20 April 2021: Articles 
A Case of Reconstruction of a Type IIIc Open Tibial Fracture with Bone Loss and Warm Ischemia Time of 13 Hours: Quality of Life and Review of the Literature
Diagnostic / therapeutic accidents, Management of emergency care
Antonios Kouzelis1ABDE*, Stavros B. Balasis2DE, Aikaterini Bavelou1BCEF, George Ch. Lampropoulos3B, Eleftheria Antoniadou4CDEF, Vasileios Athanasiou1BF, Zinon T. Kokkalis1BF, Andreas Panagopoulos1ADFDOI: 10.12659/AJCR.929993
Am J Case Rep 2021; 22:e929993
Abstract
BACKGROUND: The management of open Gustilo IIIC fractures can be challenging even for experienced orthopedic surgeons. The decision between limb salvage and amputation is extremely difficult and the scoring systems do not seem to affect it significantly. Although ischemic time has been proven to be a major factor, attempts at reconstruction of limbs with ischemic time over 6 hours have been made in past decades. A simultaneous management of skeletal, soft-tissues, and vascular injury should be performed. This requires an orthoplastic surgeon who is capable of doing all the necessary operations by him/herself with hand-surgery and microsurgery expertise.
CASE REPORT: We present a case of a 49-year-old man with a type IIIC open tibial fracture with bone loss and warm ischemia time of 13 hours, who underwent revascularization and reconstruction with good radiological and functional results after a follow-up of 3 years. A few similar cases have been presented in the literature but none of them had a combination of bone loss, severe soft tissue injury, and complete vascular disruption after a crush injury.
CONCLUSIONS: The treatment of type IIIC open fractures of the tibia can be a demanding and time-consuming process. Detailed information about the necessity of multiple surgical interventions must be explained and fully understood by the patient in order to have realistic expectations.
Keywords: Amputation, Traumatic, Fracture Fixation, Intramedullary, Fractures, Comminuted, Skin Transplantation, Tibial Arteries, Tibial Nerve, warm ischemia, Quality of Life, Reconstructive Surgical Procedures, Tibial Fractures
Background
The management of open fractures, especially when vascular injury is involved, is challenging. The annual incidence of open long-bone fractures in the United Kingdom has been reported to be 11.5 per 100 000 persons, with open fractures of the tibial diaphysis being the commonest, with the majority of them caused by traffic accidents [1].
The most widely used classification system for open fractures is that of Gustilo and Anderson, first described in 1976 [2] and then modified in 1984 to reclassify the type III injuries. Type IIIC open fractures were then defined as open fractures associated with arterial injury requiring repair [3].
Historically, open type IIIC tibial fractures have been treated with primary amputation, with studies reporting up to 78% amputation rates [4]. However, in recent decades, with advances in orthopedic, vascular, and plastic surgery, it becomes even more feasible to reconstruct rather than amputate these limbs. There are now studies suggesting that salvage is a cost-saving strategy that offers a better quality of life than amputation [5,6].
Although various scoring systems have been developed, with the Mangled Extremity Severity Score (MESS) being the commonest, when confronted with such an injury, all of them have limited usefulness and cannot safely predict the patients’ functional recovery [7].
Our aim is to present the case of a 49-year-old man with an open type IIIC tibial fracture, as a result of a crush injury, which was successfully reconstructed in our department after a warm ischemia time of 13 hours. To our knowledge, a few similar cases have been presented in the literature but none of them had a combination of bone loss, severe soft tissue injury, and complete vascular disruption after a crush injury.
Case Report
The patient, a 49-year-old man, was transferred to the Emergency Department of our University Hospital after a crush injury of his right tibia. He had a personal history of goiter, smoking, and normal thyroid hormone values. The injury was sustained after a truck door hanger crushed his right limb toward a wall, just over the ankle joint, 11 hours before the patient was transferred to the Emergency Department.
He was initially evaluated according to the ATLS protocol (Advanced Trauma Life Support). No other concomitant or life-threatening injuries were detected and the vital signs of the patient were normal. The musculoskeletal system was assessed thoroughly and the injured limb was neurovascularly examined. Initial images of the limb are presented in Figure 1. During the clinical examination, no distal arterial pulses were detected, not only by palpation of both anterior and posterior tibial artery, but also with the use of a mobile Doppler device. The capillary refill was extremely prolonged and the limb was pale and cold below the injury site. There was minor active bleeding, which was controlled by direct pressure during the initial evaluation of the patient. With regard to the motor and sensory function, despite the fact that active motion is very hard for the surgeon and very painful for the patient, there was a visible movement of the toes and excessive pain of the foot.
Intravenous antibiotics, after discussion with the infectious disease specialists, consisting of a second-generation cephalosporin and metronidazole, were administered to the patient, as well as prophylaxis for tetanus. The patient was transferred for the necessary radiographic evaluation, which revealed a comminuted distal tibial fracture with bone loss of 2 cm and fracture of the fibula at the same level. He was prepped and transferred to the Operating Theater nearly 2 hours after admission. Vascular surgeons were called to be present during the procedure.
Under general anesthesia, a thorough soft tissue and bone debridement was performed. Due to excessive damage of the anterior tibial artery, reconstruction of the posterior tibial artery was finally decided on. After that, the Orthopedic Team placed an in situ transarticular external fixator under fluoroscopy to stabilize the fracture site. A careful examination of the anterior and posterior tibial artery revealed complete disruption of both. The posterior tibial artery was completely ruptured and in very bad condition. Thorough examination of distal and proximal stumps revealed serious damage of the endothelium up to 6–7 cm long. To avoid possible post-operative thrombosis, a 10-cm graft from the major saphenous vein of the ipsilateral thigh was harvested and an end-to-end bypass anastomosis restored the posterior tibial artery blood flow (Figure 2). Revascularization of the artery was checked using a mobile Doppler device.
After an uncomplicated resuscitation, the patient was transferred to the Orthopedic ward, where he was transfused with 1 unit of red blood cells (RBCs). Intravenous antibiotics were continued and administration of oral acetylsalicylic acid (100 mg per day) and subcutaneous 4500 IU tinzaparin per day started.
Four days after the surgery, the patient underwent revision of the external fixation to achieve bone contact to gain more stability and to facilitate bone union. At the same time, a sural fasciocutaneous flap and split-thickness skin grafts were also performed for wound coverage. One month later, an additional debridement and placement of an additional split-thickness skin graft was also carried out (Figure 3).
The patient was discharged 34 days after admission, with a prescription for acetylsalicylic acid (100 mg per day), tinzaparin (subcutaneously, 4500 IU per day). He was advised to mobilize the knee joint and to use 2 crutches without bearing weight on the injured leg.
The last operation was performed 159 days after the first admission. Since for 5 consecutive months the radiological appearance of the fracture site did not demonstrate signs of callus formation, intramedullary nailing of the tibia was decided in order to achieve bone union. Four months later, a 3-column callus was detected in the radiological examination. The patient could bear weight with minimum pain and demonstrated a fixed plantar flexion deformity due to long-term application of the transarticular external fixation in an equinus position. Three years after the last operation, the clinical and radiological appearance of the leg was excellent (Figure 4).
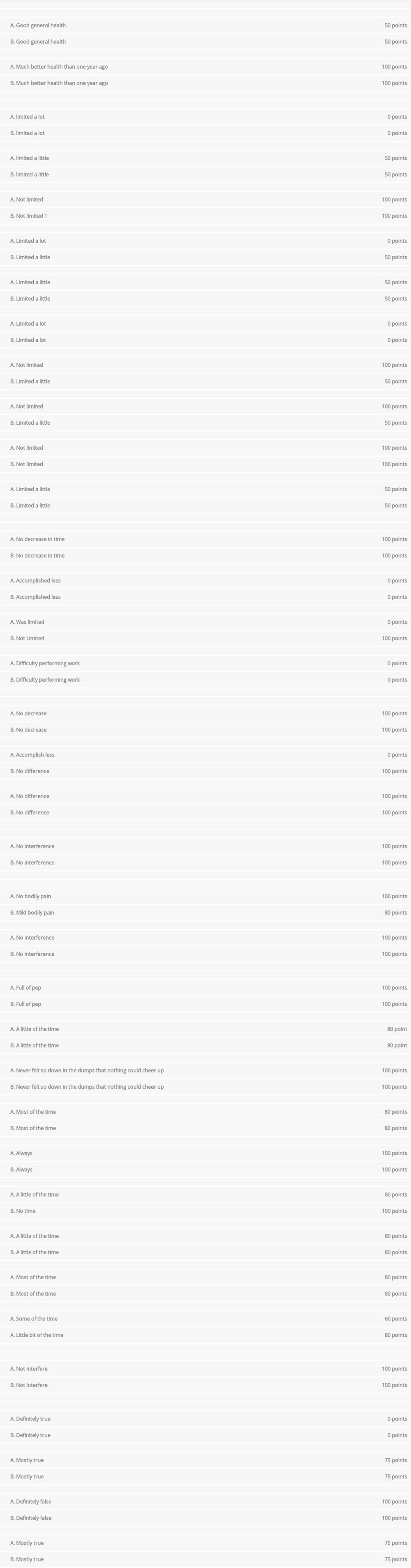
We also wanted to evaluate the impact of such a lengthy treatment process on the quality of life and overall health of the patient, as well as the perception of the same by the caregiver (his wife). For this purpose, we used the SF-36 questionnaire, which is very descriptive tool addressing quality of life and is translated and validated into Greek [8,9]. Results were excellent, and both patient and primary caregiver gave high ratings (Table 1). In particular, the patient reported that the worst outcome was role limitation due to physical health (25%) and the best outcomes were social functioning, general health, and pain (100%). The caregiver rated the worst outcome as role limitation due to physical health and physical functioning (50%) and the best outcomes were role limitations due to emotional problems, social functioning, and health change (100%).
Discussion
The treatment of open fractures can be challenging even for experienced orthopedic surgeons. When an open fracture is complicated with vascular injury requiring reconstruction, the demands are even higher. Simultaneous management of skeletal, soft-tissues, and vascular injury should be performed. This requires an orthoplastic surgeon who is capable of doing all the necessary operations by him/herself, with hand-surgery and microsurgery expertise.
The timely and accurate diagnosis of these kinds of injuries is of paramount importance for successful vascular repair and thus successful salvage of the limb. When vascular injuries and serious soft tissue damage are detected, early surgical intervention is desirable.
As Fowler et al stated in their meta-analysis, ischemic time should be considered a relative, not an absolute, predictor of amputation. They also found that surgical sequence does not affect the rate of amputations. There was no significant difference in the incidence of amputation between fracture fixation being performed after vs before revascularization [10]. There are also various studies in the literature reporting improved outcomes and low amputation rates, even with ischemic time more than 10 hours [11,12]. However, there are reviews like the one from Tunali et al, that reported that reducing ischemic time is vital for limb salvage, stating that patients with ischemia time more than 6 hours had higher risk for amputation, but, even so, more than half of them were salvaged in their study [13].
In addition to concern for the vascular status of the limb, immediate response is also needed to decrease the infection and nonunion rates. The “6-hour rule” was first proposed by Friedrich in 1898, when he observed that the effectiveness of debridement is limited if performed >6 hours after the injury [14]. This was later confirmed by Robson et al, who demonstrated that the time period needed for bacteria to reach a level of >105 per gram of tissue is a mean time of 5.71 hours after injury [15]. However, during the last decades, this has been questioned. There are studies suggesting that a delay of more than 6 hours in the primary debridement of open tibial fractures can be justified and evidence shows no statistically significant difference in overall and deep infection rates between fractures debrided within 6 hours and those debrided at more than 6 hours [16].
Regarding the arterial injury, it was found that the anterior tibial artery is more commonly injured (31.9%) in comparison with the posterior tibial artery, which has an injury rate of 8.9%. This study also demonstrated an injury rate of both anterior and posterior tibial arteries of 3.1% and of 2.1% of all 3 vessels. In general, the presence of a vascular injury has been proven to affect the functional outcome of patients following reconstruction [17], with reports suggesting that open fractures with injury to the posterior tibial artery had a significantly higher nonunion rate and delayed union than fractures without vascular injury [18].
As for the type of fixation used for this kind of injury, there are studies recommending primary external fixation for all fractures where the soft tissue cannot be initially closed [19], but also others who report that high rates (68.5%) of open fractures treated primarily with external fixator required at least 1 further operation to achieve union [20]. This was also demonstrated in our case, where a modification of the external fixation was required 4 days after the first operation and the definitive treatment was an intramedullary nail 159 days after the initial injury to achieve union.
It was also suggested that scoring systems are not predictive of functional recovery, and other factors can also influence the decision to salvage limbs, such as the extent of the soft tissue injury [7,13,20]. There are reviews demonstrating that there is no evidence supporting superior outcomes of either limb salvage or primary amputation [22], and reporting that amputation yields fewer quality-adjusted life years saved (QUALYs) and is associated with increased anxiety and depression [23]. As a result, it appears that patient may have different opinions that affect quality of life. This was also demonstrated by Pelissier et al, who reported that all of the patients with successful reconstructions in their study preferred their salvaged leg to an amputation [24].
In our case, in a 49-year-old heavy smoker, with a type IIIc open fracture with ischemia more than 10 hours, the obvious choice was a below-knee amputation. However, considering the strong will of the patient, his occupation demands (sheep breeder), the preservation of plantar sensation in the foot, and the recent considerations of the literature, we decided, having plastic and vascular surgeons available, to proceed with limb salvage.
Moreover, we investigated how the results of the procedure affected the patient’s life. We used the SF-36 questionnaire in a throughout investigation involving both the patient and his primary caregiver. The results were excellent for social functioning, pain, and health change (all scored 100%), very good for energy/fatigue (85%), emotional well-being (84%), and general health (80%), good for physical functioning (55%) and role limitations due to emotional problems (66.7%), and relatively poor for role limitations due to physical health (25%). The alternative of this procedure would be a below-knee amputation. Quality of life measured by the same SF-36 questionnaire is disappointing for patients in many aspects [24]. Godoy et al found responses to 6 of the 8 questions in the test were inadequate, suggesting an unsatisfactory quality of life of the amputees. The most obviously unacceptable attributes were physical, which demonstrates how much the mutilation affects patient quality of life. The physical capacity was also much affected by the surgery, as were the emotional aspects, the general state of health, and the social aspects. Pain interfered with the lives of these patients in a significant way, reducing the quality of life even more. Mental health and vitality were not affected. The emotional burden demonstrates that patients find the loss of the limb very difficult to accept and the quality of life does not improve with time. From all the above, we can conclude that even though the procedure is lengthy and expensive, the outcomes for the patients are really very good.
Conclusions
The treatment of type IIIC open fractures of the tibia can be a demanding and time-consuming process. Detailed information about the necessity of multiple surgical interventions must be explained and fully understood by the patient in order to have realistic expectations and achieve the best possible outcome.
Figures
References:
1.. Court-Brown CM, Rimmer S, Prakash U, The epidemiology of open long bone fractures: Injury, 1998; 29(7); 529-34
2.. Gustilo RB, Mendoza RM, Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses: J Trauma, 1984; 24(8); 742-46
3.. Gustilo RB, Mendoza RM, Williams DN, Problems in the management of type III (Severe) open fractures: A new classification of type III open fractures: J Trauma, 1984; 24(8); 742-46
4.. Flint LM, Arterial injuries with lower extremity fracture: Surgery, 1983; 93(1); 5-8
5.. Chung KC, Saddawi-Konefka D, Haase SC, A cost-utility analysis of amputation versus salvage for gustilo type IIIB and IIIC open tibial fractures: Plast Reconstr Surg, 2009; 124(6); 1965-73
6.. MacKenzie EJ, Health-care costs associated with amputation or reconstruction of a limb-threatening injury: J Bone Jt Surg, 2007; 89(8); 1685-92
7.. Schirò GR, Sessa S, Piccioli A, Primary amputation vs limb salvage in mangled extremity: A systematic review of the current scoring system: BMC Musculoskelet Disord, 2015; 16(1); 1-7
8.. Ware JE, Sherbourne CD, The MOS 36-item short-form health survey (SF-36). I.Conceptual framework and item selection: Med Care, 1992; 30(6); 473-83
9.. Pappa E, Kontodimopoulos N, Niakas D, Validating and norming of the greek SF-36 health survey: Qual Life Res, 2005; 14(5); 1433-38
10.. Fowler J, MacIntyre N, Rehman S, The importance of surgical sequence in the treatment of lower extremity injuries with concomitant vascular injury: A meta-analysis: Injury, 2009; 40(1); 72-76
11.. Drost TF, Rosemurgy AS, Kearney RE, Outcome of treatment of combined orthopedic and arterial trauma to the lower extremity: J Trauma, 1989; 29(1); 1331-34
12.. Bishara RA, Improved results in the treatment of civilian vascular injuries associated with fractures and dislocations: J Vasc Surg, 1986; 3(5); 707-11
13.. Tunali O, Gustilo type IIIC open tibia fractures with vascular repair: Minimum 2-year follow-up: Eur J Trauma Emerg Surg, 2017; 43(4); 505-12
14.. Friedrich PL, Die aseptische versorgung frischer wunden: Archiv für Klinische Chirurgie, 1898; 57; 288-310 [in German]
15.. Robson MC, Duke WF, Krizek TJ, Rapid bacterial screening in the treatment of civilian wounds: J Surg Res, 1973; 14(5); 426-30
16.. Prodromidis AD, Charalambous CP, The 6-hour rule for surgical debridement of open tibial fractures: A systematic review and meta-analysis of infection and nonunion rates: J Orthop Trauma, 2016; 30(7); 397-402
17.. Chummun S, Wigglesworth TA, Young K, Does vascular injury affect the outcome of open tibial fractures: Plast Reconstr Surg, 2013; 131(2); 303-9
18.. Brinker MR, Bailey DE, Fracture healing in tibia fractures with an associated vascular injury: J Trauma, 1997; 42(1); 11-19
19.. Faschingbauer M, Meiners J, Schulz AP, Operative treatment and soft tissue management of open distal tibial fractures – pitfalls and results: Eur J Trauma Emerg Surg, 2009; 35(6); 527-31
20.. Giannoudis PV, Papakostidis , Roberts C, A review of the management of open fractures of the tibia and femur: J Bone Jt Surg, 2006; 88(3); 281-89
21.. Swiontkowski MF, MacKenzie EJ, Bosse MJ, Factors influencing the decision to amputate or reconstruct after high-energy lower extremity trauma: J Trauma, 2002; 52(4); 641-49
22.. Saddawi-Konefka D, Kim HM, A systematic review of outcomes and complications of reconstruction and amputation for type IIIB and IIIC fractures of the tibia: Plast Reconstr Surg, 2008; 122(6); 1796-805
23.. Soni A, Tzafetta K, Knight S, Gustilo IIIC fractures in the lower limb: J Bone Jt Surg, 2012; 94(5); 698-703
24.. Pelissier P, Boireau P, Martin D, Bone reconstruction of the lower extremity: Complications and outcomes: Plast Reconstr Surg, 2003; 111(7); 2223-29
25.. De Godoy JMP, Braile DM, Buzatto SHG, Quality of life after amputation: Psychol Heal Med, 2002; 7(4); 397-400
Figures
In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250