12 April 2021: Articles 
Delayed Endovascular Thrombectomy for Ischemic Stroke in a Young Woman with No Known Risk Factors: A Case Report
Unusual clinical course, Challenging differential diagnosis, Management of emergency care, Clinical situation which can not be reproduced for ethical reasons
Bryce D. Beutler1DEF*, Rajesh Rangaswamy234AB, Richard D. King45ABE, Burton J. Tabaac467ADEFDOI: 10.12659/AJCR.930291
Am J Case Rep 2021; 22:e930291
Abstract
BACKGROUND: National guidelines and consensus statements suggest a 24-hour window for endovascular recanalization in patients presenting with acute ischemic stroke due to large-vessel occlusion. However, the safety and efficacy of extending the window for intervention remains to be definitively established.
CASE REPORT: A healthy 26-year-old woman presented with headache, left-sided hemiplegia, and rightward gaze palsy 2 days after a minor trauma. Time last known well was approximately 50 hours prior to presentation. Computed tomography angiography revealed dissection of the distal right internal carotid artery and occlusion of the M1 segment of the right middle cerebral artery. Magnetic resonance imaging showed a small area of acute infarct in the right basal ganglia and right insular cortex, but suggested a large ischemic penumbra; this was confirmed with cerebral perfusion analysis. In light of the patient’s young age and potential for penumbral salvage, mechanical thrombectomy of an M1 thrombus and stenting of an internal carotid artery dissection were performed nearly 60 hours after the onset of symptoms. The patient demonstrated marked clinical improvement over the following days and was discharged home in excellent condition one week after presentation. Based on our clinical experience and other emerging data, we propose that extension of the 24-hour window for endovascular intervention may improve functional outcomes among select individuals.
CONCLUSIONS: A 24-hour window for endovascular thrombectomy is appropriate for many patients presenting with acute ischemic stroke. However, in select individuals, extension of the window to 48 hours or beyond may improve functional outcomes.
Keywords: Neuroimaging, Stroke, Thrombectomy, Brain Ischemia, Carotid Artery, Internal, endovascular procedures, ischemic stroke
Background
Current clinical guidelines for the early management of patients with acute ischemic stroke suggest a 24-hour window for endovascular recanalization [1–3]. However, extending the window beyond 24 hours may result in a favorable outcome; emerging evidence indicates that clinical and imaging findings, rather than time last known well (TLKW), should guide management in the setting of ischemic stroke. Indeed, in select patients, endovascular intervention may improve outcomes even when performed days after symptom onset. We describe a 26-year-old woman who presented with a two-day history of progressively worsening neurologic deficits who demonstrated marked clinical improvement following endovascular stenting and thrombectomy. Written informed consent was obtained for the publication of case details.
Case Report
A 26-year-old woman presented to the Emergency Department complaining of headache and weakness. The patient explained that she had suffered a minor ground-level fall without apparent injury 3 days earlier; she had returned to her usual state of health upon going to bed that evening (TLKW). Upon waking the following morning, she began to experience a constant throbbing occipital and right temporal headache (8 hours since TLKW). In addition, she described the insidious onset of predominantly left-sided weakness. Symptoms progressively worsened over the following 2 days, prompting the patient to finally seek care in the Emergency Department (50 hours since TLKW).
The patient had been healthy prior to the onset of symptoms. She took daily oral contraceptive pills, but no other prescription medications or supplements. There was no personal or family history of atherosclerotic disease or hypercoagulability syndrome, nor was there a personal history of thrombosis or miscarriage. The patient denied use of alcohol or tobacco, but did endorse weekly marijuana use.
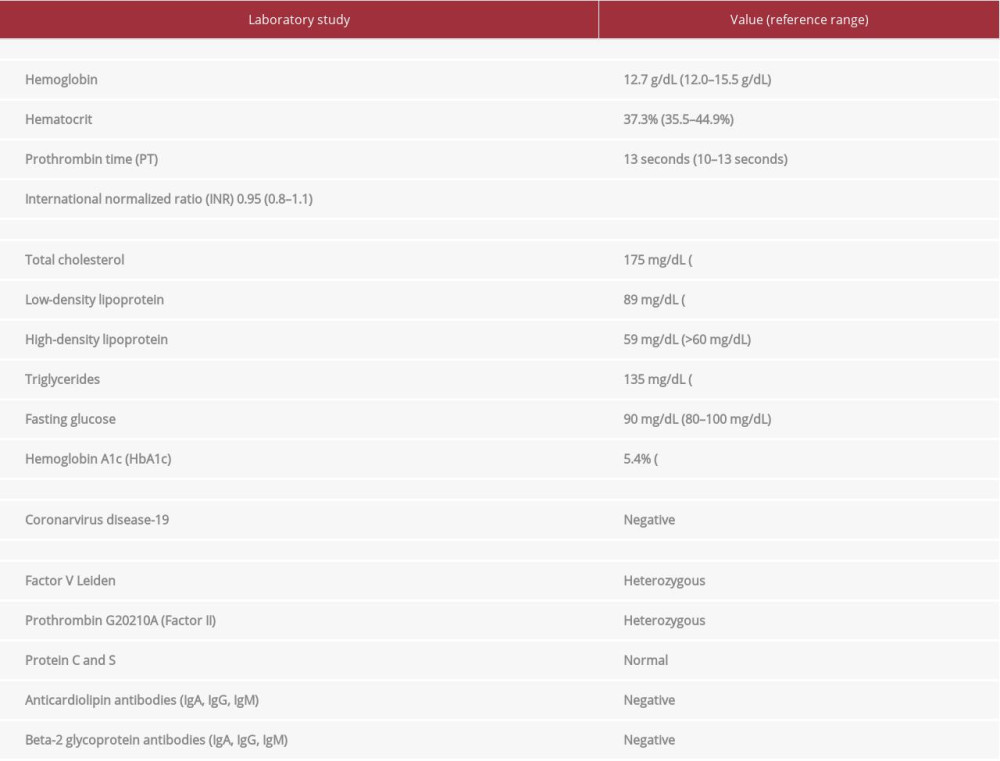
The patient was slightly tachypneic on presentation (temperature: 36.4°C; blood pressure: 122/63 mmHg; heart rate: 60 beats per minute; respiratory rate: 18 respirations per minute; oxygen saturation: 99%). Physical examination revealed a partial right gaze palsy, left facial paresis, dysarthria, left hemisensory loss of 90% as compared to the right, and unilateral motor weakness (3/5 left upper-extremity strength and 0/5 left lower-extremity strength). National Institutes of Health Stroke Scale (NIHSS) score was 15. Initial laboratory studies for stroke risk factors were unremarkable (total cholesterol: 175 mg/dL [low-density lipoprotein: 89 mg/dL, high-density lipoprotein: 59 mg/dL], triglycerides: 135 mg/dL, hemoglobin A1c: 5.4%). Fasting blood glucose was 90 mg/dL. Hematologic studies were within normal limits (prothrombin time: 13 seconds, international normalized ratio: 0.95, hemoglobin: 12.7 g/dL, hematocrit: 37.3%). The patient tested negative for coronavirus disease-19 (Table 1).
A non-contrast computed tomography (CT) scan of the head was obtained and demonstrated a region of hypodensity within the right insular ribbon; Alberta Stroke Program Early CT Score (ASPECTS) was 9. CT angiography showed occlusion of the supraclinoid segment of the right internal carotid artery (ICA) and M1 segment of the middle cerebral artery (MCA) (Figure 1). Findings were further characterized with magnetic resonance angiography (MRA), which showed a proximal right ICA occlusion with intramural thrombus (Figures 2, 3). Magnetic resonance imaging showed only a small area of acute infarct in the right basal ganglia and right insular cortex (Figure 4); this was confirmed on CT cerebral perfusion analysis, which demonstrated a completed infarct volume of 5 milliliters (mL) and mismatched volume representing ischemic brain/penumbra of 17 mL. Tmax greater than 6 seconds representing combination of completed infarct and ischemia was 22 mL (Figure 5). Correlation of the clinical presentation and imaging findings suggested a small ischemic stroke with a comparatively large penumbra. The patient was immediately started on aspirin 81 milligrams.
The case was discussed with the neurology and neurointerventional radiology teams, who concluded that, in light of the patient’s young age, large penumbra, and risk for complete infarction, the potential benefits of endovascular recanalization outweighed any potential risks. The patient and her family agreed.
The patient was transported to the angiography lab approximately 4.5 hours after presentation and nearly 55 hours since TLKW. A right cervical carotid angiogram demonstrated dissection of the right internal carotid origin with intramural hematoma (Figure 6). A right internal carotid stent was placed across the dissected segment with an embolic protection device (Figure 7). The subsequent angiogram demonstrated a right supraclinoid segment occluded by thrombus; aspiration thrombectomy was performed. After multiple aspirations, a modified treatment in cerebral ischemia (mTICI) score of 2a was achieved. Immediately after the mTICI 2a reperfusion, the patient began moving her left upper and lower extremities, suggesting significant improvement. It was therefore decided not to remove a small distal M2 segment thrombus so as to minimize the potential for adverse events. Post-thrombectomy angiography showed patency of the ICA and M1 segment (Figure 8).
Antiplatelet drugs were not administered immediately following the procedure in order to reduce the risk of hemorrhagic conversion of the right basal ganglia infarct. A follow-up MRA obtained on Oct 5 was significant for non-visualization of the right common carotid artery and right ICA, indicating carotid stent occlusion. However, there was reconstitution of the supraclinoid portion of the right ICA, likely via the patent posterior communicating and anterior communicating arteries (Figure 9). A subsequent MRI demonstrated stable infarcts in the insular region and basal ganglia with a patent right supraclinoid right internal carotid artery.
The patient began participating in physical, occupational, and speech therapy on Oct 5. Aspirin 81 milligrams daily was continued and atorvastatin 40 milligrams nightly was started for secondary prevention. Dual antiplatelet therapy was not indicated, given the stent occlusion. Re-evaluation by the neurology team revealed marked improvement in function. The patient exhibited complete resolution of gaze palsy and dysarthria. Left hemisensory loss has improved from a decrease of 90% to 30%. Left upper-extremity motor strength had improved to 4+/5 (previously 3/5) and left lower-extremity motor strength had improved to 4–/5 (previously 0/5). The patient was discharged home on Oct 7 with an NIHSS score of 5. Aspirin 81 and atorvastatin were continued.
A comprehensive stroke workup revealed that the patient was heterozygous for the factor V Leiden gene mutation. In addition, prothrombin G20210A (Factor II) DNA analysis was positive for a heterozygous mutation. Protein C and S, antithrombin III, beta-2 glycoprotein antibodies, and anticardiolipin antibodies were all within normal limits (Table 1). A 2D echocardiogram with bubble study showed evidence of an early right-to-left shunt suggestive of atrial septal defect or patent foramen ovale. The findings were discussed in detail with neuroradiology and neurointerventional specialists, who confirmed that the MRA and intraprocedural angiography definitively demonstrated dissection at the proximal ICA. However, it was also emphasized that the presence of a dissection did not necessarily exclude other causes of stroke. Given the patient’s thrombotic risk factors, including a right-to-left intracardiac shunt, oral contraceptive use, and factor V Leiden and prothrombin G20210A heterozygosity, it was postulated that a paradoxical embolism may have occurred prior to or in parallel with the traumatic dissection. Further history was most suggestive of the former hypothesis, as the patient noted that she had experienced transient episodes of left-sided weakness months prior to her presentation in the Emergency Department.
The patient agreed to switch to progestin-only contraceptives given her increased risk for thrombosis and continued to participate in outpatient physical and occupational therapy. Modified Rankin Scale for Neurologic Disability at 90 days was 1. No further episodes of stroke-like symptoms have been reported.
Discussion
In 2015, MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) demonstrated that patients who underwent early endovascular mechanical thrombectomy (EVT) experienced superior functional outcomes as compared to those who received standard medical therapy alone [4]. The results of several other trials subsequently established EVT as the standard of care for patients with acute ischemic stroke due to large-vessel occlusion who presented within 6 hours of symptom onset [5–7]. Three years later, the DEFUSE-3 (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke) trial provided evidence that the six-hour window for EVT could be extended to 16 hours among individuals presenting with neurologic deficits that were out of proportion to infarct size [2]; this was later extended to 24 hours in the DAWN (DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake-Up and Late Presenting Strokes Undergoing Neurointervention with Trevo) trial [3]. The 24-hour window for EVT has since been integrated into national guidelines for the management of acute ischemic stroke [1].
The DEFUSE-3 and DAWN trials marked a paradigm shift in the management of acute ischemic stroke, introducing a patient selection model predicated on perfusion and penumbra rather than time last known well (TLKW). Patients included in the DEFUSE-3 trial had a small initial infarct volume (less than 70 mL) and relatively large penumbra (15 mL or more), while the DAWN trial used clinical core mismatch to determine patient eligibility. Both studies represented a significant departure from the time window dogma and established that a physiology- and imaging-based approach to management could improve outcomes among patients in whom standard medical therapy would offer marginal benefit.
Emerging evidence suggests that the EVT window can be extended well beyond 24 hours. A 2018 retrospective review by Desai et al concluded that EVT is safe and effective in patients with acute ischemic stroke due to large-vessel occlusion who present up to 156 hours after symptom onset [8]. In addition, a case report by Aguilar-Salinas et al describes remarkable improvement in a woman who underwent EVT nearly one week after TLWK [9]. A more recent study demonstrated that the window for EVT may be extended even beyond one week. In a 2020 case-control study of 150 patients with acute ischemic stroke due to internal carotid or middle cerebral artery occlusion who had salvageable brain tissue and an NIHSS score of 6 or greater, Kim et al found that EVT was associated with better outcomes than medical therapy alone, including among patients presenting up to 10 days after TLKW [10]. However, no other major studies have since examined a fundamental question of stroke management: when, if ever, does the EVT window close? The data unequivocally show that patient selection should be individualized based on clinical presentation, imaging, and perfusion analysis; thus, it is reasonable to question the value of TLKW in evaluating patient eligibility for EVT. Indeed, our 26-year-old patient was conceivably spared lifelong disability by looking outside the arbitrary 24-hour window.
Patient selection in the DAWN trial was based on 3 major inclusion criteria: (1) radiologic evidence of large-vessel occlusion; (2) mismatch between the severity of the neurologic deficit and infarct volume, with a minimum NIHSS score of 10 for patients with an infarct volume of less than 31 mL and minimum NIHSS score of 20 for patients with an infarct volume of 31–51 mL; and (3) TLKW 6–24 hours prior to presentation. We advocate for a similar patient selection model based on correlation of clinical presentation and tissue perfusion. However, TLKW, beyond the 4.5-hour tissue plasminogen window, should not be used to determine eligibility. Furthermore, we believe that select individuals with an NIHSS below 10 should be considered for EVT; this decision should be based on baseline functional status, co-morbidities, patient goals, and possible outcomes.
Conclusion
In conclusion, there is a paucity of data pertaining to late EVT in the setting of acute ischemic stroke due to large-vessel occlusion. However, the results of the recent study by Kim et al and our experience with EVT in a patient presenting 2 days after LKTW provide further evidence supporting a clinical- and imaging-based approach to patient selection rather than relying on the current 24-hour time window guideline. Large-scale prospective studies are warranted to examine the value of the time window for EVT, if any, and identify which patients are most likely to benefit from late intervention.
Figures
References:
1.. Warner JJ, Harrington RA, Sacco RL, Elkind MSV, Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: Stroke, 2019; 50(12); 3331-32
2.. Albers GW, Marks MP, Kemp S, Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging: N Engl J Med, 2018; 378(8); 708-18
3.. Nogueira RG, Jadhav AP, Haussen DC, Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct: N Engl J Med, 2018; 378(1); 11-21
4.. Berkhemer OA, Fransen PS, Beumer D, A randomized trial of intraarterial treatment for acute ischemic stroke: N Engl J Med, 2015; 372(1); 11-20
5.. Chen CJ, Ding D, Starke RM, Endovascular vs medical management of acute ischemic stroke: Neurology, 2015; 85(22); 1980-90
6.. Jovin TG, Chamorro A, Cobo E, Thrombectomy within 8 hours after symptom onset in ischemic stroke: N Engl J Med, 2015; 372(24); 2296-306
7.. Goyal M, Menon BK, van Zwam WH, Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials: Lancet, 2016; 387(10029); 1723-31
8.. Desai SM, Haussen DC, Aghaebrahim A, Thrombectomy 24 hours after stroke: beyond DAWN: J Neurointerv Surg, 2018; 10(11); 1039-42
9.. Aguilar-Salinas P, Santos R, Granja MF, Revisiting the therapeutic time window dogma: Successful thrombectomy 6 days after stroke onset: BMJ Case Rep, 2018; 2018; bcr2018014039
10.. Kim BJ, Menon BK, Kim JY, Endovascular treatment after stroke due to large vessel occlusion for patients presenting very late from time last known well: JAMA Neurol, 2020 [Online ahead of print]
Figures
In Press
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.941835
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250