17 June 2021: Articles 
SARS-CoV-2-Related Subacute Thyroiditis, Myocarditis, and Hepatitis After Full Resolution of COVID-19 Serum Markers
Unusual clinical course
Alejandra Osorio Martínez1BEF, Victoria Taís González-Razo1BEF, Valeria Navarro-Sánchez1BEF, Carlos A. Souto Meiriño2CD, Miguel Ahumada-Ayala13BDEF*DOI: 10.12659/AJCR.932321
Am J Case Rep 2021; 22:e932321
Abstract
BACKGROUND: Subacute thyroiditis, myocarditis, and hepatitis are inflammatory disorders that may develop after viral infections, including SARS-CoV-2. These entities may appear after resolution of the respiratory syndrome.
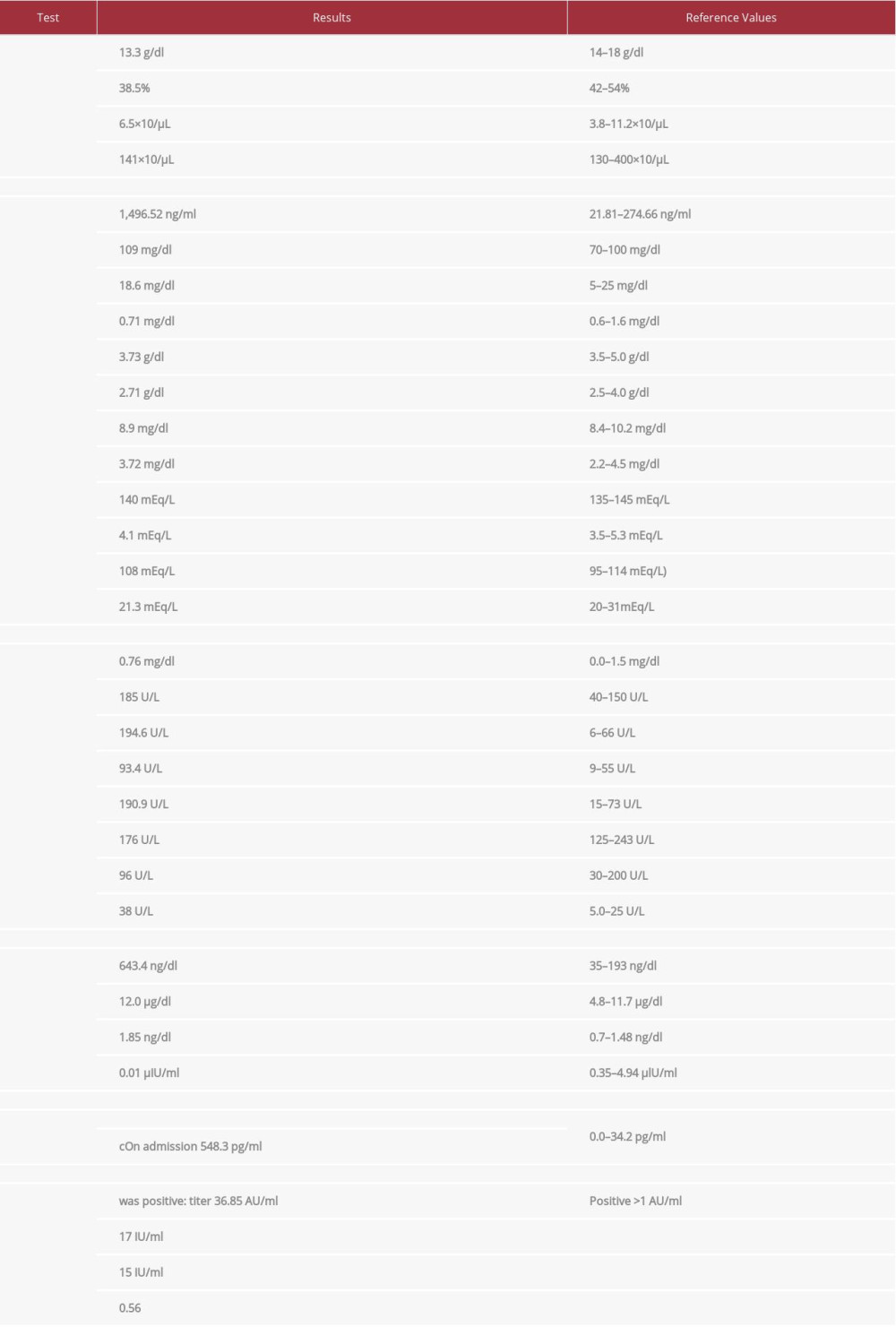
CASE REPORT: A previously healthy 64-year-old male patient came to the hospital reporting severe chest pain. He had a history of a COVID-19 pneumonia with PCR confirmation 4 weeks before. On admission to the Coronary Care Unit (CCU), the patient had a negative PCR for SARS-CoV-2; the following tests were performed: total T3 643.4 ng/dl (reference 35-193 ng/dl), total thyroxine 12.0 μg/dl (reference 4.8-11.7 μg/dl), free T4 1.85 ng/dl (reference 0.7-1.48 ng/dl), TSH 0.01 μIU/ml (reference 0.35-4.94 μIU/ml); total bilirubin 0.76 mg/dl (reference 0.0-1.5 mg/dl), alkaline phosphatase 185 U/L (reference 40-150 U/L), alanine aminotransferase 194.6 U/L (reference 6-66 U/L), aspartate aminotransferase 93.4 U/L (reference 9-55 U/L); on admission to the CCU high-sensitivity troponin I 548.3 pg/ml (reference 0.0-34.2 pg/ml), after 24 h in the CCU 801 pg/ml, and after 11 days (as an outpatient) 4.5 pg/ml. A thyroid gammagram revealed absent uptake of the radionuclide. Normal cardiac gammagraphy and cardiac enzymes ruled out myocardial ischemia and infarction. The following diagnoses were made: myocarditis, subacute thyroiditis, and reactive hepatitis due to SARS-CoV-2 infection.
CONCLUSIONS: COVID-19 has been demonstrated to be a multisystemic inflammatory disorder. The serious illness that developed in our patient after relief of his pulmonary disease underlines this nature. We suggest close follow-up of patients even after apparent clinical resolution, and performing thyroid, myocardial, and liver tests if clinically indicated.
Keywords: COVID-19, Hepatitis, myocarditis, severe acute respiratory syndrome coronavirus 2, Thyroiditis, Subacute, COVID-19, SARS-CoV-2
Background
Subacute thyroiditis (SAT) is a self-limited inflammatory disorder of the thyroid gland, more common in females; it develops after a viral infection, such as adenovirus, coxsackievirus, influenza, herpes virus (Epstein-Barr and cytomegalovirus), measles, parvovirus B19, and rubella, among others [1]. SAT is characterized by 3 stages: 1) thyrotoxicosis, lasting typically 2–3 weeks; 2) transient hypothyroidism (may be permanent); 3) recovery period, when the patient becomes euthyroid (usually after 4–6 weeks) [1]. Myocarditis is more common in men, and it has a wide range of clinical presentations, which include fatigue, chest pain, palpitations, cardiogenic shock, and even sudden cardiac arrest; it is also known for a viral prodrome with non-specific symptoms [2–4]. Liver injury is the most frequent complication of SARS-CoV-2 infection outside the respiratory system. The most common hepatic injury is acute hepatitis, which can be diagnosed by high levels of aspar-tate aminotransferase (AST), alanine aminotransferase (ALT), and total bilirubin. Other types of liver injury include steatosis, portal inflammation, granulomas, thrombotic bodies, and biliary pathology [5–8].
Case Report
We report the case of a previously healthy 64-year-old man, a resident of Mexico City, who arrived at the hospital reporting he had oppressive chest pain. His illness apparently began 1 month before, when he attended a dinner party with a group of family and friends, of which 12 out of 15 people attending were later diagnosed with COVID-19. Four days after the party, our patient developed high fever, productive cough, headache, and extreme fatigue. A PCR for SARS-CoV-2 virus was performed; it came back positive for viral genes N, E, and RdRp. Consequently, a chest computed tomography (CT) scan was performed, which revealed a multifocal pneumonia with ground-glass opacities compatible with a SARS-CoV-2 infection. Our patient was treated with oral steroids, azithromycin, and acetaminophen, with a full recovery after 2 weeks of treatment. Three weeks after the first positive PCR test for COVID-19, he developed severe oppressive chest pain, which persisted after taking analgesic drugs; for this reason, he was admitted to the hospital.
On admission to the CCU his vital signs were as follows: blood pressure 140/80 mmHg, heart rate (HR) 120 beats per minute (bpm), temperature 36.8°C. A physical examination revealed a slight distal tremor with evident generalized diaphoresis without any other abnormalities; the thyroid gland could not be palpated. Table 1 summarizes all blood tests, obtained results, and their respective reference values. Thyroid ultrasound showed a diffusely enlarged micronodular thyroid gland (Figure 1), thyroid gammagram-single photon emission tomography (SPECT): absent radionuclide uptake (Tc99m/Pertechnetate); EKG on arrival to the emergency room showed sinus tachycardia, HR 120 bpm; no ST-T wave abnormalities were observed nor any other abnormalities. On transthoracic echocardiogram, left ventricle cavity size and wall motion and thickness were normal, with ejection fraction 56%; 24-h Holter monitoring (taking atenolol 50 mg twice daily) showed an average HR of 76 bpm with no significant arrhythmias. On SPECT imaging of myocardial perfusion and function, no evidence of ischemia or infarction was found; systolic function was normal.
After these examinations and analyses, the following diagnoses were made: myocarditis, subacute thyroiditis, and reactive hepatitis after SARS-CoV-2 infection. Patient was treated with beta-blocking agents (atenolol 50 mg twice daily) and prednisone 50 mg with gradual dosage tapering over the course of 2 weeks. Three days after admission, the patient was discharged with full clinical relief. On his last outpatient visit to the endocrine clinic, he had discontinued steroids. His thyroid tests revealed a slight primary hypothyroidism, which was treated with 100 μg of levothyroxine. The patient is currently asymptomatic and without any other sequelae.
Discussion
Since the beginning of the SARS-CoV-2 pandemic in December 2019, the pathophysiology of this disease has been demonstrated to evolve to a systemic hyperinflammatory state which can involve almost any organ. Tissues expressing angiotensin-converting enzyme 2 (ACE-2) protein appear to be more susceptible, including the lungs, heart, and liver. Thyroid follicular tissue also expresses ACE-2 and is therefore susceptible to SARS-CoV-2 inflammatory destruction [9,10]. SARS-CoV-2 uses a Spike protein to attach itself to ACE-2. More recently, ACE-2 mRNA was also detected in thyroid tissue [9]. The first case of COVID-19-related subacute thyroiditis was reported in April 2020 in Italy [11]. The authors described a noticeable elevation of inflammatory markers such as C-reactive protein (CRP), as well as an increase in T4 and T3, accompanied with low levels of TSH and a thyroid ultrasound with bilateral diffuse hypoechoic and variable vascularity. Several COVID-19-related SAT cases have been reported since from all over the world [2–8,10,12–17].
In this case, clinical and imaging features were compatible with SAT. Simultaneously, the patient developed myocarditis without evidence of ischemia, and reactive hepatitis. Myocarditis was responsible for the patient’s chest pain; both ischemic heart disease and pericarditis were ruled out by diagnostic tests indicating normal myocardial perfusion and no echocardiogram alterations suggestive of pericarditis. Even throughout the patient’s hospital stay, 2 echocardiograms indicated normal diastolic function. In light of the patient’s tachycardia on admission, after making sure the patient had no contraindications with normal echocardiogram, beta-blocking agents were administered. Once acute myocarditis was suspected, cardiac magnetic resonance imaging (MRI) was not performed in view of satisfactory clinical resolution of chest pain 24 h after admission, normal echocardiogram, and 24-h Holter monitoring with no rhythm alterations, with appropriate clinical response to the beta-blocking agent. At our institution, thyroid function tests are recommended for all seriously ill patients with tachycardia with no apparent cause. Severe chest pain dominated the clinical picture. The patient was examined in supine position at the CCU, which could have made palpation of the thyroid gland difficult. Moreover, we believe the neck pain could have been masked by the severe chest pain our patient was suffering.
Ashar et al described the following manifestations in patients with COVID-19 and myocarditis: fever, cough, myalgia, fatigue, expectoration, and dyspnea [9]. Myocarditis may be identified with a cardiac MRI showing myocardial edema, elevated inflammatory markers (IL-6, CRP, and procalcitonin), and elevated levels of serum high-sensitivity troponin I [9]. Several COVID-19-related myocarditis cases have been reported from all over the world, which have been treated with corticosteroids and IL-6 inhibitors [2–4]. As for liver complications, although the pathophysiology underlying liver damage is not yet clear, ACE-2 is also expressed in liver cells and the bile duct. Liver injuries associated with COVID-19 have been transient and reversible, with no need for special treatment. Several COVID-19 related hepatitis cases have been reported from all over the world as well [5–8].
Aemaz Ur Rehman et al recently described demographics, clinical features, imaging, and laboratory findings in COVID-19-related subacute thyroiditis case reports, all compiled in a systematic review [18]. The median age reported was 40.0±11.3 years, ranging from 18 to 69 years; over three-quarters of cases were female patients, with only 6 case reports being male. Out of 21 patients, 17 presented fever and neck pain; thyroid function tests most commonly had low TSH and high T3 or T4, or both, with 100% of case reports having ultrasound changes suggesting subacute thyroiditis [18].
The age range, thyroid function tests, and image findings in our case matched those reported in the systematic review [18]. Although the literature reports subacute thyroiditis is more common among women [18], it is not exclusively a disease of women, as evidenced by our case and supported by 6 other case reports of male patient [18]. In addition, even though fever and neck pain are the most common clinical features of SAT, 4 out of 21 cases aside from ours did not present fever or neck pain either [18]. In 3 cases, the presenting symptom was tachycardia, while fatigue and palpitations were among the most commonly reported symptoms in other case reports [18]. Based on these findings, we believe that our patient’s clinical features help to illustrate the clinical variability of SARS-CoV-2-related subacute thyroiditis.
SAT, myocarditis, and hepatitis were clinically evident once respiratory manifestations were resolved and PCR tests for SARSCoV-2 were negative. Although thyroid function tests, high-sensitivity troponin I, and liver function tests are not always necessary in patients with COVID-19, these potential complications have to be kept in mind as they may aggravate the clinical course, even in apparently resolved cases when SARSCoV-2 infection is no longer ongoing [18]. To the best of our knowledge, only a single case of subacute thyroiditis has been previously reported in Mexico [18], while most reported cases have been described in Italy and Iran [18]. Therefore, we agree with Aemaz Ur Rehman et al’s emphasis on assessing SAT in patients with a history of SARS-CoV-2 infection [18], since it is possible that SAT cases are being overlooked.
A short course of treatment with steroids promptly relieved our patient’s clinical manifestations and allowed rapid discharge from the hospital. Other COVID-19-related subacute thyroiditis cases have also had satisfactory clinical outcomes when treated with steroids and anti-inflammatory drugs [18]. Since myocarditis and hepatitis are also inflammatory disorders, they usually respond simultaneously to anti-inflammatory and supportive measures [19].
Conclusions
Subacute thyroiditis, myocarditis, and hepatitis must be considered as 3 easily overlooked and serious potential complications in patients with severe COVID-19. Subacute thyroiditis must be suspected in patients with COVID-19 history who present clinical features of hyperthyroidism, such as tachycardia, tremor, or diaphoresis, with no apparent cause. The diagnosis is easily confirmed by absent radionuclide uptake in thyroid gammagram and ultrasound features including a diffusely enlarged gland. Although neck pain is typical in SAT, SARS-CoV-2-induced SAT does not always present itself with neck pain, as shown in this case, among others. Measurement of serum high-sensitivity troponin I is helpful to identify involvement of the myocardium, and elevated aminotransferases suggest liver injury, such as hepatitis. Treatment with a short course of steroids may be considered in many of these cases.
References:
1.. Chong WH, Shkolnik B, Saha B, Beegle S, Subacute thyroiditis in the setting of coronavirus disease 2019: Am J Med Sci, 2021; 361(3); 400-2
2.. Pirzada A, Mokhtar AT, Moeller AD, COVID-19 and myocarditis: What do we know so far?: CJC Open, 2020; 2(4); 278-85
3.. Cao J, Zheng Y, Luo Z, Mei Z, Myocardial injury and COVID-19: Serum hs-cTnI level in risk stratification and the prediction of 30-day fatality in COVID-19 patients with no prior cardiovascular disease: Theranostics, 2020; 10(21); 9663-73
4.. Inciardi RM, Lupi L, Zaccone G, Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19): JAMA Cardiol, 2020; 5(7); 819-24
5.. Yang R-X, Zheng R-D, Fan J-G, Etiology and management of liver injury in patients with COVID-19: World J Gastroenterol, 2020; 26(32); 4753-62
6.. Papadopoulosa N, Vasileiadib S, Deutschb M, COVID-19 and liver injury: Where do we stand?: Ann Gastroenterol, 2020; 33(5); 459-64
7.. Samidoust P, Samidoust A, Samadani AA, Khoshdoz S, Risk of hepatic failure in COVID-19 patients. A systematic review and meta-analysis: Infez Med, 2020; 28(Suppl. 1); 96-103
8.. Lagana SM, Kudose S, Iuga AC, Hepatic pathology in patients dying of COVID-19: A series of 40 cases including clinical, histologic, and virologic data: Mod Pathol, 2020; 33(11); 2147-55
9.. Rotondi M, Coperchini F, Ricci G, Detection of SARS-COV-2 receptor ACE-2 mRNA in thyroid cells: A clue for COVID-19-related subacute thyroiditis: J Endocrinol Invest, 2021; 44(5); 1085-90
10.. Chakraborty U, Ghosh S, Chandra A, Ray AK, Subacute thyroiditis as a presenting manifestation of COVID-19: A report of an exceedingly rare clinical entity: BMJ Case Rep, 2020; 13(12); e239953
11.. Brancatella A, Ricci D, Viola N, Sgrò D, Subacute thyroiditis after SarsCov-2 infection: J Clin Endocrinol Metab, 2020; 105(7); dgaa276
12.. Gorini F, Bianchi F, Iervasi G, COVID-19 and thyroid: Progress and prospects: Int J Environ Res Public Health, 2020; 17(18); 6630
13.. Ippolito S, Dentali F, Tanda ML, SARS-CoV-2: A potential trigger for subacute thyroiditis? Insights from a case report: J Endocrinol Invest, 2020; 43(8); 1171-72
14.. Asfuroglu Kalkan E, Ates I, A case of subacute thyroiditis associated with Covid-19 infection: J Endocrinol Invest, 2020; 43(8); 1173-74
15.. Ruggeri RM, Campennì A, Siracusa M, Subacute thyroiditis in a patient infected with SARS-COV-2: An endocrine complication linked to the COVID-19 pandemic: Hormones (Athens), 2021; 20(1); 219-21
16.. Mattar SAM, Koh SJQ, Rama Chandran S, Cherng BPZ, Subacute thyroiditis associated with COVID-19: BMJ Case Rep, 2020; 13(8); e237336
17.. Campos-Barrera E, Alvarez-Cisneros T, Davalos-Fuentes M, Subacute thyroiditis associated with COVID-19: Case Rep Endocrinol, 2020; 2020; 8891539
18.. Aemaz Ur, Rehman M, Farooq H, Ali MM, The association of subacute thyroiditis with COVID-19: A systematic review: SN Compr Clin Med, 2021 [Online ahead of print]
19.. Bril F, Al Diffalha S, Dean M, Fettig DM, Autoimmune hepatitis developing after coronavirus disease 2019 (COVID-19) vaccine: Causality or casualty?: J Hepatol, 2021 [Online ahead of print]
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943214
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943010
16 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943687
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250