05 April 2021: Articles 
Portal and Mesenteric Vein Thrombosis Associated with Hyperthyroidism
Unknown etiology
Aya Kato1AE, Yuichiro Matsuo1EF, Aki Miyagaki2E, Keita Endo3E, Eiji Hiraoka1ABDEF*DOI: 10.12659/AJCR.929565
Am J Case Rep 2021; 22:e929565
Abstract
BACKGROUND: Non-malignant and non-cirrhotic portal and mesenteric vein thrombosis is rare. It has been reported that the hyperthyroid state is associated with increased risks of venous thrombosis due to increases in levels of various coagulation and anti-fibrinolytic factors. Particularly, changes in levels of these factors are also reported in cases of portal and mesenteric vein thrombosis. Although hyperthyroidism is not known as a risk factor for portal and mesenteric vein thrombosis, it might be an underlying pathogenesis of hyperthyroidism-associated portal and mesenteric vein thrombosis.
CASE REPORT: A 59-year-old Japanese man with a history of Grave’s disease presented with acute portal and mesenteric vein thrombosis and hyperthyroidism. Anticoagulation therapy was initiated and the dose of antithyroid drug was increased. He underwent various tests to identify causes of portal and mesenteric vein thrombosis. However, all test results were within normal range except for hyperthyroidism. Therefore, we discontinued anticoagulation therapy after normalization of thyroid hormone status. After 3 years, he experienced recurrence of portal vein thrombosis concomitant with hyperthyroidism.
CONCLUSIONS: Hyperthyroidism might be associated with portal vein thrombosis. Thyroid function tests should be performed in cases of portal and mesenteric vein thrombosis in the absence of other risk factors.
Keywords: hyperthyroidism, Mesenteric Vascular Occlusion, Venous Thrombosis, Mesenteric Veins, Portal Vein, Thrombolytic Therapy
Background
Portal and mesenteric vein thrombosis is a manifestation of unusual-site venous thromboembolism. Its incidence is lower than that of the usual-site venous thromboembolism (lower-extremity deep-vein thrombosis and pulmonary embolism) [1].
The risk factors of portal and mesenteric vein thrombosis include local and systemic factors. The pathogenesis of local risk factors includes endothelial damage and stasis. Endothelial damage may be caused by abdominal cancer (eg, pancreatic, hepatobiliary, or gastrointestinal); abdominal inflammatory diseases (eg, inflammatory bowel disease or pancreatitis); infections (eg, cholecystitis, appendicitis, or hepatic abscess); or abdominal surgery [2]. Stasis may result from liver cirrhosis, portal hypertension, and abdominal compartment syndrome [2]. Hypercoagulability as a systemic risk factor can be caused by inherited or acquired disorders. Examples of inherited conditions are anti-thrombin deficiency, protein C deficiency, protein S deficiency, factor V Leiden mutation, and prothrombin G20210A mutation [3]. Acquired disorders include myeloproliferative neoplasms, antiphospholipid antibody syndrome, Behcet’s disease, paroxysmal nocturnal hemoglobin-uria, hyperhomocysteinemia, hormonal therapy, and pregnancy [3]. However, currently available investigations could not identify causal factors in approximately 20% of patients [2].
To date, there have been no reports of the association of hyperthyroidism with portal and mesenteric vein thrombosis. However, it has been reported that the hyperthyroid state was associated with increased risks of pulmonary embolism, deep-vein thrombosis, and cerebral venous thrombosis due to increases in levels of various coagulation and anti-fibrinolytic factors [4]. Herein, we describe a patient who presented with portal and mesenteric vein thrombosis that might possibly be associated with hyperthyroidism.
Case Report
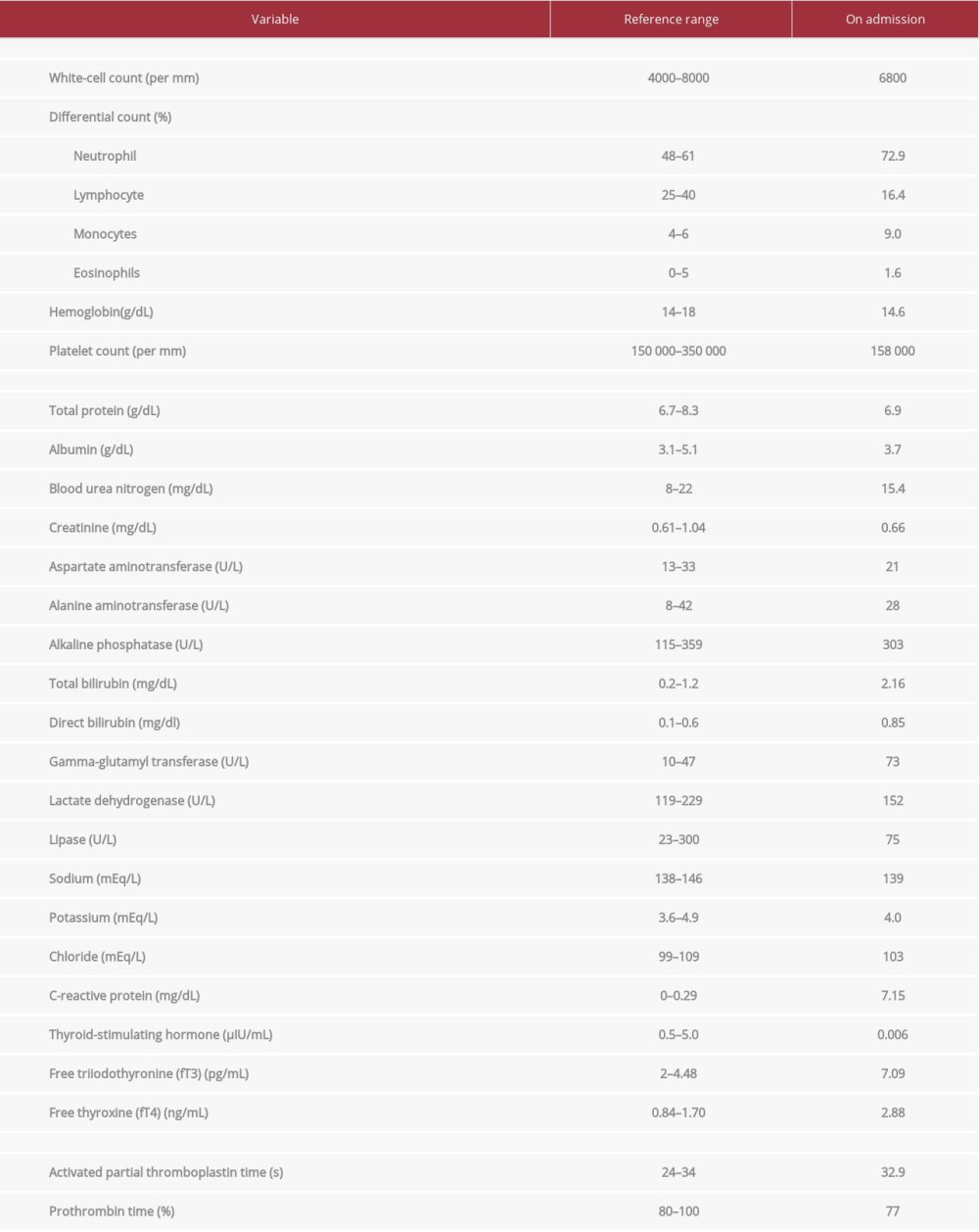
A 59-year-old Japanese man presented to our hospital with continuous epigastric pain for 5 days. He had no fever, weight loss, nausea, diarrhea, or vomiting. For the past 20 years, he had been taking 5 mg thiamazole every other day for hyper-thyroidism due to Grave’s disease. His family medical history was unremarkable. He had a smoking history of consuming approximately 2–3 cigarettes per day for 25 years. However, he had quit smoking 10 years prior. He had a history of alcohol consumption of 14 grams per day for 35 years. On admission, his blood pressure and heart rate were 128/80 mmHg and 101 beats per min, respectively. His body mass index was 22.8 kg/m2. Physical examination revealed epigastric tenderness. Laboratory test results revealed raised levels of free triiodothyronine (FT3) and free thyroxine (FT4), and low levels of thyroid-stimulating hormone (TSH), being consistent with hyperthyroid state (Table 1). Results of renal function, liver enzyme, and coagulation tests were all within normal range (Table 1). He did not have signs suggestive of dehydration. He had moist oral membrane and normal serum levels of blood urea nitrogen and creatinine. An abdominal computed tomography (CT) scan showed pylethrombophlebitis complicated with thrombosis of the portal vein and superior mesenteric vein. There were no signs of other intraabdominal inflammation or neoplasms. No findings of chronic pancreatitis were present, such as calcification or atrophy of the pancreas, or dilation of the main pancreatic duct (Figure 1).
He was diagnosed with acute symptomatic portal and mesenteric vein thrombosis and hyperthyroidism. Anticoagulation with heparin was initiated, and thiamazole was increased from 5 mg every other day to 5 mg daily. His epigastralgia was resolved on day 3 of hospitalization. Anticoagulation was switched from heparin to warfarin. The patient was discharged from hospital on day 16. To investigate causes of portal and mesenteric vein thrombosis, upper gastrointestinal endoscopy; colonoscopy; magnetic resonance cholangiopancreatography; blood tests of protein C, protein S, and anti-thrombin III; and antiphospholipid antibody tests (lupus anticoagulant factor, anti-cardiolipin immunoglobulin G, and anti-cardiolipin β2-glycoproteinI complex antibody) were performed. None of them showed remarkable results. In summary, regarding causes of the portal vein thrombosis, malignancy, liver cirrhosis, abdominal infectious or inflammatory diseases, and hypercoagulable disorders were excluded.
During outpatient follow-up, although he developed remarkable hepatopetal collateral circulation due to portal hypertension, the thrombus became indistinct (Figure 2). It was not clear whether the thrombus completely resolved. However, we discontinued treatment with anticoagulation 12 months after its initiation when his thyroid function had been normalized on thiamazole 5 mg daily. He was referred back to his primary care physician.
Three years later, he presented to our hospital with 2 weeks of epigastric pain. Abdominal CT scan showed mesenteric vein thrombosis and residual hepatopetal collateral circulation (Figure 3). He was diagnosed with recurrent portal and mesenteric vein thrombosis. On admission, he was administered heparin, which was later switched to warfarin (3 mg daily) on day 7 of readmission. Of note, thyroid function test results had worsened 3 months prior to his second admission (TSH <0.006 μIU/mL; free T3, 11.0 pg/dL; and free T4, 3.40 ng/dL). Then, the dose of thiamazole was increased from 5 mg daily to 30 mg daily 4 days before his second admission. On admission, his thyroid function test results were TSH <0.008 μIU/mL; FT4, 2.19 ng/dL; TSH-receptor antibody, 12.2 IU/L (normal range: less than 2.0 IU/L) on thiamazole 30 mg daily.
Ten days after admission, his endoscopic ultrasound revealed portal vein stenosis and residual thrombus near the confluence of the superior mesenteric vein and splenic vein. The thrombus in the superior mesenteric vein had resolved. Blood flow velocity was high on the proximal side of the stenosis, which suggested an influence of hepatopetal collateral circulation. We decided to continue anticoagulation indefinitely. He became asymptomatic on hospital day 4, and was discharged to home on hospital day 15.
Discussion
We encountered a case of portal and mesenteric vein thrombosis, which recurred concomitantly with worsening of hyper-thyroidism. To the best of our knowledge, this is the first case that shows a possibility of an association between hyperthyroidism and portal and mesenteric vein thrombosis.
Hyperthyroidism shifts hemostatic balance toward hypercoagulable and hypofibrinolytic states [4]. An association between hyperthyroidism and portal and mesenteric vein thrombosis has not been previously published. However, the hyperthyroid state has been reported to be associated with an increased risk of pulmonary embolism, deep-vein thrombosis of the lower limbs, and cerebral venous thrombosis [4]. The underlying etiology of hyperthyroid state as a risk factor of venous thrombosis is not only autoimmune thyroid diseases such as Graves’ disease and Hashimoto’s thyrotoxicosis, but also non-auto-immune thyroid diseases, such as subacute thyroiditis [4,5].
Hypercoagulability due to hyperthyroidism may be caused by an increase in levels of various coagulation factors such as factor VIII, IX, X, von Willebrand factor (vWF), and fibrinogen, and an anti-fibrinolytic factor such as plasminogen-activator inhibitor-1 (PAI-1) [6]. High levels of factors VIII and vWF are especially associated with the usual sites venous thrombosis (deep-vein thrombosis and pulmonary embolism) [7]. Several reports suggest that the risk of venous thromboembolism is increased with increased levels of FT4 [4,5,8]. The risk of venous thrombosis of these usual sites positively correlates with FT4 levels [9], which is also associated with high levels of factor VIII and vWF [4]. Increased levels of factors VIII, vWF, and PAI-1 were also reported among patients with portal and mesenteric vein thrombosis [10–12]. Therefore, increases in factor VIII and vWF caused by hyperthyroidism may possibly contribute to thrombus formation in portal and mesenteric veins.
The patient was a former smoker. Smoking causes endothelial dysfunction [13]. Both current smoking and past history of smoking lead to mildly elevated incidence of venous thromboembolism [14]. The smoking history could have had an effect on his repeated thromboembolism.
He did not have risk factors for thrombosis, except for hyperthyroidism and smoking history. Furthermore, portal and mesenteric vein thrombosis developed twice, concomitantly with worsening of hyperthyroidism. Based on the patient’s medical history and the previously mentioned literature, portal and mesenteric vein thrombosis might possibly have been caused by a hypercoagulable state induced by hyperthyroidism. However, we did not check on his factor VIII and vWF levels. To confirm an association between hyperthyroidism and portal and mesenteric vein thrombosis, it could have been helpful if we checked on these factors.
Portal hypertension due to the first portal vein thrombosis may have contributed to recurrence of portal and mesenteric vein thrombosis. Endoscopic ultrasound of this case revealed portal stenosis, and the blood flow velocity was different at the proximal and distal sides of the stenosis. It represents venous blood flow stasis at the distal side of the stenosis, which might also contribute to thrombus formation. Moreover, once portal hypertension develops, it might cause endothelial cell dysfunction in the extrahepatic and systemic circulations [15]. Endothelial damage is also a local risk factor of portal and mesenteric vein thrombosis. Recurrence of portal and mesenteric vein thrombosis might be due to not only hypercoagulable state by worsening of hyperthyroidism, but also local risk factors of stasis and endothelial damage caused by portal hypertension due to the first portal vein thrombosis. Additionally, since we could not confirm complete resolution of the first thrombus, a possibility remains that progression of residual portal vein thrombosis resulted in this second episode. However, in our case, portal hypertension had existed for 3 years since the first episode of portal and mesenteric vein thrombosis without recurrence of symptomatic portal and mesenteric vein thrombosis.
Given that the portal and mesenteric vein thrombosis recurred just after worsening of hyperthyroidism, it might be possible that hyperthyroidism contributed to portal and mesenteric vein thrombus formation. This is a single case report. Therefore, an accumulation of further cases is required.
Conclusions
We reported a case of portal and mesenteric vein thrombosis associated with hyperthyroidism. Thus, it may be reasonable to check on thyroid function as an underlying cause of idiopathic portal and mesenteric vein thrombosis.
Figures
References:
1.. Valeriani E, Riva N, Nisio MD, Splanchnic vein thrombosis: Current perspectives: Vasc Health Risk Manag, 2019; 15; 449-61
2.. Björck M, Koelemay M, Acosta S, Editor’s Choice – Management of the diseases of mesenteric arteries and veins: Clinical practice guidelines of the European Society of Vascular Surgery (ESVS): Eur J Vasc Endovasc Surg, 2017; 53; 460-510
3.. De Stefano V, Martinelli I, Splanchnic vein thrombosis: Clinical presentation, risk factors and treatment: Intern Emerg Med, 2010; 5; 487-94
4.. Elbers LPB, Fliers E, Cannegieter SC, The influence of thyroid function on the coagulation system and its clinical consequences: J Thromb Haemost, 2018; 16; 634-45
5.. Franchini M, Lippi G, Targher G, Hyperthyroidism and venous thrombosis: A casual or causal association? A systematic literature review: Clin Appl Thromb Hemost, 2011; 17; 387-92
6.. Ordookhani A, Burman KD, Hemostasis in overt and subclinical hyperthyroidism: Int J of Endocrinol Metab, 2017; 15; e44157
7.. Rietveld IM, Lijfering WM, le Cessie S, High levels of coagulation factors and venous thrombosis risk: Strongest association for factor VIII and von Willebrand factor: J Thromb Haemost, 2019; 17; 99-109
8.. Hooper JMW, Stuijver DJF, Orme SM, Thyroid dysfunction and fibrin network structure: A mechanism for increased thrombotic risk in hyper-thyroid individuals: J Clin Endocrinol Metab, 2012; 97; 1463-73
9.. van Zaane B, Squizzato A, Huijgen R, Increasing levels of free thyroxine as a risk factor for a first venous thrombosis: A case-control study: Blood, 2010; 155; 4344-49
10.. Alkim H, Ayaz S, Sasmaz N, Hemostatic abnormalities in cirrhosis and tumor-related portal vein thrombosis: Clin Applied Thromb Hemoss, 2012; 18; 409-15
11.. Raffa S, Reverter JC, Seijyo S, Hypercoagulability in patients with chronic noncirrhotic portal vein thrombosis: Clin Gastroenterol Hepatol, 2012; 10; 72-78
12.. Parikh M, Adelsheimer A, Somoza E, Factor VIII elevation may contribute to portomesenteric vein thrombosis after laparoscopic sleeve gastrectomy: A multicenter review of 40 patients: Surg Obes Relat Dis, 2017; 13; 1835-39
13.. Rajendran P, Rengarajan T, Thangavel J, The vascular endothelium and human diseases: Int J Biol Sci, 2013; 9; 1057-69
14.. Pomp ER, Rosendaal FR, Doggen CJ, Smoking increases the risk of venous thrombosis and acts synergistically with oral contraceptive use: Am J Hematol, 2008; 83; 97-102
15.. Iwakiri Y, Endothelial dysfunction in the regulation of portal hypertension: Liver Int, 2012; 32; 199-213
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250