07 May 2021: Articles 
A 41-Year-Old Woman with Excessive Fat of the Lower Body Since Puberty with Progression to Swollen Ankles and Feet Despite Caloric Restriction, Due to Lipedema and Protein-Calorie Malnutrition: A Case of Stage 3 Lipedema
Mistake in diagnosis, Educational Purpose (only if useful for a systematic review or synthesis), Rare coexistence of disease or pathology
Thomas F. Wright1ABDEF*, Karen L. Herbst23DEFDOI: 10.12659/AJCR.930306
Am J Case Rep 2021; 22:e930306
Abstract
BACKGROUND: Lipedema is a common condition that presents as excessive fat deposition in the extremities, initially sparing the trunk, ankles, and feet, and is found mainly in women, usually occurring after puberty or pregnancy. Lipedema can progress to include lipo-lymphedema of the ankles and feet. This report is of a 41-year old woman with Stage 3 lipedema and lipo-lymphedema with excessive fat of the lower body since puberty, with progression to swollen ankles and feet despite dietary caloric restriction.
CASE REPORT: A 41-year-old woman noticed increased fat in her legs since age 12. Her weight and leg size increased until age 21, when she reached a maximum weight of 165 kg, and underwent a Roux-En-Y gastric bypass. Over 12 months, she lost 74.8 kg. Her trunk significantly reduced in weight, but her legs did not. Fifteen years later, during recovery from hysterectomy surgery, she became progressively weaker and swollen over her entire body. Laboratory test results showed hypoalbuminemia (2.0 g/dL), lymphopenia, and hypolipoproteinemia. She was diagnosed with protein and calorie malnutrition with marked gut edema requiring prolonged parenteral nutrition. After restoration of normal protein, her health returned and her pitting edema resolved, but her extremities remained enlarged. She was subsequently diagnosed with lipedema.
CONCLUSIONS: This report demonstrates that early and correct diagnosis of lipedema is important, as women who believe the condition is due to obesity may suffer the consequences of calorie or protein-calorie deficiency in an attempt to lose weight.
Keywords: Body Mass Index, Kwashiorkor, lymphedema, Nutritional Physiological Phenomena, Obesity, Ankle, Caloric Restriction, Child, Edema, Lipedema, Protein-Energy Malnutrition, Puberty, young adult
Background
Lipedema is a loose connective tissue (LCT) disease characterized by disproportionate accumulation of fibrotic subcutaneous adipose tissue and extracellular fluid in the limbs of women due to microvascular inflammation [1]. Lipedema is poorly recognized and it is often confused with lifestyle-induced obesity [2]. Often, women with lipedema are instructed to reduce caloric intake or increase exercise, neither of which substantially affects lipedema. Lipedema is also often confused with lymphedema, which causes asymmetric swelling of the limbs and is caused by defects in lymphatic transport [3] (Table 1). The diagnosis of lipedema is based on the clinical criteria first published by Wold and updated most recently with International Consensus Diagnostic Criteria [4,5] (Table 2). These criteria emphasize heavy, tender, symmetric enlargement of the limbs, sparing the hands and feet, with negative Kaposi-Stemmer’s Sign. The prevalence of lipedema is not known; however, the most cited estimate of prevalence is 11% of the female population [6]. Lipedema is classified as a diffuse painful symmetric lipomatosis and needs to be differentiated from another lipomatosis disease, called Dercum’s disease, which is characterized by painful lipomas [7].
Lipedema progression is graded by stages [3,5,8]. Stage 1 lipedema is characterized by a thickening and disproportionate accumulation of loose connective tissue in the extremities. The skin remains smooth, but there are small palpable nodules in the LCT; the tissue is generally not heavy or swollen, but there may be pain, and there is resistance to weight loss by diet or exercise. Stage 2 lipedema is characterized by increased fibrous tissue leading to larger palpable nodules in the LCT and increased swelling and tenderness of affected areas. Stage 3 lipedema is characterized by formation of lobules of skin and LCT, and larger and more extensive masses in the tissue [8]. Increased tissue sodium and extracellular water are seen in Stage 2 and 3 lipedema [9,10]. Delayed lymphatic transport in lipedema may be present before overt clinical secondary lymphedema or lipo-lymphedema is seen [11,12]. A percentage of women in Stage 3 lipedema develop overt secondary lymphedema with pitting edema in the legs and feet, called lipo-lymphedema [13].
Body mass index (BMI) is commonly used to aid in the diagnosis of diseases. BMI less than 18.5 kg/m2 is associated with malnutrition. Obesity is often defined as BMI at or above 30 kg/m2 [14]. Lipedema is often associated with an increased BMI and confused with non-lipedema obesity [2]. However, non-lipedema obesity is often more centrally located, especially around the abdomen or android area, resulting in metabolic disease such as type 2 diabetes mellitus (DM2), whereas lipedema is disproportionately located below the waist and also on the arms in gynoid areas, and this pattern is usually cardio-protective [15]. Therefore, defining obesity by increased BMI alone can be inaccurate because it describes two very different adipose tissue diseases. This clinical case illustrates that solely using BMI to describe obesity can lead to misleading or inaccurate conclusions. This report is of a 41-year old woman with Stage 3 lipedema and lipo-lymphedema with excessive fat of the lower body since puberty, with progression to swollen ankles and feet despite dietary caloric restriction.
Case Report
CLINICAL COURSE:
The patient was diagnosed with severe protein-calorie malnutrition, anasarca, and Stage 3, Type 3 (waist to ankle), and type 4 (arms affected) lipedema. The hypoalbuminemia caused not only pitting edema of her face, trunk, and extremities, but also gut edema, so that the patient was unable to absorb nutrition properly from her gastrointestinal tract. She was started on parenteral nutrition. As her nutritional state and her serum protein levels improved, her pitting edema resolved and she lost 29.5 kg. Her Kaposi-Stemmers sign reverted to negative in her hands and feet, consistent with lipedema without clinically significant secondary lymphedema. However, mild non-pitting edema in her extremities persisted, which is consistent with lipedema in Stages 2 and 3 of the disease. After several weeks of parenteral nutrition, she was started on enteral and then oral nutrition. Her microcytic iron deficiency anemia, vitamin D deficiency, lymphopenia, and hyperlipoproteinemia all resolved with supplementation and resolution of her gut edema. After stabilization in an acute care setting, she was transferred to a rehabilitation unit to recover her strength and mobility (Figure 1A, 1B).
Discussion
This clinical case sheds some insight into the loose connective tissue disease of lipedema, which is dominated by adipose tissue that can persist in the face of severe protein-calorie malnutrition, and how persistent lipedema tissue can delay a diagnosis of malnutrition. The case also illustrates how edema in lipedema can be multifactorial and switch between nonpitting edema, with no involvement of the feet and hands, to pitting edema, with involvement of the feet and hands. The presence of orthostatic or dependent edema, which usually spares the feet, has been considered a sign of the disease since it was first described by Allen and Hines, but it remains poorly understood [16]. Clinically, on exam, one can appreciate weighty subcutaneous tissue with non-pitting edema in the dependent extremities in women with stage 2 and 3 lipedema. Crescenzi et al showed that there is increased tissue sodium in the lower extremities of women with lipedema on magnetic resonance imaging (MRI), suggesting an increase in glycosaminoglycans, which bind sodium but also water [9]. This increased sodium in the lower extremity skin is present even when there is no free fluid seen in the lower extremities on MRI [9]. This may be one reason why patients with lipedema often have non-pitting edema (the water/fluid is bound to glycosaminoglycans) instead of pitting edema (characterized by increased unbound water/fluid). Increased extracellular water has been shown to be present in the lower extremities, compared with the upper extremities, of women with higher stages of lipedema: Stages 2 and 3 when measured by bioimpedance spectroscopy [10]. Delayed lymphatic transport is also found by lymphangioscintigraphy in patients with lipedema before the overt appearance of clinical secondary lymphedema or lipo-lymphedema [11]. In the case presented here, nonpitting edema was present in the subcutaneous adipose tissue of the lower extremities. This non-pitting edema spared the feet when the patient was in a good nutritional state of health with normal protein levels. This is consistent with the above clinical scientific observations of lipedema. During her state of protein-calorie malnutrition, her feet and hands developed pitting edema, which is also seen in advanced stage 3 lipedema and which is often described clinically as secondary lymphedema and or lipo-lymphedema. In the case presented here, we believe her lymphedema was secondary to her hypoalbuminemia because her lymphoscintigram was interpreted as showing delayed transport but was otherwise normal.
This case illustrates an individual who simultaneously had protein-calorie malnutrition and a BMI over 30 kg/m2, consistent with obesity. Her increased BMI was largely due to lipedema tissue in the extremities, as her trunk was clearly not obese. Obesity is defined by the World Health Organization [WHO] as abnormal or excessive fat accumulation that presents a risk to health. The WHO further defines a BMI over 25 kg/m2 as over-weight, and BMI over 30 kg/m2 as obese [14]. The distribution of the patient’s excess fat accumulation was not centrally located but was distributed on her hips, arms, and legs. This distribution of fat is not associated with metabolic disease, including cardiovascular disease, hypertension, and diabetes [15]. A better definition of obesity is the Obesity Medicine Association’s definition: a chronic, relapsing, multifactorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences [17]. Lipedema tissue contains hypertrophic adipocytes, similar to non-lipedema obesity, and is associated with lymphedema, similar to non-lipedema obesity [7]. However, the disproportionate fat accumulation in lipedema that confers unique mobility issues is generally not associated with other metabolic effects until later stages [15]. This case shows a woman who, despite her elevated BMI, had hypolipoproteinemia, low-to-normal blood sugar, and other metabolic measures which are considered cardioprotective and not associated with the metabolic changes seen in obesity. BMI is a score and is not an objective measurement of disease-associated fat mass or, more precisely, fat mass-related mechanical and metabolic disturbances. BMI can be elevated by increased nonfat mass such as fluid weight, as seen in this case, or increased muscle mass. In summary, a BMI score, just like the height and weight measurements from which it is derived, is not a biologically representative measure. This case demonstrates how BMI ranges used by the WHO for diagnosis of over-weight and obesity can be misleading or biologically wrong, as in this case of a patient with lipedema [18]. Awareness of lipedema among healthcare professionals is poor, and individuals with lipedema are often told they can be treated with caloric restriction, as occurred in this case [19].
The patient’s lymphorrhea and body swelling were secondary to hypoproteinemia and not due to liver, kidney, or heart disease, or even lymphedema. The edema and lymphorrhea resolved after the patient’s protein level returned to normal. The patient’s lymphoscintigram also did not show evidence of lymphedema, although the clearance of radiotracer was slightly delayed. The slight delay in clearance could have been secondary to hypoalbuminemia or inflammation inhibiting lymphatic vessel pumping [20]. Lipedema is often associated with delayed clearance of radiotracer in lymphangioscintigraphy studies [11,12] and can cause secondary lymphedema, but did not in this case.
Lipedema is characterized by onset and worsening during periods of hormonal changes such as puberty, as occurred in this case [5,8]. The patient’s history of worsening of symptoms after her total hysterectomy is also noteworthy. Development or worsening of lipedema is often associated with hormonal changes such as hysterectomy with removal of the ovaries [8]. The patient had a steady weight until her total hysterectomy resulted in worsening of her edema. The nutritional stress of recovering from surgery may also have precipitated protein malnutrition, which can result in gut edema.
Conclusions
This case report demonstrates that an early and correct diagnosis of lipedema is important, as women who believe the condition is due to obesity may suffer the consequences of calorie or protein-calorie deficiency in an attempt to lose weight. This case also illustrates that lipedema can persist even in the face of severe protein and calorie malnutrition and that BMI can be an inaccurate guide for the diagnosis of lipedema, malnutrition, and obesity.
References:
1.. AL-Ghadban S, Cromer W, Allen M, Dilated blood and lymphatic microvessels, angiogenesis, increased macrophages, and adipocyte hypertrophy in lipedema thigh skin and fat tissue: J Obesity, 2019; 2019; 8747461
2.. Herbst KL, Rare adipose disorders (RADs) masquerading as obesity: Acta Pharmacol Sin, 2012; 33(2); 155-72
3.. Buck DW, Herbst KL, Lipedema: A relatively common disease with extremely common misconceptions: Plast Reconstr Surg Glob Open, 2016; 4(9); e1043
4.. Wold LE, Hines EA, Allen EV, Lipedema of the legs; a syndrome characterized by fat legs and edema: Ann Intern Med, 1951; 34; 1243-50
5.. Sandhofer M, Habbema L, Herbst K, Prevention of progression of lipedema with liposuction using tumescent local anesthesia: Results of an International Consensus Conference: Dermatol Surg, 2020; 46(2); 220-28
6.. Foldi E, Lipedema: Foldi’s Textbook of Lymphology, 2006; 417-27, Munich, Germany, Elsevier GmbH
7.. Beltran K, Herbst KL, Differentiating lipedema and Dercum’s disease: Int J Obes (Lond), 2017; 41(2); 240-45
8.. Wollina U, Lipedema – an update: Dermatol Ther, 2019; 32(2); e12805
9.. Crescenzi R, Marton A, Donahue PMC, Tissue sodium content is elevated in the skin and subcutaneous adipose tissue in women with lipedema: Obesity (Silver Spring), 2018; 26(2); 310-17
10.. Crescenzi R, Donahue PMC, Weakley S, Lipedema and Dercum’s disease: A new application of bioimpedance: Lymphat Res Biol, 2019; 17(6); 671-79
11.. Forner-Cordero I, Olivan-Sasot P, Ruiz-Llorca C, Lymphoscintigraphic findings in patients with lipedema: Rev Esp Med Nucl Imagen Mol, 2018; 37(6); 341-48
12.. Gould DJ, El-Sabawi B, Colletti PM, Abstract: Uncovering lymphatic transport abnormalities in patients with lipedema: Plast Reconstr Surg Glob Open, 2017; 5(9 Suppl.); 215
13.. Herbst K, Mirkovskaya L, Bharhagava A, Lipedema fat and signs and symptoms of illness, increase with advancing stage: Arch Med, 2015; 7; 4-10
14.. : Obesity: Preventing and managing the global epidemic: Report of a WHO consultation, 2000, World Health Organization
15.. Torre YS, Wadeea R, Rosas V, Lipedema: Friend and foe: Horm Mol Biol Clin Investig, 2018; 33(1) /j/hmbci.201833.issue-1/hmbci-2017-0076/hmbci-2017-0076.xml
16.. Wold LE, Hines EA, Allen EV, Lipedema of the legs; A syndrome characterized by fat legs and edema: Ann Intern Med, 1951; 34(5); 1243-50
17.. Felmerer G, Stylianaki A, Hägerling R, Adipose tissue hypertrophy, an aberrant biochemical profile and distinct gene expression in lipedema: J Surg Res, 2020; 253; 294-303
18.. Müller MJ, Braun W, Enderle J, Beyond BMI: Conceptual issues related to overweight and obese patients: Obes Facts, 2016; 9(3); 193-205
19.. Fetzer A, Fetzer S, Early lipoedema diagnosis and the RCGP e-learning course: Br J Community Nurs, 2015(Suppl.S22); S24-28
20.. Schwager S, Detmar M, Inflammation and lymphatic function: Front Immunol, 2019; 10; 308
Tables
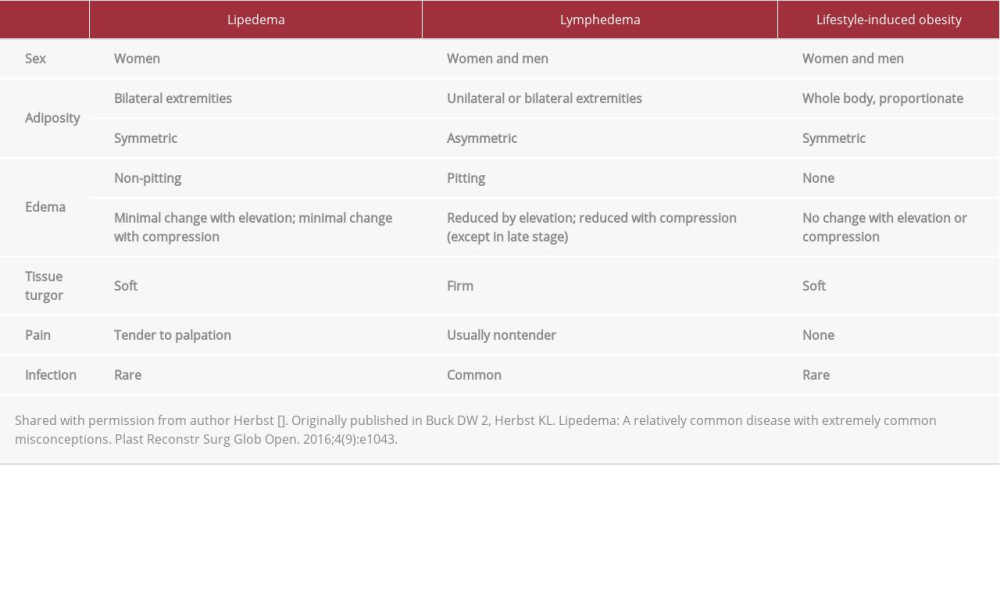 Table 1.. Comparison of findings in lipedema, lymphedema, and lifestyle-induced obesity.
Table 1.. Comparison of findings in lipedema, lymphedema, and lifestyle-induced obesity.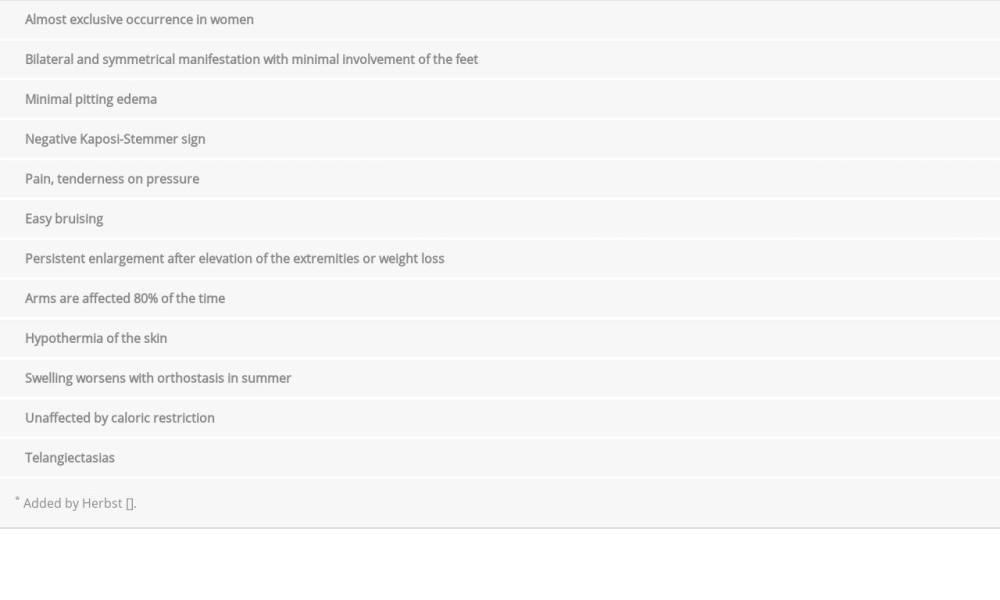 Table 2.. Diagnostic criteria for lipedema.
Table 2.. Diagnostic criteria for lipedema.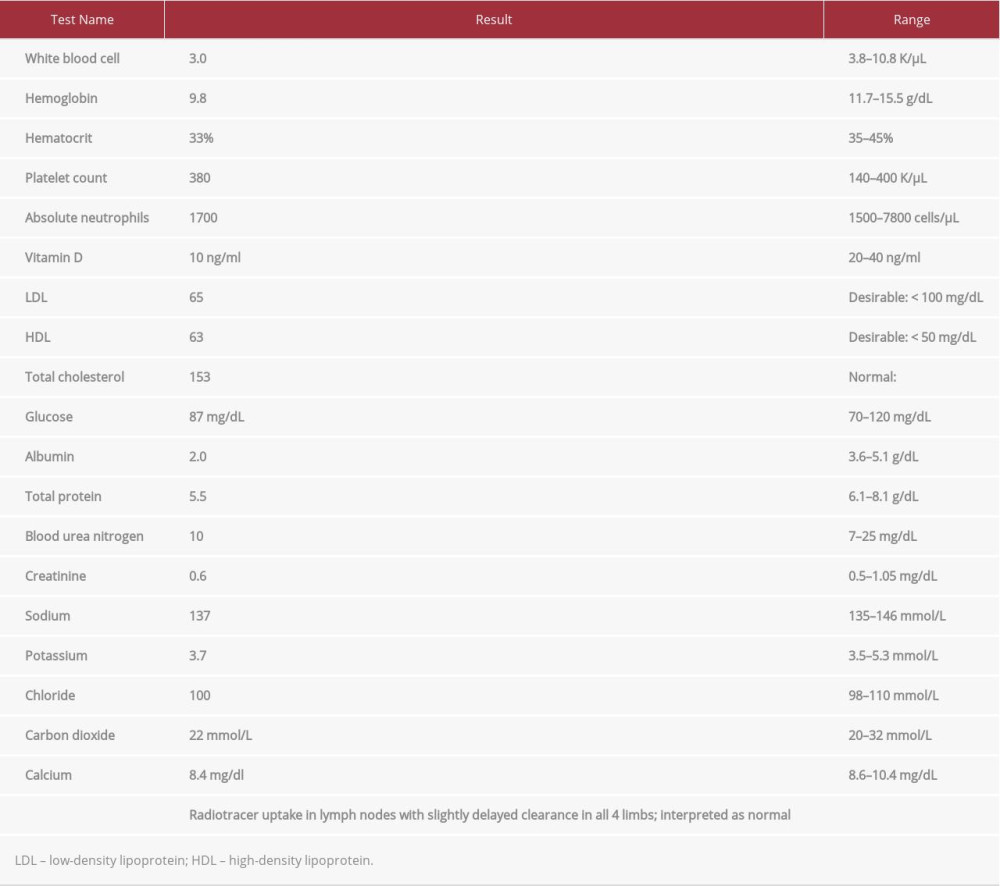 Table 3.. Laboratory test results.
Table 3.. Laboratory test results.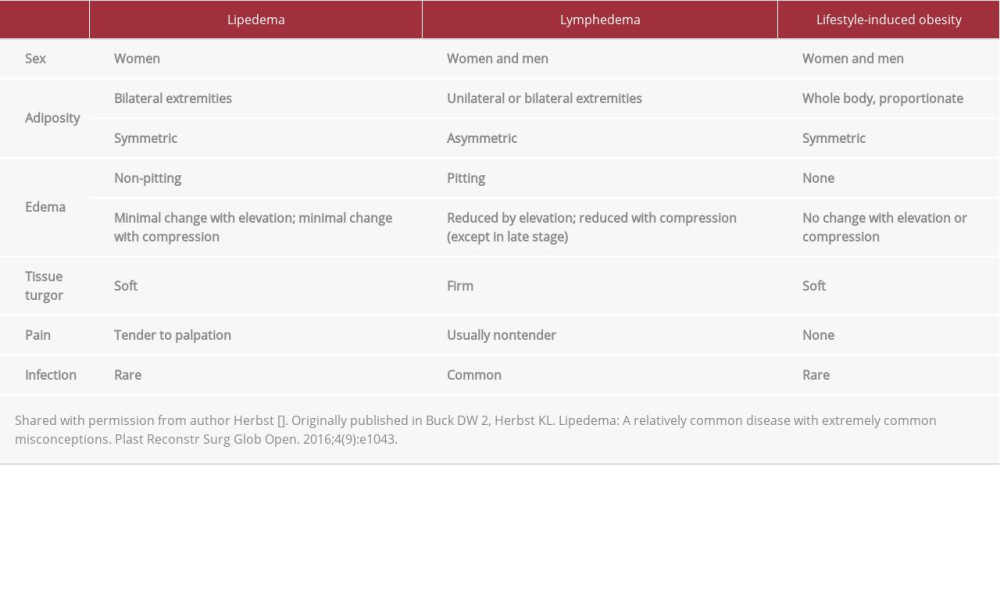 Table 1.. Comparison of findings in lipedema, lymphedema, and lifestyle-induced obesity.
Table 1.. Comparison of findings in lipedema, lymphedema, and lifestyle-induced obesity.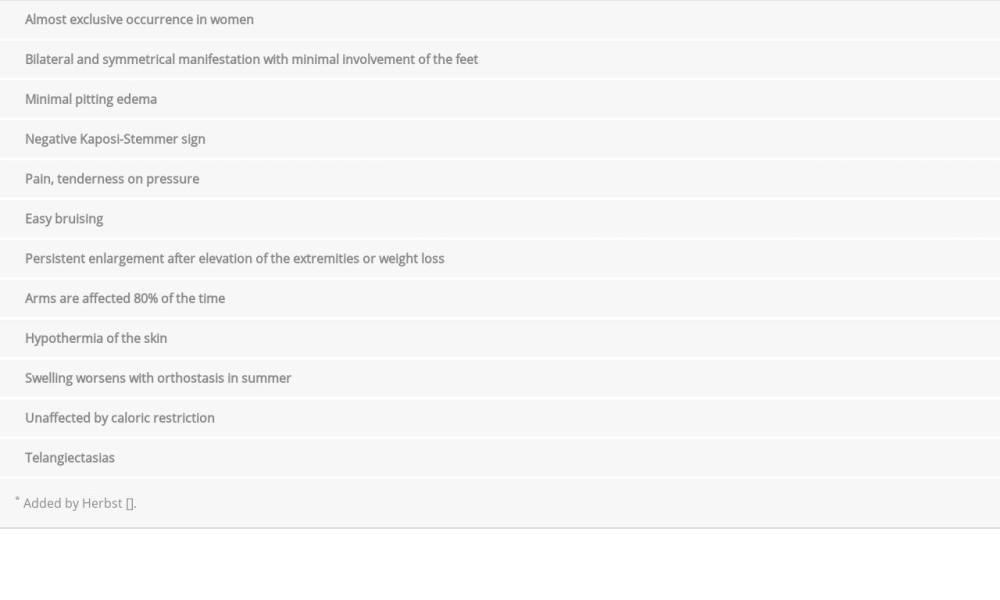 Table 2.. Diagnostic criteria for lipedema.
Table 2.. Diagnostic criteria for lipedema.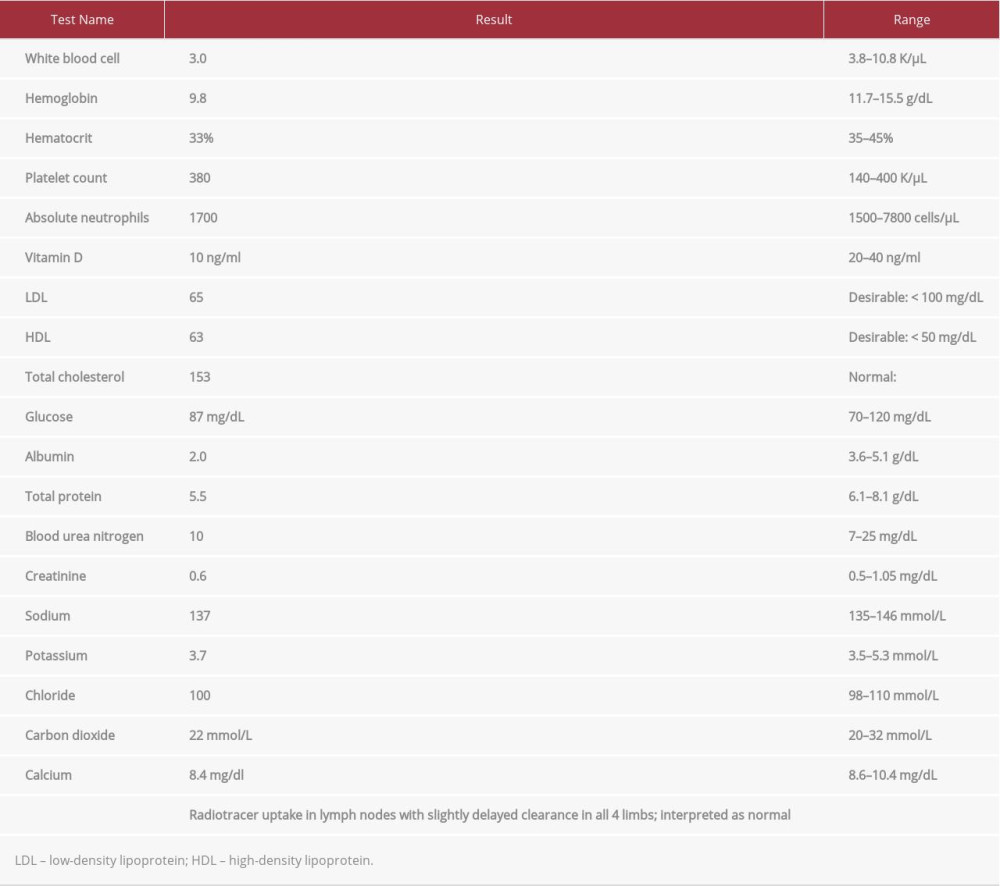 Table 3.. Laboratory test results.
Table 3.. Laboratory test results. In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








