (Part 2): Chest, 1988; 93(6); 1242-48
14.. Cordier JF, Cryptogenic organising pneumonia: Eur Respir J, 2006; 28(2); 422-46
15.. Epler GR, Drug-induced bronchiolitis obliterans organizing pneumonia: Clin Chest Med, 2004; 25(1); 89-94
Figures
Tables
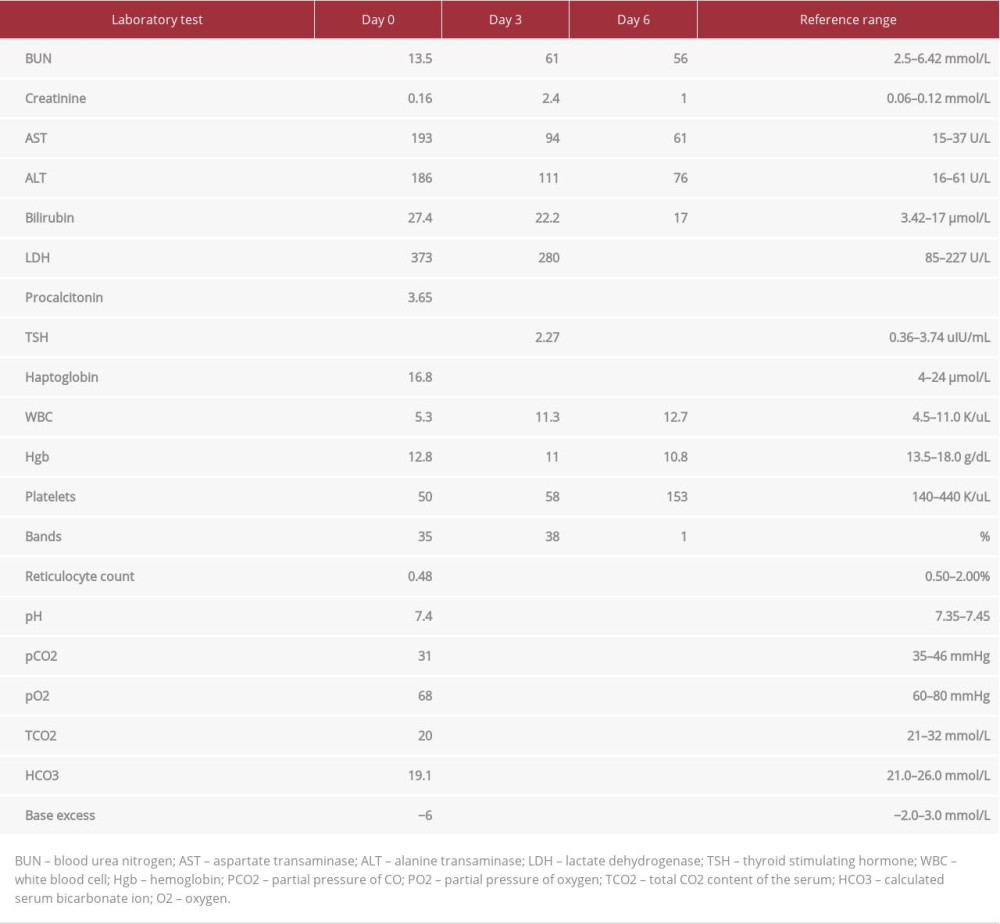 Table 1.. Pertinent laboratory values with reference ranges.
Table 1.. Pertinent laboratory values with reference ranges. Table 2.. Vital signs during the first 5 days.
Table 2.. Vital signs during the first 5 days.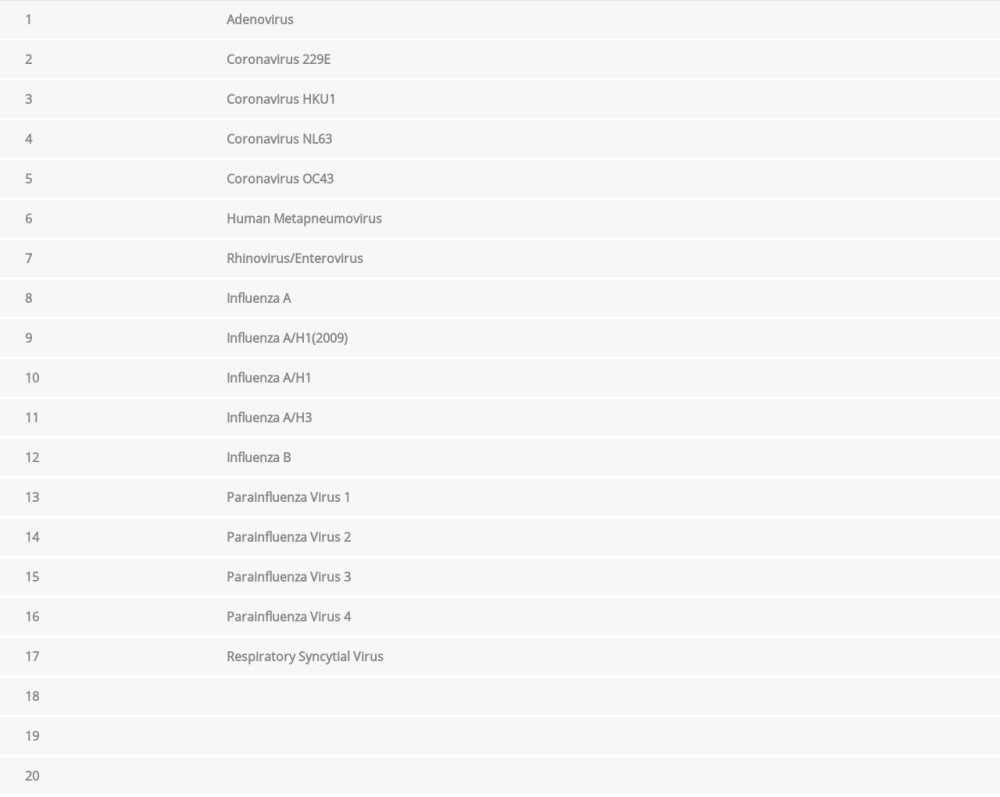 Table 3.. Respiratory infective organism ruled out with the respiratory multiplex real-time polymerase chain reaction.
Table 3.. Respiratory infective organism ruled out with the respiratory multiplex real-time polymerase chain reaction.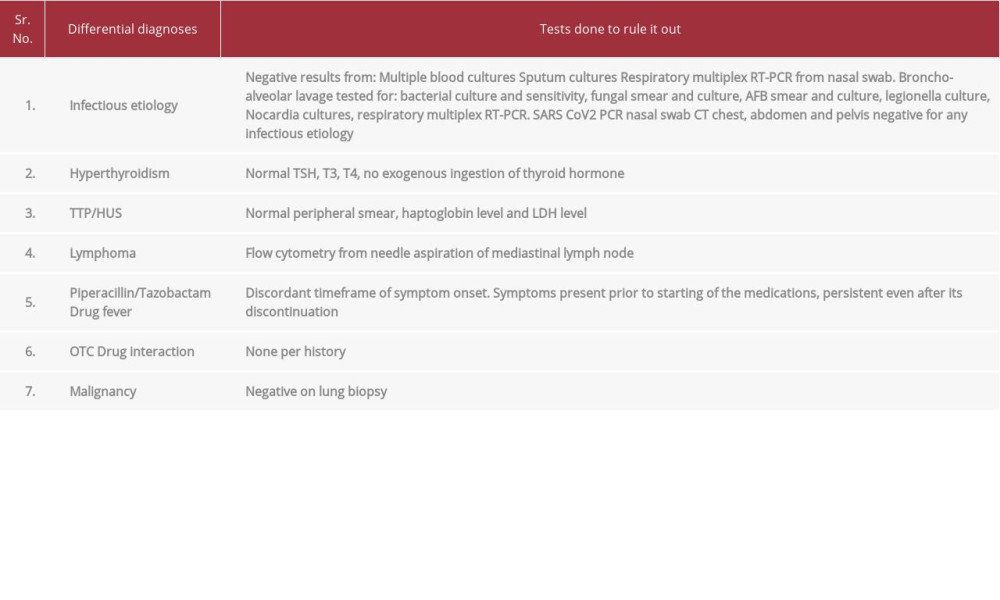 Table 4.. Differential diagnoses considered as the possible cause of patient’s clinical symptoms and tests done to rule them out.
Table 4.. Differential diagnoses considered as the possible cause of patient’s clinical symptoms and tests done to rule them out.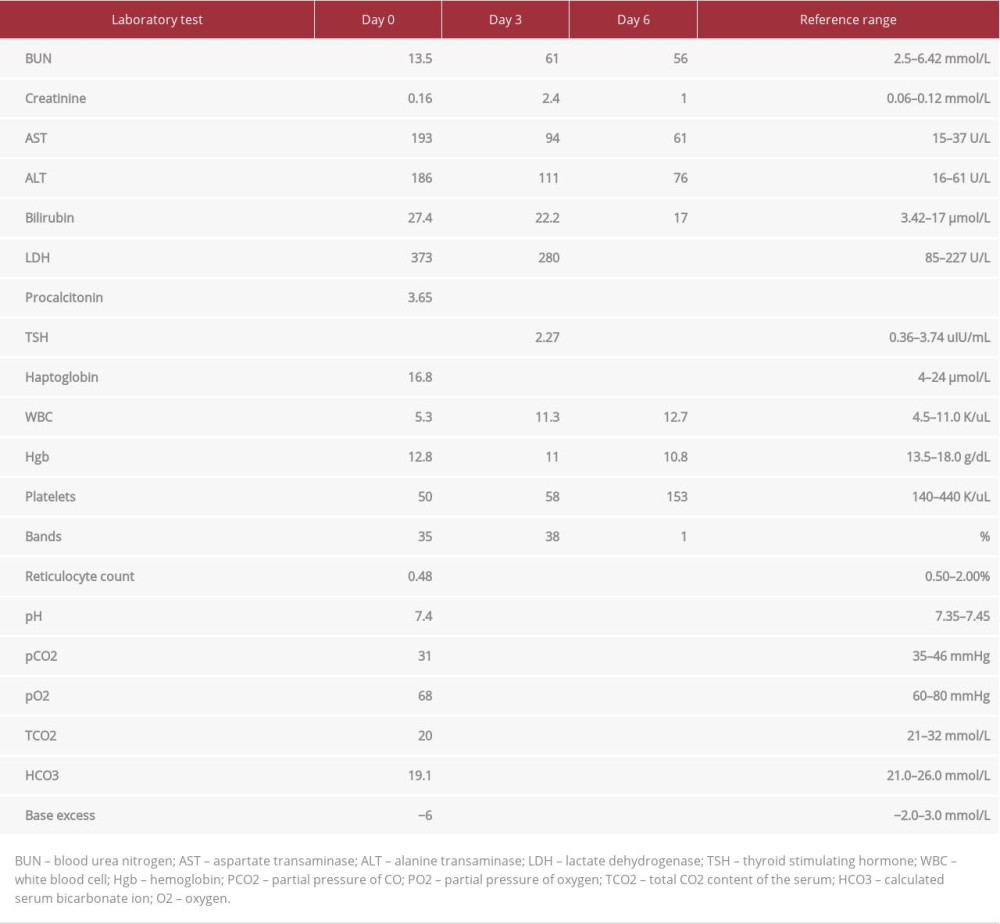 Table 1.. Pertinent laboratory values with reference ranges.
Table 1.. Pertinent laboratory values with reference ranges. Table 2.. Vital signs during the first 5 days.
Table 2.. Vital signs during the first 5 days.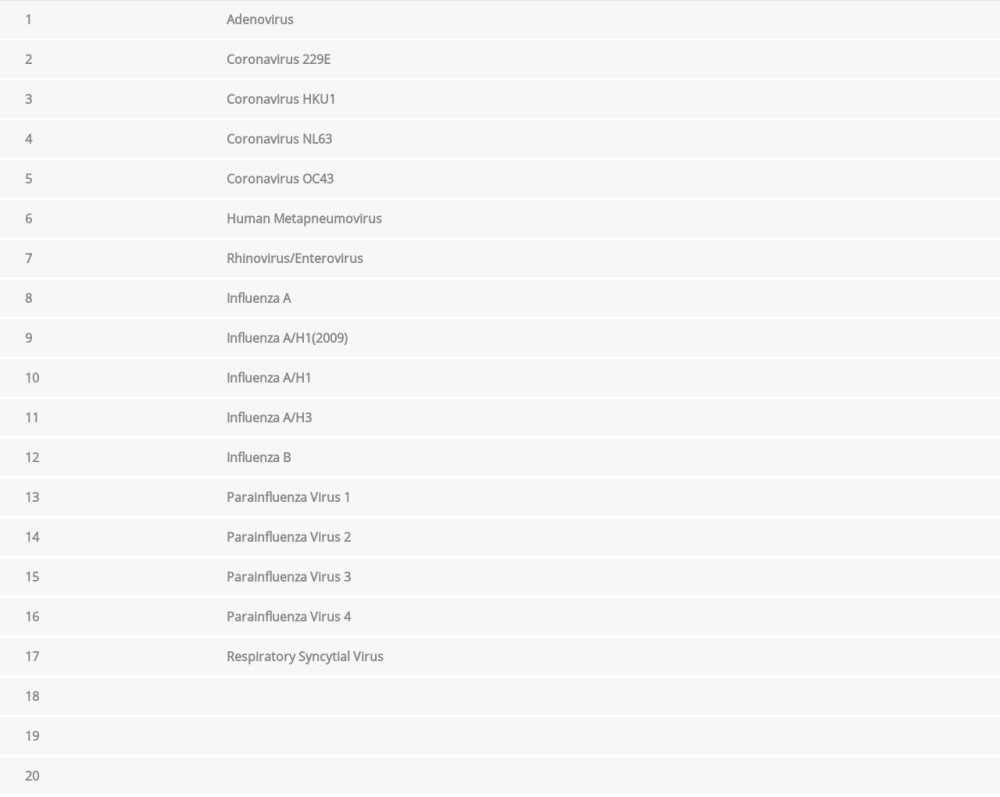 Table 3.. Respiratory infective organism ruled out with the respiratory multiplex real-time polymerase chain reaction.
Table 3.. Respiratory infective organism ruled out with the respiratory multiplex real-time polymerase chain reaction.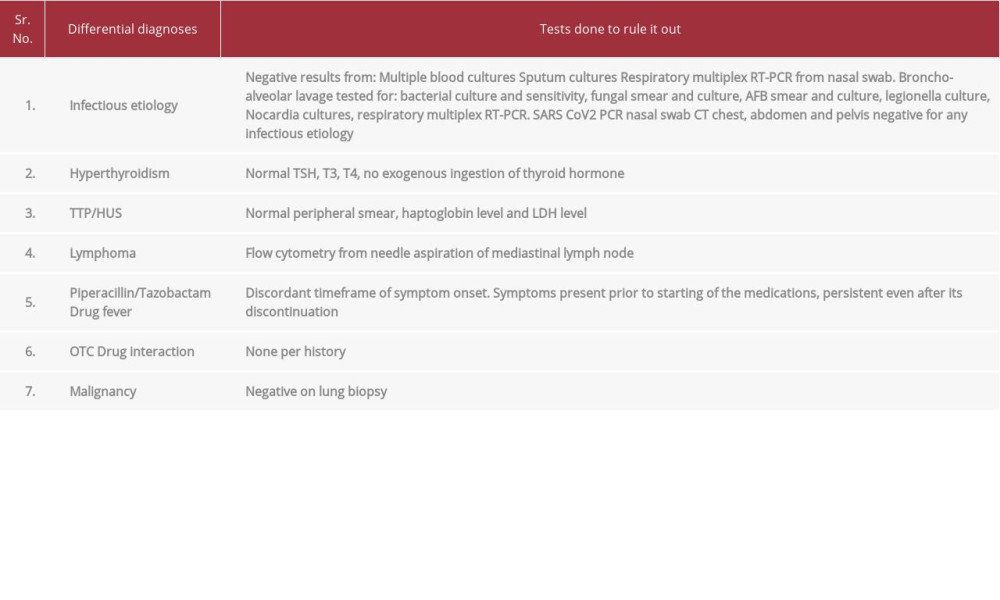 Table 4.. Differential diagnoses considered as the possible cause of patient’s clinical symptoms and tests done to rule them out.
Table 4.. Differential diagnoses considered as the possible cause of patient’s clinical symptoms and tests done to rule them out. In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








