20 January 2021: Articles 
Myasthenic Crisis as the First Presentation of Myasthenia Gravis: A Case Report
Unusual clinical course, Challenging differential diagnosis
Alvin Olivier Payus12DEF*, Justin Leow Wen Hsiang2BCD, Jia Qian Leong3DEF, Azliza Ibrahim4CDE, Azman Ali Raymond5EFDOI: 10.12659/AJCR.928419
Am J Case Rep 2021; 22:e928419
Abstract
BACKGROUND: Myasthenic crisis is a condition characterized by the sudden onset of myasthenic weakness involving the respiratory muscles and requires ventilatory support to prevent death. This is a case report of respiratory failure in a 43-year-old man as the first presentation of myasthenia gravis.
CASE REPORT: A 43-year-old man with underlying hypertension and a lacunar stroke with good muscle-power recovery presented with severe community-acquired pneumonia, complicated with respiratory failure requiring invasive ventilatory support. He responded well to the intravenous antibiotic therapy and after 1 week of treatment, he was hemodynamically stable and his septic parameters improved. However, he persistently failed to maintain adequate spontaneous respiratory effort after the removal of the ventilatory support and had to be reintubated multiple times. There was no other identifiable cause for the worsening respiratory failure. He had no clinical features or muscle weakness suggestive of myasthenia gravis. However, his blood test was positive for serum anti-acetylcholine receptor antibodies and repetitive nerve stimulation tests showed the characteristic decremental response of compound muscle action potential amplitude, in keeping with the diagnosis of myasthenia gravis. He responded well to intravenous immunoglobulin and was discharged with anticholinesterase inhibitors and long-term immunosuppression therapy.
CONCLUSIONS: This report demonstrates that when patients are admitted to the hospital with acute respiratory failure without any underlying pulmonary disease and with weakness of the respiratory muscles, the diagnosis of myasthenia gravis presenting with a myasthenic crisis should be considered.
Keywords: Myasthenia Gravis, Neuromuscular Junction, Receptors, Cholinergic, Respiratory Insufficiency, Immunoglobulins, Intravenous, Respiration, Artificial
Background
Myasthenia gravis is an immune-mediated condition involving the production of various types of antibodies directed against the motor receptors in the postsynaptic membrane at the neuromuscular junction [1]. Myasthenia gravis can be divided into 2 clinical forms: ocular myasthenia gravis limited to the eyelids and extraocular muscles, and generalized myasthenia gravis, which in addition to the involvement of ocular and eyelid muscles, can involve a variable combination of limb, bulbar, and respiratory muscles [1,2]. The incidence of myasthenia gravis ranges from 0.3 to 2.8 per 100 000 people, and it is estimated to affect more than 700 000 people worldwide [3]. It has a bimodal peak of incidence, with the first peak occurring in the 2nd to 3rd decades, which has a female predominance, and the second peak occurring in the 6th to 8th decades, which has a male predominance [1]. Myasthenia gravis is clinically diagnosed based on the typical history and physical findings. These are supported by the presence of serum autoantibodies directed against the postsynaptic components of the neuromuscular junction (most commonly the acetylcholine receptor) combined with the characteristic findings of a repetitive nerve stimulation test showing a decremental response and single-fiber electromyography showing a characteristic jitter response [4].
There are 3 principal treatments for myasthenia gravis: acetylcholinesterase inhibitors (including pyridostigmine or neostigmine) that aim to increase the availability of acetylcholine in the neuromuscular junction; long-term immunosuppressive agents (including corticosteroids, azathioprine, or mycophenolate mofetil) that target the underlying autoantibody; and rapid immunomodulatory therapy (including intravenous immunoglobulin or plasma exchange) that directly removes or deactivates the autoantibodies from circulation [3,4]. In patients with thymomas, a thymectomy is considered as a treatment option. However, a thymectomy has a significant role in selected patients without the evidence of a thymoma, including patients with generalized myasthenia gravis who are <60 years old and have positive autoantibodies [5].
A myasthenic crisis is a severe and life-threatening complication of myasthenia gravis characterized by respiratory failure that requires intubation and ventilatory support due to respiratory or oropharyngeal muscle weakness [6]. It is believed that up to 10% to 20% of myasthenia gravis patients will experience at least 1 crisis in their lifetime, and the estimated annual risk is about 2% to 3% [7]. The goal of treatment for a myasthenic crisis is to secure the airway, achieve prompt initiation of rapid immunomodulatory and immunosuppressive therapy, and to treat the identified precipitating factors, including infections, and the use of certain medications (aminoglycosides and beta blockers) [6–8]. Here, we report a case of respiratory failure in a 43-year-old man as the first presentation of myasthenia gravis and aim to increase the awareness among clinicians that the diagnosis of myasthenia gravis presenting with a myasthenic crisis should be considered.
Case Report
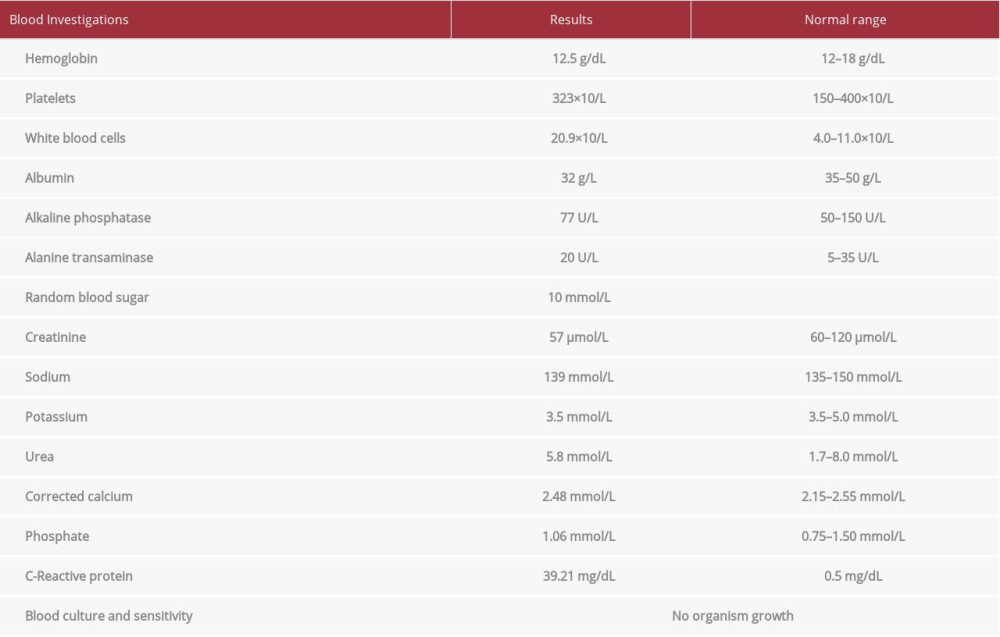
A 43-year-old man with a history of hypertension and a mild lacunar infarction with no remnant of weakness was taking oral perindopril 4 mg once daily and oral aspirin 150 mg once daily. He had no other remarkable medical or family history. He was referred from a district hospital for worsening respiratory failure secondary to community-acquired pneumonia requiring invasive ventilatory support. His chest X-ray showed consolidation over the right lower zone. The initial blood investigation results showed evidence of ongoing sepsis (Table 1) with marked leukocytosis and raised C-reactive protein levels. There was mild hypoalbuminemia, which could be due to the ongoing infection, and hyperglycemia due to stress. There were no abnormalities in the hepatic and renal functions, and the electrolytes were within the normal range. The blood cultures did not show any organism growth.
He was initially treated with intravenous (IV) co-amoxiclav 1.2 gm 3 times daily. However, he was transferred to the Intensive Care Unit as his vital signs deteriorated and he developed septic shock requiring triple inotropes support to maintain adequate mean arterial pressure. His condition improved after he completed 1 week of IV piperacillin/tazobactam 4.5 gm 4 times daily, and an extubation was performed. He failed to maintain adequate oxygenation via spontaneous respiratory effort after extubation, and had to be reintubated for ventilatory support. After several failed attempts to extubate, he underwent a tracheostomy for prolonged invasive ventilatory support. His repeat chest X-ray showed a marked improvement and no worsening of the consolidation. There was no identifiable cause for the persistent respiratory failure, and there were no clinical features of myasthenia gravis.
However, in view of the high index of suspicion by the treating physician, the patient was investigated for myasthenia gravis. The anti-acetylcholine receptor antibody level was 0.8 nmol/L (normal value <0.05 nmol/L). His nerve conduction study showed the characteristic decremental responses upon repetitive nerve stimulation, which were highly suggestive of neuromuscular junction disorder. There was characteristic decremental compound muscle action potential amplitude in response to repetitive nerve stimulation on the right abductor pollicis brevis (Figure 1A) and the right trapezius (Figure 1B). Both these findings were in keeping with the diagnosis of myasthenia gravis.
Immediately after the confirmation of the diagnosis, IV immunoglobulin 0.4 g/kg daily was started and administered for 5 days along with oral pyridostigmine 60 mg 3 times daily, oral prednisolone 15 mg once daily, and oral azathioprine 50 mg once daily. His condition gradually improved 2 weeks after taking the medication, and he managed to maintain good oxygen saturation on room air. Therefore, the tracheostomy was removed, and he was successfully discharged with oral azathioprine 50 mg once daily and oral pyridostigmine 60 mg 4 times to 5 times daily. He underwent a contrast-enhanced computed tomography scan of the thorax, which showed no evidence of a thymoma. He is currently followed up every 3 months at the Neurology Clinic. He responded well to the medication and there have been no further myasthenic crises since his discharge.
The patient gave informed consent for writing and publishing this case report, including the image and the results of his nerve conduction study. The Ethics Board of the Institute for Clinical Research of Malaysia gave approval for the publication of this case report via the National Medical Research Register.
Discussion
Myasthenia gravis is an antibody-mediated, T-cell-dependent autoimmune disorder, which is directed against the receptors or receptor-associated proteins located in the postsynaptic membrane of the neuromuscular junction [1]. Its hallmark clinical manifestation is muscle weakness that worsens with exertion and improves with resting [4]. In this report, we described a case of myasthenia gravis with an initial presentation of refractory respiratory failure requiring intubation and mechanical ventilation. The preceding history of severe community-acquired pneumonia obscured the suspicion of myasthenia gravis among the clinicians and caused an unnecessary diagnostic delay.
One of the complications of myasthenia gravis is the development of life-threatening respiratory failure that requires invasive ventilatory support to prevent death, in a condition called a myasthenic crisis. It is due to weakness of the respiratory or bulbar muscles, and has a mortality rate of 16% [6]. Although a myasthenic crisis can occur spontaneously, there are several common triggers, including concurrent infections, the use of certain medications including antibiotics (aminoglycosides, fluoroquinolones, macrolides), and high-dose corticosteroids used in the treatment of myasthenia gravis [6,7]. In the present case, we believe that the precipitating factor for the crisis episode was the severe bacterial pneumonia, which was further exacerbated by the stressful environment during the attempt to remove the invasive ventilatory support. There were no other identifiable causes or any administered medication that can explain the condition.
Myasthenia gravis, which presented for the first time as an isolated respiratory failure without any other neurological weakness [9] as reported in the present case, is very unusual. Therefore, this report illustrates the importance of considering myasthenia gravis as part of the differential diagnosis in cases of unexplained dyspnea or respiratory failure, especially in cases where the neurological causes can be overlooked when the patient presents with other causes of respiratory disease.
Conclusions
In conclusion, this case report demonstrates that when patients are admitted to the hospital with acute respiratory failure without underlying pulmonary disease but with weakness of the respiratory muscles, a diagnosis of myasthenia gravis presenting with a myasthenic crisis should be considered.
References:
1.. Gilhus NE, Myasthenia Gravis: N Engl J Med, 2016; 375(26); 2570-81
2.. Spillane J, Higham E, Kullmann DM, Easily missed? Myasthenia gravis: BMJ, 2013; 19; 36-38
3.. Narayanaswami P, Sanders DB, Wolfe G, International consensus guidance for management of myasthenia gravis: 2020 update: Neurology, 2020 [Online ahead of print]
4.. Bird SJ, Clinical manifestations of myasthenia gravis, 2015 UpToDate. 7th version.
5.. Evoli A, Meacci E, An update on thymectomy in myasthenia gravis: Expert Rev Neurother, 2019; 19(9); 823-33
6.. Neumann B, Angstwurm K, Mergenthaler P, Myasthenic crisis demanding mechanical ventilation: A multicenter analysis of 250 cases: Neurology, 2020; 94(3); e299-313
7.. Bird SJ, Overview of the treatment of myasthenia gravis: UpToDate; 2020
8.. Stetefeld H, Schroeter M, SOP myasthenic crisis: Neurological Research and Practice, 2019; 1(1); 19
9.. Sharma SR, Sharma N, Yeolekar ME, An undiagnosed myasthenia gravis presenting as isolated recurrent acute respiratory failure: J Neurosci Rural Pract, 2012; 3(1); 80-82
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250