27 March 2021: Articles 
Minimal Change Disease After Elective Surgical Abortion: A Case Report
Unusual clinical course, Rare disease
Sheldon Greenberg1ABCDEF*, Kundan R. Jana1ABCDEF, Kalyana C. Janga1ABCDEF, Kamlesh Kumar1BDOI: 10.12659/AJCR.930292
Am J Case Rep 2021; 22:e930292
Abstract
BACKGROUND: Pregnancy causes a physiological increase in renal blood flow and glomerular filtration rate, which leads to a transient increase in urinary protein excretion. Up to 300 mg/d proteinuria is known to occur in pregnancy due to physiological changes. Proteinuria of greater than 3 g/d is categorized as being within the nephrotic range, and the most common cause of nephrotic range proteinuria in the later stages of pregnancy is preeclampsia. Minimal change disease (MCD) as a cause of nephrotic syndrome is rare in pregnancy and is rarer still after abortion. Here, we report a patient who presented with nephrotic syndrome due to MCD after elective surgical abortion.
CASE REPORT: A 21-year-old woman presented with shortness of breath, worsening anasarca, abdominal distension, and weight gain 3 weeks after undergoing elective surgical abortion at 7 weeks of gestation. There was no hematuria and no past medical history or family history of kidney disease. Investigations revealed normal serum creatinine with hypoalbuminemia, dyslipidemia, nephrotic range proteinuria, and negative serology for autoimmune diseases. Renal biopsy showed podocyte effacement with normal glomeruli and intact tubulointerstitium, confirming the diagnosis of MCD. The patient was treated with steroids, antidiuretics, statins, and angiotensin receptor blockers. She responded well, showing symptomatic improvement and resolution of proteinuria, hypoalbuminemia, and dyslipidemia. She was gradually tapered off steroids during subsequent follow-up visits.
CONCLUSIONS: Only a single case of a patient presenting with acute renal failure and MCD after a missed abortion has been reported. To the best of our knowledge, this is the second case report of MCD after abortion and the first report of a patient with MCD without acute renal failure after elective termination of pregnancy.
Keywords: Abortion, Induced, Nephrosis, Lipoid, nephrotic syndrome, Kidney Diseases, Kidney Glomerulus, Pregnancy, Proteinuria, young adult
Background
A normal range proteinuria of up to 300 mg/d is known to occur in pregnancy, and it principally consists of tubular and glomerular protein [1]. Nephrotic syndrome is defined as proteinuria of more than 3 g/d with hypoalbuminemia and is often associated with edema and hypercholesterolemia. The incidence of nephrotic syndrome in pregnancy is 0.012–0.025% [2]. The most common cause of nephrotic range proteinuria in pregnancy after 20 weeks of gestational age is preeclampsia. Proteinuria before 20 weeks of gestation is usually suggestive of an underlying renal disease [3].
There have been very few reports of patients with minimal change disease (MCD) as a cause of nephrotic syndrome during pregnancy. The literature contains only a single case report of MCD with acute renal failure in a patient with a missed abortion [4]. In the current case report, we describe a patient who presented with anasarca after undergoing elective surgical abortion at 7 weeks of gestation and was found to have nephrotic syndrome due to MCD on renal biopsy
Case Report
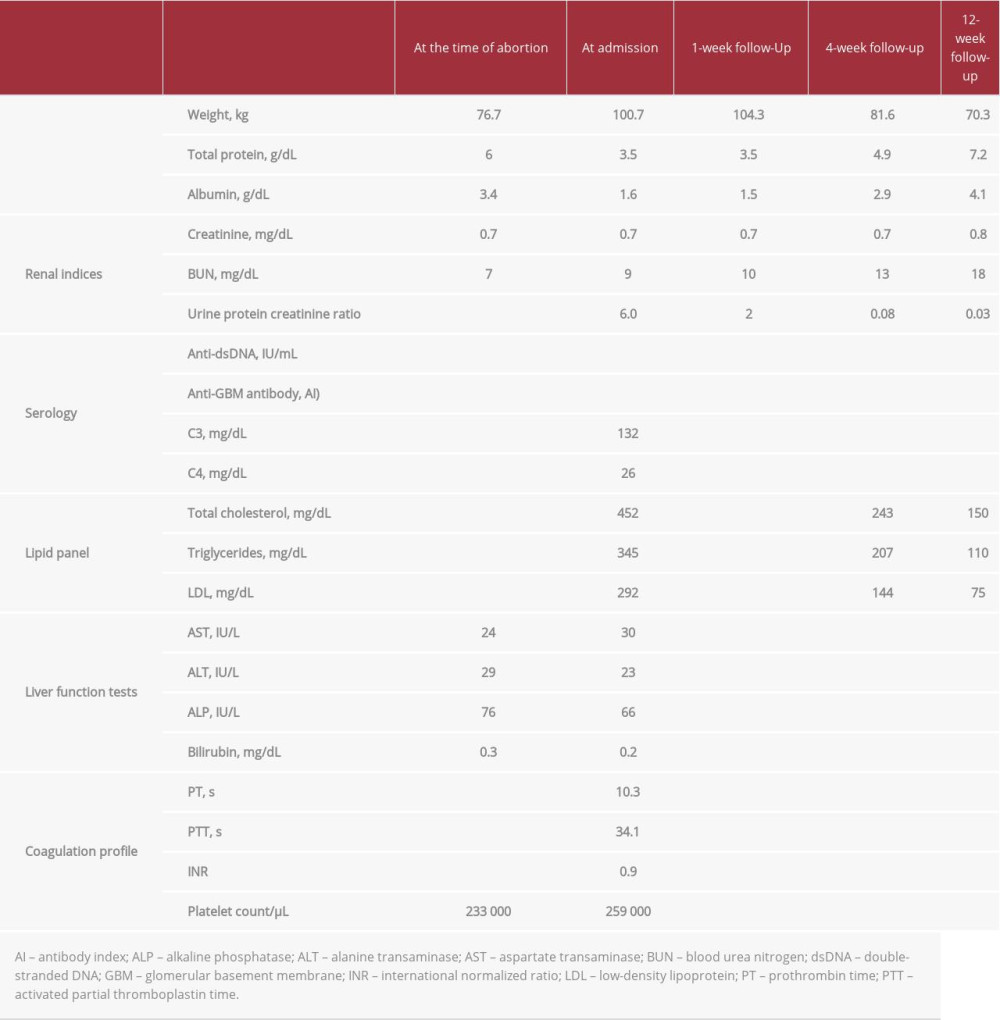
A 21-year-old woman presented with complaints of worsening anasarca for the past 3 weeks. She had undergone a surgical abortion 3 weeks before for nonmedical social reasons. She noticed bilateral lower extremity edema 3 days after the abortion. The edema progressively worsened during the following weeks, and she developed periorbital edema, sacral edema, abdominal distension, and shortness of breath. The patient also stated that she gained 25 kg in the last 3 weeks. She denied fever, cough, chest pain, nausea, vomiting, abdominal pain, or any urinary symptoms. She had no significant past medical history or family history. This pregnancy was her fourth. Obstetric history was significant for complete spontaneous abortion in her first pregnancy at 6 weeks gestational age. Subsequently, the patient had 2 healthy children, now aged 2.5 years and 1 year, through normal vaginal delivery without any complications. Urinary analysis during her third pregnancy showed no proteinuria, with serum albumin of 4.3 g/dL. During her fourth pregnancy, the patient elected to undergo a surgical abortion at 7 weeks 3 days gestational age. She had an albumin of 3.4 g/dL and serum creatinine of 0.7 mg/dL at the time of abortion (Table 1). Elective termination of pregnancy was performed by suction dilatation and curettage under aseptic conditions. Minimal bleeding was noted, and the patient tolerated the procedure well. She obtained adequate pain control with single dose of intramuscular ketorolac. She was discharged on ciprofloxacin 500 mg for 3 days. Three weeks later she presented to the hospital with anasarca as the chief concern.
At presentation, her vitals were normal with a blood pressure of 114/73 mmHg. On examination, the patient appeared well and was in no apparent distress. She had anasarca with peri-orbital edema, sacral edema, bilateral lower extremity edema, and abdominal wall distension with prominent striae. There was no abdominal fluid wave. Her lungs were clear and heart sounds were normal. Laboratory tests were significant for an albumin of 1.6 g/dL, cholesterol of 452 mg/dL, triglycerides of 345 mg/dL, and low-density lipoprotein of 292 mg/dL. Urinalysis demonstrated 6 g/d of protein with no white blood cells or red blood cells (Table 1). Serology workup, including double-stranded DNA, complement levels, anti-glomerular basement membrane antibody, antineutrophil cytoplasmic antibodies (c-ANCA, p-ANCA, and atypical ANCA), and rheumatoid factor, was negative. Serology for HIV, hepatitis B virus, and hepatitis C virus was also negative. A renal biopsy was performed, and no changes were found on light microscopy (Figure 1) or direct immunofluorescence. However, the biopsy revealed greater than 70% visceral epithelial foot process effacement with segmental microvillous transformation (Figure 2). These findings were consistent with a diagnosis of MCD.
The patient was started on 50 mg prednisone once daily, 20 mg furosemide once daily, losartan 25 mg once daily, and atorvastatin 80 mg once daily. Furosemide was discontinued 4 weeks later and steroid taper was started after 12 weeks. At 12 weeks follow-up, the patient had lost more than 31.8 kg and her urine protein had decreased to 30 mg/d from the initial 6 g/d. Anasarca, lower extremity swelling, and dyslipidemia also resolved, and the patient’s albumin improved from 1.5 to 4.1 g/dL. The patient was eventually tapered off steroids after 16 weeks and remained on losartan and statin.
Discussion
MCD accounts for 15–25% of all adult-onset nephrotic syndrome [5]. The majority of cases with MCD are idiopathic. Secondary causes include drugs (eg, nonsteroidal anti-inflammatory drugs [NSAIDs]), hematologic or solid malignancies, infections, and renal or systemic diseases [6,7]. MCD in pregnancy is especially rare, with only a few cases being reported to date. MCD associated with abortion is rarer still, with only a single case having been reported. In that case, the patient experienced a missed abortion at 8 weeks of gestation and also presented with acute renal failure. Renal biopsy showed normal histology on light microscopy with foot process effacement on electron microscopy [4].
Our patient developed symptoms after elective termination of pregnancy by dilatation and curettage at 7 weeks 3 days of gestational age. She noticed bilateral lower extremity edema 3 days after the abortion, which progressed to anasarca with periorbital and sacral edema over the next 3 weeks. Renal biopsy confirmed isolated MCD. The patient also responded well to steroids, with proteinuria decreasing from 6 g to 80 mg in 4 weeks and dropping to 30 mg at 16 weeks. This pregnancy was the patient’s fourth in 4 years. Her first pregnancy was a spontaneous abortion due to unknown cause and the next 2 pregnancies ended with normal vaginal deliveries without any complications. The patient had no similar symptoms in her previous pregnancies, with albumin of 4.3 g/dL in her third pregnancy. She had no history of proteinuria or preeclampsia. Her albumin was 3.4 g/dL at the time of abortion of her fourth pregnancy.
The pathogenesis of MCD remains unknown, but T-cell-mediated cytokine release and upregulation of proteins that disrupt the integrity of podocytes have been proposed as major contributors [8]. Disorder of T lymphocytes in a case of missed abortion was thought to have precipitated MCD in the previously reported case [4]. During pregnancy there is Th2 polarization of immunity signifying a suppression of Th1-mediated immunity contributing to maternal tolerance of the fetus. A few studies have proposed MCD to be a Th2-mediated disease [9]. Although MCD did not manifest during our patient’s previous pregnancies, surgical abortion could have led to an exaggerated immune response leading to increased proinflammatory cytokines and subsequent podocyte injury. The favorable response to steroids and immunosuppressants points to a role for the immune system in this pathogenesis [10].
Our patient received a single intramuscular dose of ketorolac for pain control. NSAIDs have been reported to cause MCD along with acute interstitial nephritis/acute tubular necrosis. A few studies have also reported isolated MCD due to NSAIDs. Fenoprofen, naproxen, and selective cyclooxygenase 2 inhibitors such as celecoxib have been implicated in the causation of nephrotic syndrome due to MCD [11,12]. It has been reasoned that NSAID-induced conversion of arachidonic acid to leukotrienes leads to activation of T cells. These activated T cells release cytokines that cause podocyte injury and increased glomerular permeability [13]. However, higher risk of nephrotic range proteinuria due to conventional NSAIDs occurs with a current use of more than 2 weeks [14]. Although our patient was given ketorolac, it was only a single intramuscular dose and renal biopsy showed no tubulointerstitial changes. Therefore, it is unlikely that MCD in our patient was due to NSAID use. NSAID-induced nephrotic syndrome has excellent remission with discontinuation of offending agent, which did not happen in our patient [15,16].
Steroids form the first line of treatment for MCD. Although there is variability in the response to steroids and the course of the disease, studies have shown up to 75–90% responsiveness at a median of 10–13 weeks [17,18]. The patient in our case report showed excellent response to steroids. Her proteinuria decreased to normal levels with 4 weeks of steroid therapy and remained in remission. Steroids were tapered down after 12 weeks.
Conclusions
The role of immunological changes in the pathogenesis of MCD needs further investigation to elucidate the factors involved, especially in pregnancy and abortion. Our patient developed symptoms and nephrotic range proteinuria after undergoing abortion, with abrupt development of hypoalbuminemia. Although there is no conclusive evidence of causation, it is imperative to be mindful of a possible relationship between abortion and MCD. Renal biopsy should be performed in patients such as ours to institute timely treatment and thereby prevent the complications of prolonged proteinuria due to this disease.
References:
1.. , ACOG Practice Bulletin No. 202: Gestational hypertension and preeclampsia: Obstet Gynecol, 2019; 133(1); 1
2.. Segarra-Medrano A, Carnicer-Caceres C, Arbos-Via MA, Biological markers of nephrotic syndrome: A few steps forward in the long way: Nefrologia, 2012; 32(5); 558-72
3.. Gonzalez Suarez ML, Kattah A, Renal disorders in pregnancy: Core curriculum 2019: Am J Kidney Dis, 2019; 73(1); 119-30
4.. Nishihara G, Nakamoto M, Yasunaga C, Minimal-change nephrotic syndrome with acute renal failure associated with missed abortion: Nephron, 1998; 80(2); 234-36
5.. Vivarelli M, Massella L, Ruggiero B, Minimal change disease: Clin J Am Soc Nephrol, 2017; 12(2); 332-45
6.. Kodner C, Diagnosis and management of nephrotic syndrome in adults: Am Fam Physician, 2016; 93(6); 479-85
7.. Trachtman H, Hogan J, Radhakrishnan J, Minimal change disease: National Kidney Foundation Primer on Kidney Diseases, 2014; 164-69, Philadelphia, W.B. Saunders
8.. Cara-Fuentes G, Clapp WL, Johnson RJ, Pathogenesis of proteinuria in idiopathic minimal change disease: Molecular mechanisms: Pediatr Nephrol, 2016; 31(12); 2179-89
9.. Pan Q, Wu J, Tao J, Role of basophils in the pathogenesis of minimal change nephrotic syndrome: A literature review: Exp Ther Med, 2014; 8(4); 1027-31
10.. Mathieson PW, Immune dysregulation in minimal change nephropathy: Nephrol Dial Transplant, 2003; 18(Suppl. 6); vi26-29
11.. Chen YH, Tarng DC, Profound urinary protein loss and acute renal failure caused by cyclooxygenase-2 inhibitor: Chin J Physiol, 2011; 54(4); 264-68
12.. Almansori M, Kovithavongs T, Qarni MU, Cyclooxygenase-2 inhibitor-associated minimal-change disease: Clin Nephrol, 2005; 63(5); 381-84
13.. Vega J, Goecke H, Mendez GP, Nephrotic syndrome and acute tubular necrosis due to meloxicam use: Ren Fail, 2012; 34(10); 1344-47
14.. Bakhriansyah M, Souverein PC, van den Hoogen MWF, Risk of nephrotic syndrome for non-steroidal anti-inflammatory drug users: Clin J Am Soc Nephrol, 2019; 14(9); 1355-62
15.. Alper AB, Meleg-Smith S, Krane NK, Nephrotic syndrome and interstitial nephritis associated with celecoxib: Am J Kidney Dis, 2002; 40(5); 1086-90
16.. Merida E, Praga M, NSAIDs and nephrotic syndrome: Clin J Am Soc Nephrol, 2019; 14(9); 1280-82
17.. Szeto CC, Lai FM, Chow KM, Long-term outcome of biopsy-proven minimal change nephropathy in Chinese adults: Am J Kidney Dis, 2015; 65(5); 710-18
18.. Canetta PA, Radhakrishnan J, The evidence-based approach to adult-onset idiopathic nephrotic syndrome: Front Pediatr, 2015; 3; 78
Figures
In Press
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250