10 April 2021: Articles 
Hypokalemia-Induced Rhabdomyolysis Caused by Adrenal Tumor-Related Primary Aldosteronism: A Report of 2 Cases
Unusual clinical course, Challenging differential diagnosis
Chung-Tso Chen1ABCDEF*, Yen-Chieh Wang12ABD, Chih-Ming Lin1ABCDFDOI: 10.12659/AJCR.929758
Am J Case Rep 2021; 22:e929758
Abstract
BACKGROUND: Primary aldosteronism, also known as Conn’s syndrome, is a clinical condition caused by excessive production of aldosterone. The classic presenting signs of primary aldosteronism are hypertension and hypokalemia. However, rhabdomyolysis induced by severe hypokalemia is a rare manifestation of primary aldosteronism. There were only a few cases presented in the English literature over the last 4 decades.
CASE REPORT: We present 2 cases, a 53-year-old man and a 46-year-old man, with severe hypokalemia-induced rhabdomyolysis caused by adrenal tumor-related primary aldosteronism. Both of these patients were under medical treatment with oral anti-hypertension drug for hypertension, but were poorly controlled. They both presented to the Emergency Department with muscle weakness and pain. Laboratory testing showed elevated creatinine phosphokinase (CPK) and low serum potassium levels. Hypokalemia-induced rhabdomyolysis was suspected. A further endocrine survey showed low PRA (plasma renin activity) and high aldosterone levels, finding which are compatible with primary aldosteronism. Computed tomography (CT) was arranged for further evaluation, and adrenal tumors were found in both cases. Both patients underwent robotic-assisted laparoscopic adrenalectomy. In both cases, there was no recurrence of hypokalemia without potassium supplementation, and their hypertension was under better control at further follow-up visits.
CONCLUSIONS: Hypokalemic rhabdomyolysis is a rare manifestation of primary aldosteronism. It might be difficult to making a diagnosis when rhabdomyolysis and severe hypokalemia are the first manifestations in patients with primary aldosteronism. The use of diuretics for hypertension treatment might be a risk factor for extremely low potassium levels, which can induce rhabdomyolysis in patients with primary aldosteronism.
Keywords: Adrenal Gland Neoplasms, Adrenalectomy, Adrenocortical Hyperfunction, Hyperaldosteronism, Hypokalemia, Aldosterone, Hypertension, rhabdomyolysis
Background
Primary aldosteronism, also known as Conn’s syndrome, is a clinical condition caused by excessive production of aldosterone, resulting in sodium retention and potassium excretion. The classic presenting signs of primary aldosteronism (PA) are hypertension and hypokalemia. Hypokalemia induced by PA is a chronic process with tolerable symptoms of fatigue, malaise, muscle weakness, and muscle cramping [1]. In some cases, however, the extremely low levels of potassium caused by PA can induce rhabdomyolysis. Rhabdomyolysis induced by severe hypokalemia is a rare manifestation of PA. There were only a few cases presented in the English literature over the last 4 decades [2–9]. Here, we present 2 cases of severe hypokalemia-induced rhabdomyolysis caused by adrenal tumor-related primary aldosteronism.
Case Report
CASE 1:
A 53-year-old man with resistant hypertension, which was poorly controlled despite being treated with a combination of Amlodipine, Valsartan, and Hydrochlorothiazide, was referred to our hospital due to progressive weakness of the limbs for 2 weeks. The patient also complained of muscle soreness, general malaise, nausea, and tea-colored urine. He denied having heavy exercise recently. He also had a past history of diabetes with vildagliptin and metformin treatment, as well as gouty arthritis without medication control. He was a heavy smoker with smoking history over 30 years. He denied any specific family history and allergy history.
At the Emergency Department, his vital signs were stable except for elevated blood pressure (164/110 mmHg). Physical examination revealed that all 4 limbs had tenderness but were freely movable. His consciousness status was clear and no neurologic deficit was noted. Laboratory testing showed elevated creatinine phosphokinase (CPK) (15 930 IU/L), low serum potassium (2.1 mmol/L), and metabolic alkalosis (pH 7.505). Urine testing showed occult blood positive, with normal count of red blood cell (Table 1). Based on these clinical features and data, hypokalemia-induced rhabdomyolysis was diagnosed. Intravenous hydration and potassium supplementation were administered. After admission, an endocrine survey was performed due to persistent hypokalemia even after supplementation of potassium and showed low PRA (plasma renin activity), high aldosterone levels, and high ARR (aldosterone-to-renin ratio), findings which are compatible with primary aldosteronism (Table 1). Other endocrine indicators such as cortisol and adrenocorticotropic hormone (ACTH) were normal. Therefore, a computed tomography (CT) of the adrenal glands was arranged and revealed a 1.3-cm oval lesion on the left adrenal gland (Figure 1).
CASE 2:
A 46-year-old man with hypertension was being treated with Valsartan and Hydrochlorothiazide. He was referred to our hospital due to sudden onset of lower-limbs pain and weakness. He denied other past medical history, family history, and allergy history. Cigarette smoking and alcohol consumption were also denied.
At the Emergency Department, extremely elevated blood pressure (217/136 mmHg) was noted. Physical examination revealed bilateral thigh tenderness, but all 4 limbs were freely movable. His consciousness status was clear and no neurologic deficit was noted. The lab data showed severe hypokalemia with elevated CPK and myoglobin. A urine test showed occult blood positive with elevated count of red blood cell (Table 1). Rhabdomyolysis secondary to hypokalemia was diagnosed. An abdominal CT was arranged, which showed a 1.5-cm oval mass on the left adrenal gland (Figure 2). After admission, due to persistently low potassium level in spite of supplementation of potassium, an endocrine survey was performed and showed low PRA and high ARR, findings which are compatible with primary aldosteronism (Table 1). Other endocrine indicators such as cortisol and ACTH were normal.
Both patients were first treated for their rhabdomyolysis and severe hypokalemia. Adequate intravenous hydration and potassium supplementation were necessary. The symptoms such as muscular pain and weakness and the lab data showing rhabdomyolysis were improved after initial treatment. Their potassium levels improved gradually, but both patients had a poor initial response to treatment. Both of them were then treated with robotic-assisted laparoscopic adrenalectomy after their serum CPK and K+ levels improved (preoperative CPK and K+ level, 345 IU/L and 3.5 mmol/L in Case 1; 1049 IU/L and 4 mmol/L in Case 2). Pathological examinations revealed adrenocortical adenomas. In both cases, there was no recurrence of hypokalemia without potassium supplementation, and lab results were normal at the follow-up visits (Table 2). Their hypertension was also under better control at further follow-up visits.
Discussion
Rhabdomyolysis is a pathological condition of skeletal muscle cell damage that leads to the release of toxic intracellular material, such as CPK, myoglobin, and potassium, into the blood circulation [10]. There are multiple potential causes of rhabdomyolysis, including trauma, ischemia, metabolic disorders, infection, and drug and electrolyte disorders. Hypokalemia and hypophosphatemia are the major causes of electrolyte abnormality-induced rhabdomyolysis [11,12].
Potassium plays an important role in the regulation of skeletal muscle blood flow in the pathogenesis of rhabdomyolysis. Potassium released from muscle cells during exercise mediates vasodilation, which increases the blood flow to muscles appropriately to meet enhanced energy demands. However, profound hypokalemia (serum potassium <2.5 mEq/L) may lead to lower increases in blood flow and decreased muscle perfusion, which can promote the development of rhabdomyolysis by decreasing the blood flow to the muscles in response to exertion [13].
In PA, excessive production of aldosterone results in sodium retention with plasma volume expansion and potassium excretion. It usually presents with hypertension and mild hypokalemia, while malaise, fatigue, and muscular weakness are generally tolerable symptoms [2]. However, extremely low levels of potassium may occur due to vomiting and diarrhea or when diuretics are used [3,4]. Both of the patients discussed in this report had a history of hypertension and were taking anti-hypertension drugs, including Hydrochlorothiazide. These factors might increase the risk of hypokalemia-induced rhabdomyolysis in both cases. A study by Zavatto et al [7] noted that there were 22 previous cases of severe hypokalemic rhabdomyolysis induced by PA reported in the English literature over the 39 years from 1976 to 2015. This indicates that hypokalemic rhabdomyolysis is a rare manifestation of primary aldosteronism. In addition, 8 of those 22 cases involved patients who used diuretics (hydrochlorothiazide or furosemide) as anti-hypertension drugs. A recent report by Wu et al [8] also presented a 44-year-old woman with poorly controlled hypertension that was being treated with captopril and indapamide. She was sent to an Emergency Department due to weakness in the lower extremities and difficulty walking for 2 days. Laboratory finding revealed elevated CPK and extremely low potassium. They first treated this patient as having polymyositis. Endocrine survey and CT examination were performed due to persistent hypokalemia even after high-dose supplementation of potassium. An endocrine survey showed suppressed PRA and extremely high ARR. A CT scan revealed a 1.8-cm adenoma in the right adrenal area. She finally underwent surgical removal of the adenoma and reported no recurrence of the symptoms at the 8-month follow-up. Her symptoms, laboratory finding, imaging finding, and clinical course were similar to our cases. These finding might indicate that the use of thiazide and loop diuretics are important risk factors for severe hypokalemia-induced rhabdomyolysis in PA patients and result in their mechanism of potassium expulsion. It also indicates that the easily misdiagnosis when rhabdomyolysis and severe hypokalemia are the first manifestations in PA patients [8,9]. In our cases, we first only treated their rhabdomyolysis and hypokalemia. The response to the treatment was initially poor because we did not recognize the true cause of their problems.
The treatment strategies for PA entail removing the source of excess mineralocorticoids or blocking the effect of aldosterone in the target organs. Therefore, control and prevention of the morbidity associated with excess mineralocorticoids are the treatment goals [14,15]. Adrenal vein sampling (AVS) is the criterion standard for localizing the laterality of aldosterone-secreting adenomas and for differentiating between unilateral or bilateral sources of aldosterone secretion in patients with PA [16,17]. In patients with confirmed lateralizing aldosterone secretion, adrenalectomy should be considered. The majority of patients with small unilateral aldosterone-producing adenomas are candidates for laparoscopic adrenalectomy [18]. However, for those patients who are not surgical candidates, such as those with bilateral aldosterone secretion or poor general condition, medical treatment is indicated. The aldosterone receptor antagonists, such as spironolactone, are successful in lowering blood pressure and maintaining potassium levels. They are, therefore, the first choices of antihypertensive agents in patients with PA [14,15]. In our cases, it was necessary to manage the rhabdomyolysis and severe hypokalemia first. Adequate intravenous hydration and potassium supplementation were thus necessary. We did not perform AVS in these 2 cases because CT examinations reveal a unilateral adrenal tumor over 1 cm in size in both cases. We eventually decided not to perform such an invasive diagnostic procedure on either of them. Both of our patients were then treated with robotic-assisted laparoscopic adrenalectomy after their serum CPK and K+ levels normalized. In both cases, there was no recurrence of hypokalemia without potassium supplementation after surgery or during further follow-up.
Conclusions
Hypokalemic rhabdomyolysis is a rare manifestation of PA. Making a diagnosis of PA can be difficult when rhabdomyolysis and severe hypokalemia are the first manifestations. The use of diuretics for hypertension treatment might be a risk factor for extremely low potassium levels, which can induce rhabdomyolysis in patients with PA. Patients taking diuretics, especially thiazide, can potentially be predisposed to hypokalemia-induced rhabdomyolysis, as were the patients in the present report. Patients with hypokalemia of unknown etiology or with truly resistant hypertension should be evaluated for PA.
References:
1.. Wu VC, Hu YH, Er LK, Case detection and diagnosis of primary aldosteronism – the consensus of Taiwan Society of Aldosteronism: J Formos Med Assoc, 2017; 116; 993-1005
2.. Zhang W, Li CW, Zeng CY, Rhabdomyolysis presenting with severe hypokalemia in hypertensive patients: A case series: BMC Res Notes, 2013; 6; 155
3.. Goto A, Takahashi Y, Kishimoto M, Primary aldosteronism associated with severe rhabdomyolysis due to profound hypokalemia: Intern Med, 2009; 48; 219-23
4.. Cooray MSA, Bulugahapitiya US, Peiris DN, Rhabdomyolysis: A rare presentation of aldosterone-producing adenoma: Indian J Endocrinol Metab, 2013; 17(Suppl1); S237-39
5.. Wang SC, Chiu KY, Primary hyperaldosteronism manifested by rhabdomyolysis: Open J Clin Med Case Rep, 2019; 1519
6.. Cakir I, Senol S, Simsek Y, Primary hyperaldosteronism presenting with rhabdomyolysis in emergency room – Case report: Journal of Acute Disease, 2016; 5(3); 264-66
7.. Zavatto A, Concistrè A, Marinelli C, Hypokalemic rhabdomyolysis: A rare manifestation of primary aldosteronism: Eur Rev Med Pharmacol Sci, 2015; 19; 3910-16
8.. Wu C, Xin J, Xin M, Hypokalemic myopathy in primary aldosteronism: A case report: Exp Ther Med, 2016; 12; 4064-66
9.. Pecnik P, Müller P, Vrabel S, Two cases of hypokalaemic rhabdomyolysis: Same but different: BMJ Case Rep, 2018; 2018; bcr2017223609
10.. Singh D, Chander V, Chopra K, Rhabdomyolysis: Methods find exp clin pharmacol, 2005; 27; 39-48
11.. Knochel JP, Mechanisms of rhabdomyolysis: Curr Opin Rheumatol, 1993; 5; 725-31
12.. Torres PA, Helmestetter JA, Kaye AM, Rhabdomyolysis: Pathogenesis, diagnosis, and treatment: Ochsner J, 2015; 15(1); 58-69
13.. Knochel JP, Schlein EM, On the mechanism of rhabdomyolysis in potassium depletion: J Clin Invest, 1972; 51; 1750
14.. Young WF, Primary aldosteronism: renaissance of a syndrome: Clin Endocrinol (Oxf), 2007; 66; 607-18
15.. Young WF, Diagnosis and treatment of primary aldosteronism: Practical clinical perspectives: J Intern Med, 2019; 285(2); 126-48
16.. Chayovan T, Limumpornpetch P, Hongsakul K, Success rate of adrenal venous sampling and predictors for success: A retrospective study: Pol J Radiol, 2019; 84; e136-41
17.. Kahn SL, Angle JF, Adrenal vein sampling: Tech Vasc Interv Radiol, 2010; 13(2); 110-25
18.. Gonzalez RJ, Shapiro S, Sarlis N, Laparoscopic resection of adrenal cortical carcinoma: A cautionary note: Surgery, 2005; 138; 1078-85
Figures
Tables
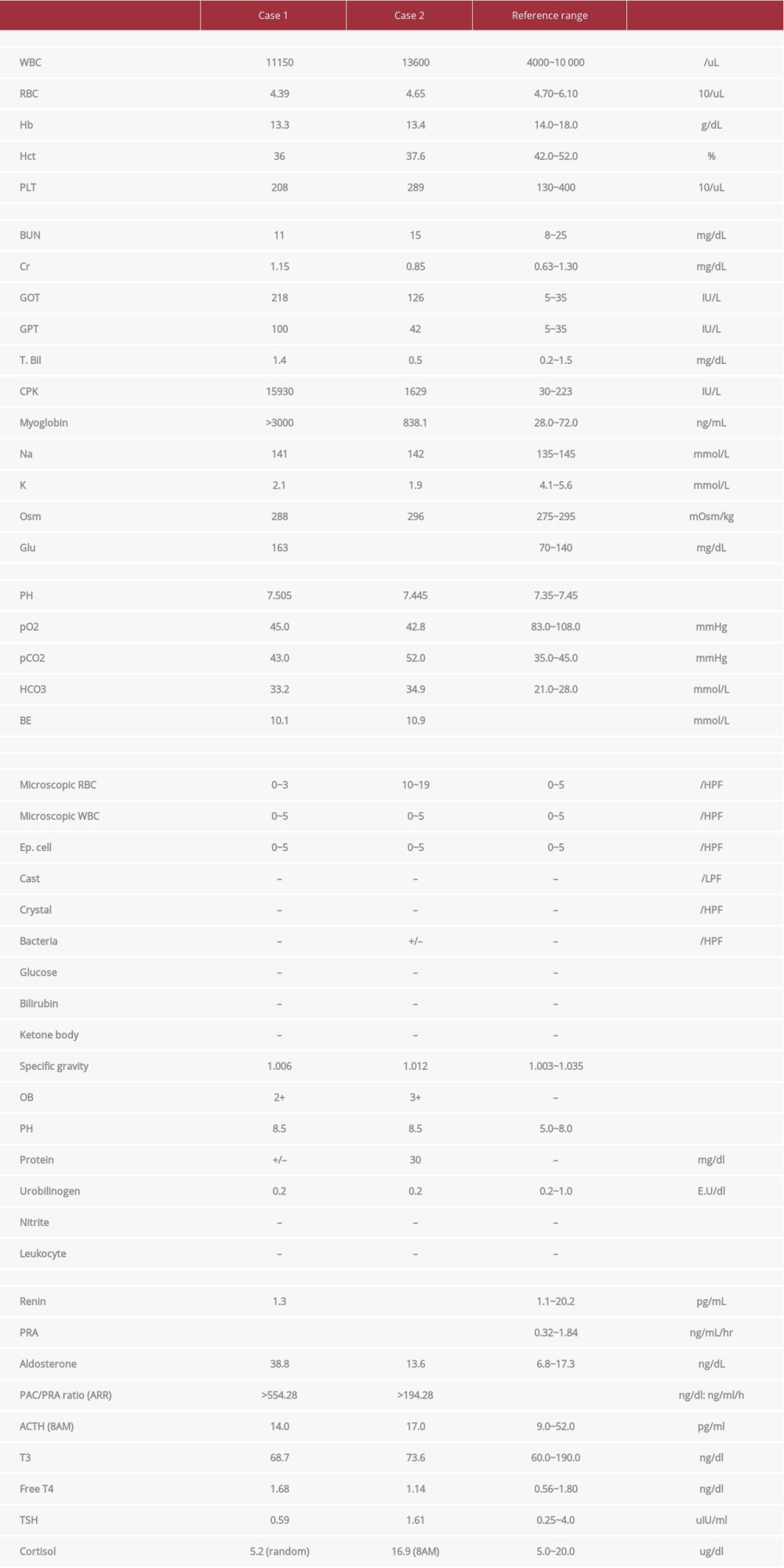 Table 1.. Laboratory data on admission and endocrine data.
Table 1.. Laboratory data on admission and endocrine data.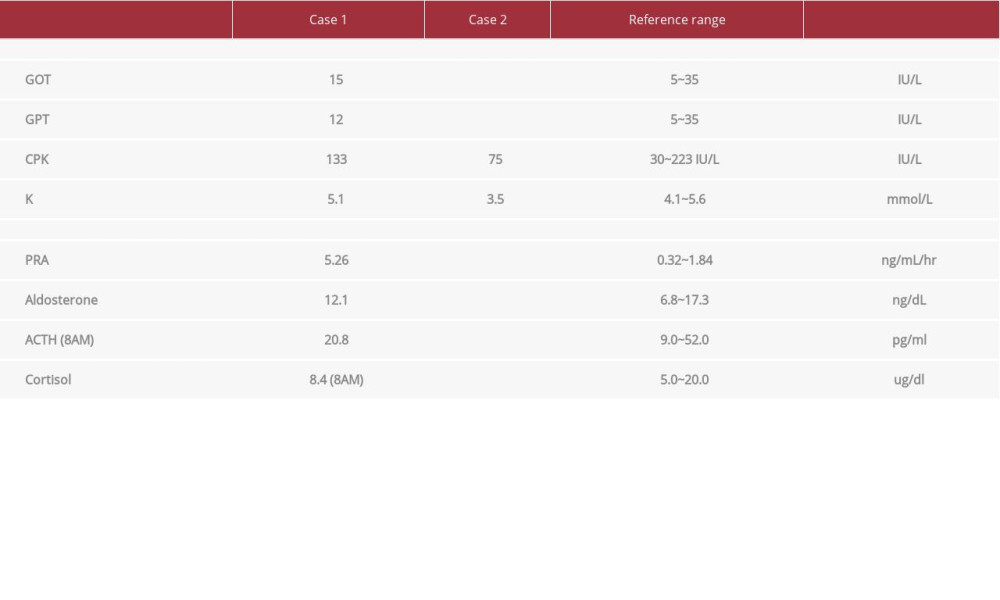 Table 2.. Laboratory data at 3-month follow-up visits and endocrine data at 1-year follow-up visits.
Table 2.. Laboratory data at 3-month follow-up visits and endocrine data at 1-year follow-up visits.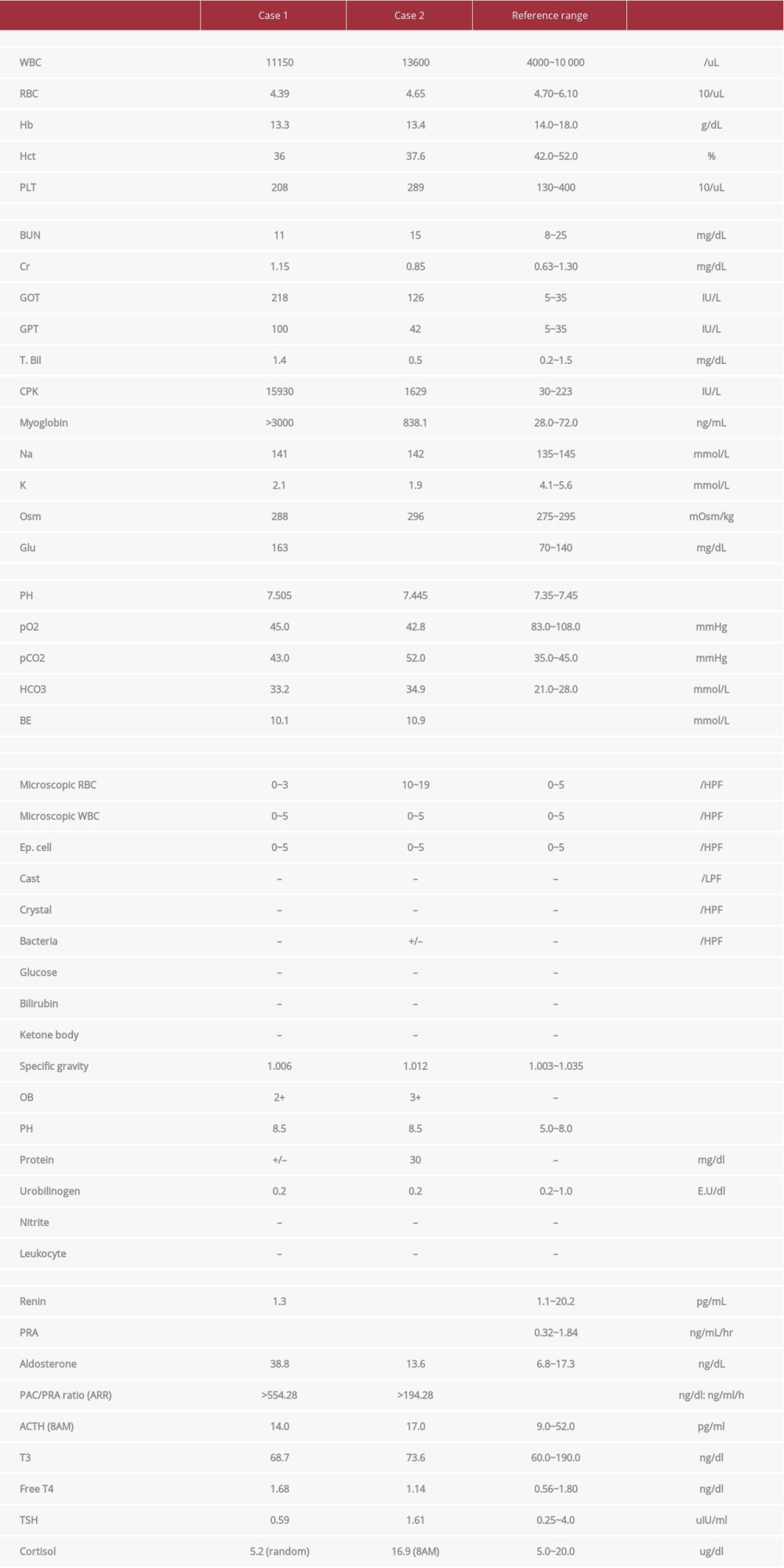 Table 1.. Laboratory data on admission and endocrine data.
Table 1.. Laboratory data on admission and endocrine data.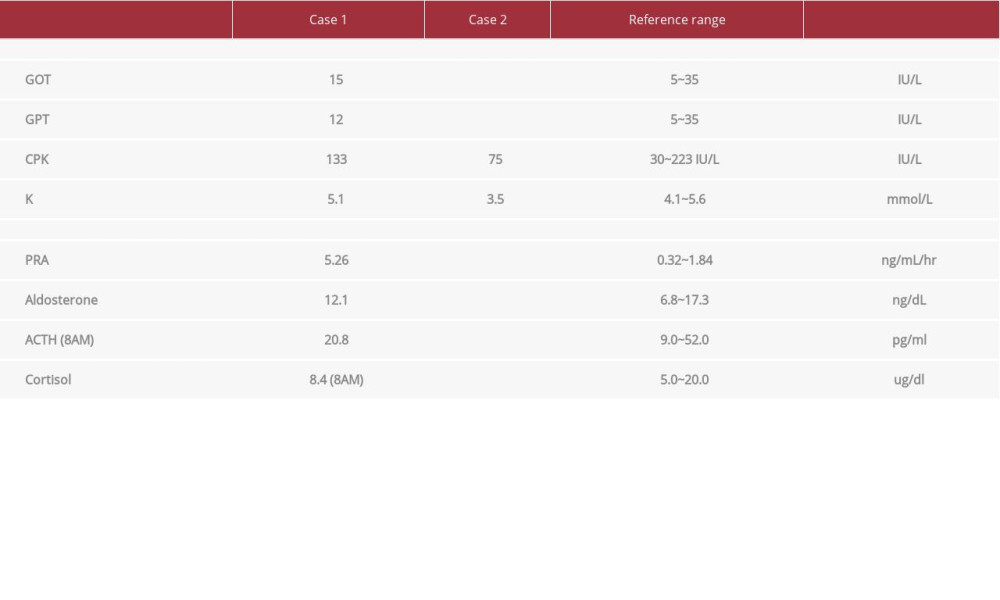 Table 2.. Laboratory data at 3-month follow-up visits and endocrine data at 1-year follow-up visits.
Table 2.. Laboratory data at 3-month follow-up visits and endocrine data at 1-year follow-up visits. In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








