22 March 2021: Articles 
Single-Setting Superior Vena Cava Biopsy and Stenting Utilizing Cone Beam Computed Tomography as an Additional Tool
Management of emergency care
Daniel Yuxuan Ong1ABCDEF, Lawrence Han Hwee Quek1ABCDEF, Ivan Kuang Hsin Huang1ABCDEF, Gavin Hock Tai Lim1ABCDEF, Gabriel Chan1ABCDEF, Yi-Wei Wu1ABCDEF, Seung Wook Ryu1ABCDEF, Uei Pua1ABCDEF*DOI: 10.12659/AJCR.929048
Am J Case Rep 2021; 22:e929048
Abstract
BACKGROUND: Malignant disease is a common etiology of superior vena cava syndrome (SVCS). Being a medical emergency, it often requires rapid diagnostic evaluation and therapy. Transcaval biopsy and endovascular stenting in a single-setting has been described, but only in a handful of cases. These cases utilized intra-operative venograms. In this study, we also used intra-operative cone beam computed tomography (CBCT) to increase the safety and efficacy of such single-setting procedures.
CASE REPORT: From January 2017 to July 2019, there were 5 patients with malignant SVCS who underwent single-setting superior vena cava biopsy and endovascular stenting utilizing intra-operative CBCT as an adjunct. Demographic data, clinical presentation, investigation results, procedural details, and patient outcomes were recorded. CBCT was utilized in all cases to optimize sampling of biopsies, visualize subsequent stent positioning, and for early detection of procedure-related complications. Transcaval biopsy was diagnostic in 4 of the 5 patients. Endovascular stents were deployed successfully in all cases, with post-stenting venogram demonstrating relief of prior obstructed segments. One patient had a complication of an apical pneumothorax, with no associated long-term pneumothorax-related morbidity or mortality.
CONCLUSIONS: This study demonstrates that single-setting transcaval biopsy and stenting in the context of malignant SVCS is a cost-efficient, safe, and feasible approach. In addition, the additional use of intra-operative CBCT is a useful tool to increase procedure efficacy and safety.
Keywords: Biopsy, Cone-Beam Computed Tomography, endovascular procedures, Superior Vena Cava Syndrome, Stents, Vena Cava, Superior
Background
Malignant disease is a common etiology of superior vena cava syndrome (SVCS) [1,2]. To determine the urgency and necessity for intervention, classification systems have been developed. In these classification systems, various parameters are considered, for instance, symptomatology [3–5]. Regardless, being a medical emergency, it often requires rapid diagnostic evaluation and therapy [1,2].
Conventionally, tissue diagnosis of mediastinal masses causing SVCS can be achieved via mediastinoscopy-, flexible bronchoscopy-, or computed tomography (CT)-guided percutaneous biopsy. The positive biopsy rates for image-guided percutaneous mediastinal biopsy are 77% for fine-needle aspiration cytology and up to 94% for core samples, with complication rates of 1.3% to 20%, with the most common complication being pneumothorax [6,7]. Subsequent treatment options include endovascular stenting, chemotherapy, and/or radiotherapy. SVC stenting has been reported to offer faster, more effective, and more sustained relief of symptoms [8].
Single-setting transcaval biopsy with endovascular stenting has been described, and allows rapid diagnosis and therapy to be achieved [9–11]. Existing techniques use pre-operative CT imaging and intra-operative venograms. In this study, we also used intra-operative cone beam computed tomography (CBCT), which increases the safety and efficacy of a single-setting SVC biopsy and stenting.
Case Reports
OPERATIVE TECHNIQUES:
The patient’s pre-operative CT images were reviewed (Figure 1A, 1B). The obstruction site’s spatial relation to surrounding vital structures (eg, aorta, bronchus) were established in o’clock fashion based on axial imaging. This was later assessed again using CBCT, with correlation to the clock face at the groin puncture site. All procedures were performed in a flat-panel-based angiographic suite with CBCT equipped (Allura Xper FD20; Philips Medical Systems, The Netherlands). Common femoral vein access was obtained using ultrasound guidance and secured with a vascular sheath. A guidewire was manipulated past the occluded segment and positioned within the internal jugular vein. An intra-operative venogram was used to demonstrate the SVC obstruction pre-stenting (Figure 1C, 1D). A trans-jugular liver biopsy set (Argon Medical, TX) was used for the biopsy. A two-stage firing mechanism involves deploying the needle at the site of interest first, with sampling performed subsequently after confirming optimal positioning via fluoroscopy and CBCT (Figure 1E, 1F). Intra-operative images were acquired using CBCT with a 220-degree rotation of the C-arm, and the XperGuide software (Allura, XperGuide; Philips Medical Systems, The Netherlands) was used for multiplanar reconstruction on the workstation. A total of 4 cm of core tissue was then obtained. After collection of the biopsy samples, the SVC was stented. Stents used in our institution include Zilver Vena (Cook Medical Inc., Bloomington, IN), Sinus XL (OptiMed, Ettlingen, Germany), Venovo (Bard, Tempe, AZ), and ABRE (Medtronic, Minneapolis, MN). Stent selection was based on patient factors and operator’s preference. Post-stenting venogram was obtained to demonstrate relief of the SVC obstruction (Figure 1G). CBCT was concurrently utilized to demonstrate positioning of the SVC stent, as well as to assess for early procedure-related complications such as hematoma formation (Figure 2A–2C).
Results
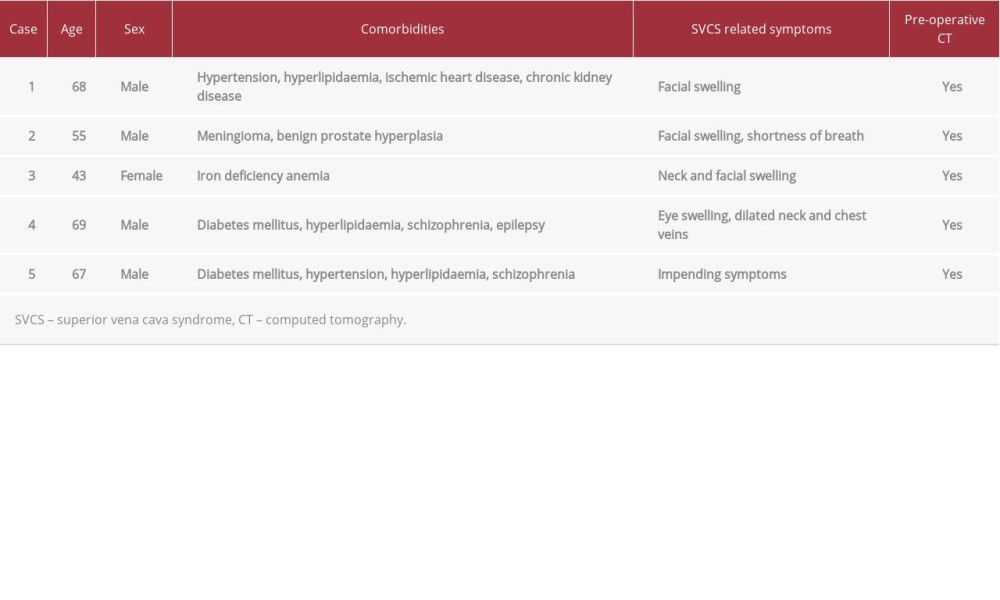
Demographic information of the 5 patients is displayed in Table 1. Five patients (4 men, 1 woman) with a mean age of 60 years and an age range of 43–69 years were identified. Four patients had symptomatic SVCS, while 1 was having impending symptoms.
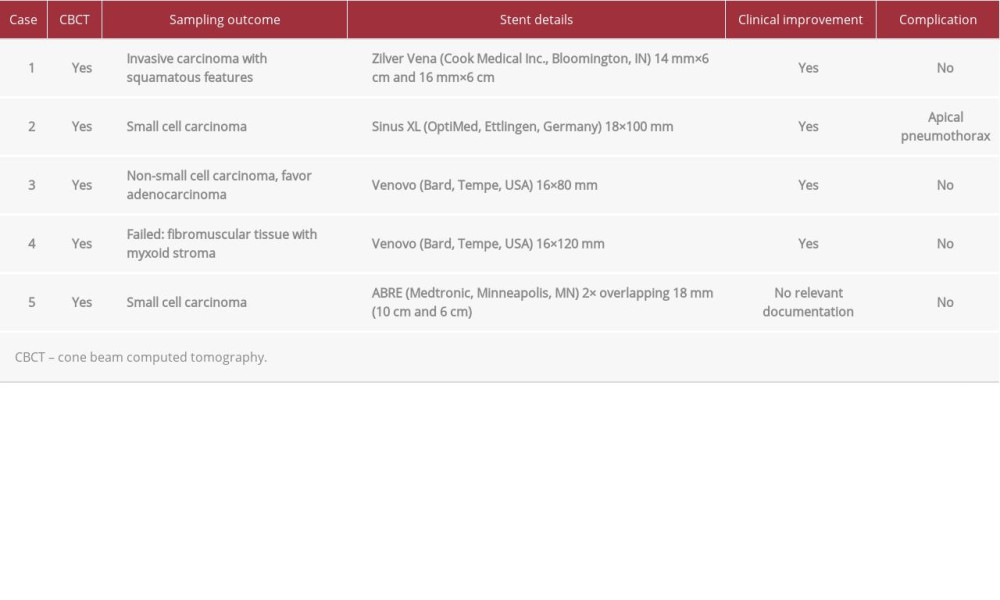
All the patients had pre-operative CT and intra-operative CBCT, which contributed to the planning and execution of the procedure. Four of 5 biopsies performed were successful and yielded oncologic diagnosis. The biopsy that did not yield oncologic diagnosis was later obtained via endobronchial ultrasound-guided biopsy, with the final histologic diagnosis of small cell carcinoma.
Procedural details are displayed in Table 2. Stents were deployed successfully in all cases, with post-stenting venogram demonstrating relief of prior obstructed segments. Four of 5 cases had documented symptom relief/improvement. One case lacked detailed post-procedure documentation. These patients do not have a history of prior SVC stenting.
One patient experienced a postoperative complication of development of a 3-cm apical pneumothorax. There was no long-term pneumothorax-related morbidity or mortality. The patient was eventually discharged with plans for outpatient follow-up.
Discussion
Superior vena cava syndrome is an emergency often warranting emergent management [1,2]. While transvenous biopsy of masses such as the kidney has been well described [12], there is a paucity of data on transvenous biopsy of mediastinal masses. Transcaval biopsy and endovascular stenting in a single-setting is even rarer, with only a handful of cases described [9–11]. Described techniques involves utilizing pre-operative CT and intra-operative venogram to assist with the procedure.
In this study, we also used intra-operative CBCT to increase the safety and efficacy of a single-setting SVC biopsy and stenting. The exact details of CBCT image acquisition are not within the scope of this report. Briefly, CBCT uses flat-panel detector technology to obtain CT-like axial images. The radiation source beam and flat panel detector are coupled together by a C-arm. In a single rotation of the C-arm, the CBCT unit is able to acquire a volumetric dataset, the exact volume of which varies depending on the machine used [13,14]. The advantage of CBCT is that it allows cross-sectional imaging of the area of interest to be obtained intra-operatively. This confers the additional benefit of optimizing sampling for biopsy, and also enabling the visualization of stent positioning. Early detection of postoperative complications such as hematoma formation is also now possible.
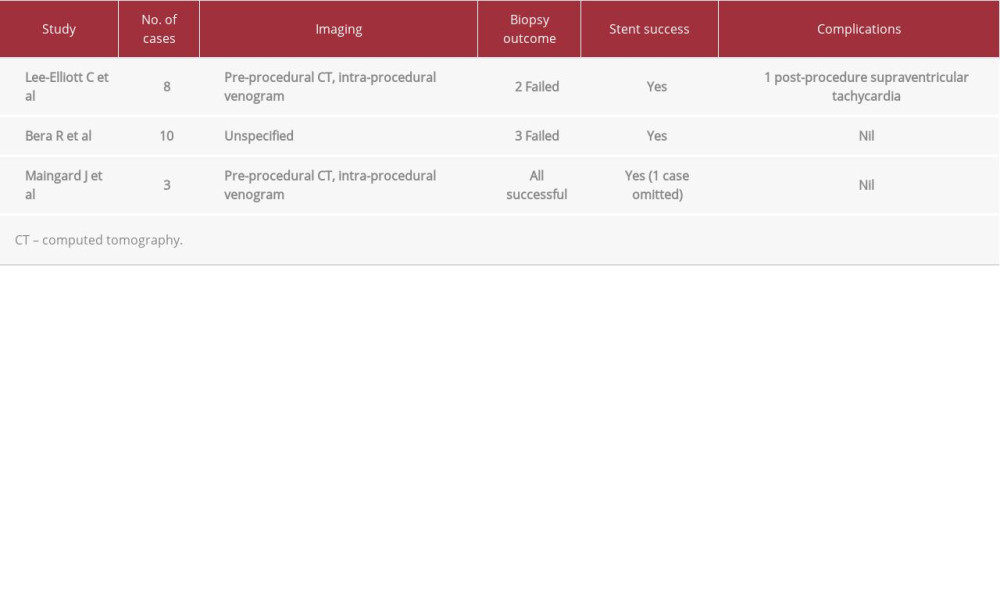
The results of the present study suggest that single-setting transcaval biopsy and endovascular stenting with CBCT as an adjunct is a safe and feasible option in the management of malignant SVCO. Theoretically, the additional visualization of the region of interest provided by the use of CBCT can increase the rates of biopsy success and also reduce the rates of operative complications. This technique may thus be comparable, or superior, to percutaneous options of mediastinal biopsy. In our case series, 1 patient had a complication of an apical pneumothorax, but did not have any long-term pneumothorax-related morbidity or mortality. Although our study had a small sample size, the low incidence of procedure-related complication makes this approach an attractive one. In this study, all patients had successful stent deployments, with relief of SVC obstruction demonstrated on post-stenting venogram. Together with the preceding evidence of single-setting transcaval biopsy and stenting, this study supports the safety and efficacy of such procedures (Table 3). As the patients recruited in this study were among the first undergoing such procedures, we are optimistic that with further experience, improvements in technical success can be expected.
There are many benefits of a single-setting SVC biopsy and stenting. The procedure is minimally invasive and avoids the need for further invasive diagnostic procedures. Patient comfort is also maximized [11]. From an economic standpoint, there are cost savings, as diagnosis and alleviation of symptoms can potentially be rapidly achieved in a single intervention. In our institution, the potential savings can amount up to approximately $2600 or more ($1200 from an extra admission, and $1400 for an additional CT-guided biopsy if a 2-stage procedure was performed instead). Maingard [11] also suggests that hospital stay could be reduced as a result. With the additional use of CBCT, as previously posited, surgeons can more accurately target the biopsy site, which can also reduce biopsy-related complications.
There are several limitations of this study. Firstly, this is a small sample-sized retrospective case series analysis. In addition, this study does not adequately address the issue of patient selection. Patient factors, such as young age, or disease factors such as lymphoma, would undoubtedly influence the feasibility of such an approach [9,11]. Furthermore, the additional use of CBCT comes with risks of radiation exposure.
Conclusions
To conclude, this study supplements existing evidence that single-setting transcaval biopsy and stenting in the context of malignant SVCS is a cost-efficient, safe, and feasible approach. In addition, the additional use of intra-operative CBCT is a useful tool to increase procedure efficacy and safety.
Figures
References:
1.. Straka C, Ying J, Kong F, Review of evolving etiologies, implications and treatment strategies for the superior vena cava syndrome: SpringerPlus, 2016; 5(1); 229
2.. Hamzik J, Chudej J, Dzian A, Endovascular stenting in malignant obstruction of superior vena cava: International J Surg Case Rep, 2015; 13; 84-87
3.. Lonardi F, Gioga G, Agus G, Double-flash, large-fraction radiation therapy as palliative treatment of malignant superior vena cava syndrome in the elderly: Supportive Care in Cancer, 2002; 10(2); 156-60
4.. Yu J, Wilson L, Detterbeck F, Superior vena cava syndrome – a proposed classification system and algorithm for management: J Thoracic Oncol, 2008; 3(8); 811-14
5.. Kishi K, Sonomura T, Mitsuzane K, Self-expandable metallic stent therapy for superior vena cava syndrome: Clinical observations: Radiology, 1993; 189(2); 531-35
6.. Morrissey B, Adams H, Gibbs A, Crane M, Percutaneous needle biopsy of the mediastinum: review of 94 procedures: Thorax, 1993; 48(6); 632-37
7.. Grant T, Stull M, Kandallu K, Percutaneous needle biopsy of mediastinal masses using a computed tomography-guided extrapleural approach: Journal of Thoracic Imaging, 1998; 13(1); 20
8.. Nicholson A, Ettles D, Arnold A, Greenstone M, Dyet J, Treatment of Malignant Superior Vena Cava Obstruction: Metal Stents or Radiation Therapy: J Vasc Interv Radiol, 1997; 8(5); 781-88
9.. Lee-Elliott C, Abubacker M, Lopez A, Fast-track management of malignant superior vena cava syndrome: Cardiovasc Intervent Radiol, 2004; 27(5); 470-73
10.. Bera R, Zia Z, Bashir O, Abstract No. 435: Simultaneous transvenous biopsy and stenting in malignant superior vena cava obstruction: J Vasc Interv Radiol, 2012; 23(3); S172-73
11.. Maingard J, Brooks M, Transcaval core biopsy in malignant superior vena cava obstruction: Potential for single stage diagnosis and treatment: J Med Imaging Radiat Oncol, 2017; 61(2); 232-38
12.. Wendth A, Garlick W, Pantoja E, Shamoun J, Transcatheter biopsy of renal carcinoma invading the inferior vena cava: J Urol, 1976; 115(3); 331-32
13.. Wong K, Tan B, Taneja M, Cone beam computed tomography for vascular interventional radiology procedures: Early experience: Ann Acad Med Singap, 2011; 40(7); 308-14
14.. Orth R, Wallace M, Kuo M, C-arm Cone-beam CT: General principles and technical considerations for use in interventional radiology: J Vasc Interv Radiol, 2009; 20(7); S538-44
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250