09 August 2021: Articles 
Autopsy Case of Pfeiffer Syndrome Type 2, a Phenotype of Fibroblast Growth Factor Receptor-Associated Craniosynostosis Syndromes, with Tracheal Cartilage Sleeve and Abnormal Hyperplasia of Bronchial Cartilages
Rare disease
Shin-ya Katsuragi1ABCDEF, Etsuko Hirose2ABCDEF, Yoshifumi Arai1ABCDEF, Yoshiro Otsuki1CDEF*, Shigeru Ohki2BCDE, Hiroshi Kobayashi13ACDEFDOI: 10.12659/AJCR.932450
Am J Case Rep 2021; 22:e932450
Abstract
BACKGROUND: Pfeiffer syndrome (PS) is a fibroblast growth factor receptor (FGFR)-associated craniosynostosis syndrome, characterized by abnormally broad and medially deviated thumbs and great toes. Tracheal cartilage sleeve (TCS) is associated with several FGFR-associated craniosynostosis syndromes, including PS. TCS is an airway malformation in which the tracheal cartilage rings fuse with each other to form a sleeve of cartilage.
CASE REPORT: The patient was a 4-year-old girl with PS, TCS, and abnormal hyperplasia of non-fused intrapulmonary cartilages. The patient showed cranial dysplasia on prenatal ultrasonography. At birth, a cloverleaf skull in association with hydrocephalus and digital malformations was apparent. These findings were consistent with PS type 2. The diagnosis of PS type 2 was confirmed from a genetic test detecting a FGFR2 mutation (Y340C). During the clinical course, she underwent several surgeries, including ventriculoperitoneal shunts, sequential cranioplasty surgeries, and tracheotomy due to upper airway abnormalities. At 4 years old, she died of multiple organ failure following aspiration pneumonia. The autopsy revealed that the tracheal cartilages had fused with each other, resulting in a condition called TCS, in which the cartilage rings and tracheal ligaments were absent. The lungs were poorly aerated, and the dilated bronchi had thickened walls surrounded by many cartilage fragments, mainly at the hilum. These cartilages tended to overlap at both ends, did not fuse, and were greatly altered in size and shape.
CONCLUSIONS: We report the results of autopsy for PS with the first histopathological findings for the lungs and other visceral organs.
Keywords: Acrocephalosyndactylia, Craniosynostoses, Fibroblast Growth Factor 2, tracheal stenosis, Autopsy, Bronchi, Cartilage, Child, Preschool, Hyperplasia, Infant, Newborn, Phenotype, Pregnancy, Receptor, Fibroblast Growth Factor, Type 2, Syndrome
Background
Pfeiffer syndrome (PS) is a disorder of syndromatic craniosynostosis or a craniosynostosis syndrome, representing a hereditary form of craniosynostosis, associated with extracranial abnormalities [1]. Pfeiffer provided the first reports of PS cases in 1964 [2], and Cohen proposed 3 subclassifications based on differences in skull shape and the form of heredity [3]. Schell subsequently reported mutations in fibroblast growth factor receptor
Case Report
CLINICAL SUMMARY:
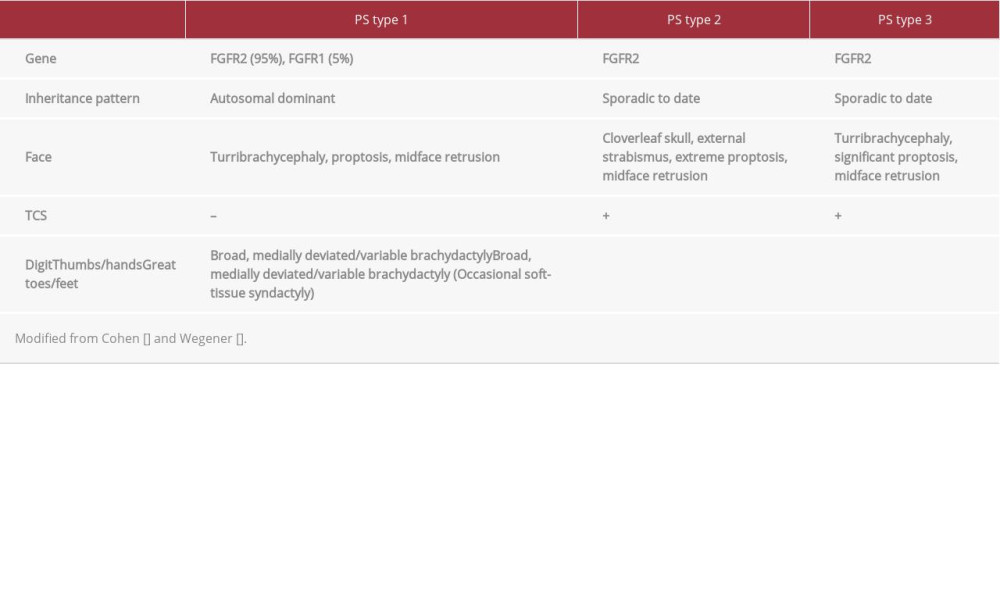
The patient was a 4-year-old girl with no family history of craniosynostosis syndrome among her parents or siblings. In gestational week 20, fetal ultrasonography detected cranial stenosis, hydrocephalus, and exophthalmos. She was born at 37 weeks and 5 days of gestation to her 35-year-old mother by scheduled caesarian section. She was 50 cm long and weighed 2.8 kg at birth. Apgar scores were 8 at 1 min and 5 min, but oxygenation and intubation therapy were needed for cyanosis due to respiratory insufficiency. Macroscopically, cloverleaf skull (Figure 1A, 1B), midface retrusion, medial deviation of the thumbs (Figure 1C, 1D), micromelia, and ankylosis of the elbows were noted (Figure 1E, 1F). Computed tomography offered a clear image of the cloverleaf skull deformity with bulging of the anterior frontal and bilateral temporal regions in association with hydrocephalus (Figure 1A, 1B). The face showed exophthalmos, strabismus, left microophthalmopathy, and mid-face retrusion in the form of a hypoplastic maxilla, saddle nose, and narrow nares. The broad thumbs indicated medial deviation (Figure 1C, 1D). All fingers and toes showed brachydactyly. No syndactyly was found. These congenital abnormalities were consistent with PS type 2 (Table 1). Postnatal genetic testing confirmed heterozygous missense mutation c. 1019A>G (p. Y340C) in the FGFR2 gene. The patient underwent ventriculoperitoneal shunting immediately after birth and tracheotomy at 139 days old for upper airway abnormalities, including choanal stenosis and TCS. A wire-reinforced flexible silicone tube was selected to prevent formation of granulation tissue in the tracheal lumen and to better manage respiration. We were able to easily change the length of this tube, allowing good maintenance of respiration. She underwent planned bronchoscopy every 2 months to evaluate the trachea, which was short and partially narrowed. Using the silicone tube, we could provide care without forming granulation tissue, although good management of patients with TCS with such tubes is widely known to be very difficult. Subsequently, cranioplasties were performed several times. Ventriculoperitoneal shunts were replaced repeatedly owing to shunt malfunctions, such as obstruction and infection. When a sudden change in intracranial pressure caused cardiopulmonary arrest at 2 years old, the patient developed post-resuscitation encephalopathy. Recurrent aspiration pneumonia from TCS made stable breathing difficult to maintain. At 4 years old, she died of multiple organ failure due to aspiration pneumonia.
BODY AND CRANIUM: An autopsy was performed 2.5 h after death. The patient was 69 cm in height and weighed 10 kg. These values were roughly equivalent to those of a 1-year-old child. She had a short neck and micromelia (Figure 1F). Brain autopsy was not permitted, but the gross shape of the cranium was still irregular and supratentorial tissue was lost, which was attributed to the post-resuscitation encephalopathy at 2 years old. The cranial base was visible through the right frontal postoperative fistula.
LARYNX AND LOWER AIRWAY: Macroscopically, the vocal cords, epiglottis, and middle region of the hyoid bone were aplastic (Figure 2A [blue dashed line], 2C). The air tract from the thyroid cartilage to the right and left main bronchi formed a long, tube-like structure. Tracheal rigidity was high because of the absence of cartilaginous rings and marked narrowing of the posterior membranous septum (Figure 2A–2D). Histologically, the tracheal cartilages were mutually fused, resulting in an absence of cartilaginous rings and tracheal ligaments. However, no abnormal changes to tissue structures or cells in the cartilages were evident. No abnormal ossification was observed (Figure 2B). The mucosa of the trachea showed chronic mild inflammation, erosions, and moderate hyperplasia of the submucosal glands (Figure 2E).
LUNGS AND BRONCHI: The lungs weighed 70 g (left) and 77 g (right). Both lungs showed rubbery elasticity and poor aeration. Dilated bronchi had thickened walls encircled by many pieces of cartilage, mainly at the hilum (Figure 3A). These cartilages tended to overlap each other at both ends without any fusions and were highly variable in size and shape (Figure 3B). However, histological examination failed to reveal any abnormalities of tissues and cell structures of the cartilages. Mixed foci of old and new bronchopneumonia were found in areas with rubber-like elasticity on macroscopic inspection (Figure 3C). These foci showed scattered foreign-body giant cells.
OTHER VISCERAL ANOMALIES/FINDINGS:
Diffuse intestinal adhesions attributable to surgical treatment for intestinal malrotation were observed. An accessory spleen, 15 mm in diameter, and an ectopic pancreas, 5 mm in diameter, were detected in the pancreatic tail and proximal jejunum, respectively. No abnormalities were identified in the cardiovascular or urinary tracts. The thymus (12.5 g) was almost fatty, with scarce parenchyma. The adrenal glands were highly atrophic, probably due to prolonged steroid administration (left, 1.4 g; right, 1.3 g). Hemosiderosis was found in the organs of the reticuloendothelial system, such as the spleen, liver, and lymph nodes, and was attributed to repeated blood transfusions. Geographic infarction and organized thrombus were found in the spleen (57.3 g) (Figure 4A, 4B). The kidneys (left, 25.5 g; right, 31.4 g) showed histological immaturity of some glomeruli, particularly in the subcapsular region (Figure 4C). The liver (215 g) revealed diffuse vacuolar degeneration of hepatocytes.
Discussion
Craniosynostosis is a relatively common congenital anomaly characterized by premature fusion on 1 or more cranial sutures.
This anomaly affects 1 in 2000 to 2500 live births [9]. PS is a craniosynostosis syndrome related to mutations of
The cranium shows a cloverleaf form in type 2, and turribrachycephaly (high, prominent forehead) in types 1 and 3. TCS has been reported in types 2 and 3. Craniofacial abnormalities in PS are related to the organs derived from the neural crest [9]. In the head and neck, the neural crest plays essential roles in organogenesis, depending on the
Usual cases of TCS show cartilaginous fusion between the cricoid cartilage and some adjacent tracheal cartilage, although the extent of cartilaginous fusion varies among cases [15]. Generally, the severity of respiratory insufficiency in TCS increases with a wider extent of cartilaginous fusion [16]. Cases with TCS involving as far as the carina, such as our case, reportedly show severe respiratory impairment. Several reports have described TCS in PS with respect to the frequency and prognosis of patients [7,16]. One series found TCS in 5 of 11 PS cases [7]. In another series, 4 of 5 patients with TCS in PS died of respiratory distress or airway complications within 15 months of birth [15]. In the present case, it was very difficult to manage the respiratory function due to the characteristics of PS as described above. It is possible that we were able to maintain respiratory function by using wire-reinforced flexible silicone tubing, which is expected to improve the life expectancy in similar cases.
Autopsy reports including histological findings for PS with TCS remain very limited [6–8]. A histology of ulcer, chronic inflammation, and granulation tissue of the tracheal mucosa has been described [7]. In our case, the trachea with reduced flexibility demonstrated chronic mild inflammation, erosions, and moderate hyperplasia of the submucosal glands. In addition, we observed many non-fused cartilages of various sizes and shapes encircling the dilated bronchi in bilateral lungs. Meanwhile, we could not find any abnormalities of tissue and cell structures on histological examination of the cartilages. Abnormal chondrogenesis in the lower respiratory tracts may correlate closely with TCS.
Reports of PS with systemic organ study at autopsy are also scant. However, one review article described rates of visceral organ abnormalities in PS types 2 and 3, such as urogenital abnormality (22%), gastrointestinal malformation (22%), and cardiac malformation (13%) [18]. One autopsy case described hypoplasia of the gallbladder and loss of the lesser omentum on gross inspection [19]. To the best of our knowledge, no histopathological examination of the visceral organs at autopsy, excluding the trachea, has been reported in the literature. These visceral abnormalities may be related to
Conclusions
We have reported an autopsy case of PS type 2. We performed a systemic histological study of all visceral organs. We observed many non-fused cartilages of various sizes and shapes in the intrapulmonary bronchi. However, we could not identify any histological abnormalities of the tissue and cell structures of the cartilage. Intestinal malrotation was also identified in this case. Further studies are needed to clarify the abnormalities of visceral organs in PS and other
Figures
References:
1.. Vogels A, Fryns JP, Pfeiffer syndrome: Orphanet J Rare Dis, 2006; 1; 1-19
2.. Pfeiffer RA, [Dominant hereditary acrocephalosyndactylia.]: Z Kinderheilkd, 1964; 90; 301-20 [in German]
3.. Cohen MM, Pfeiffer syndrome update, clinical subtypes, and guidelines for differential diagnosis: Am J Med Genet, 1993; 45; 300-7
4.. Schell U, Hehr A, Feldman GJ, Mutations in FGFR1 and FGFR2 cause familial and sporadic Pfeiffer syndrome: Hum Mol Genet, 1995; 4; 323-28
5.. : GeneReviews® [Internet], Seattle, University of Washington, Seattle c1993–2020. (Cited 30 October 2020) FGFR Craniosynostosis Syndromes Overview. https://www.ncbi.nlm.nih.gov/books/NBK1455
6.. Chen JC, Holinger LD, Congenital tracheal anomalies: Pathology study using serial macrosections and review of the literature: Pediatr Pathol, 1994; 14; 513-37
7.. Hockstein NG, McDonald-McGinn D, Zackai E, Tracheal anomalies in Pfeiffer syndrome: Arch Otolaryngol Head Neck Surg, 2004; 130; 1298-302
8.. Stone P, Trevenen CL, Mitchell I, Rudd N, Congenital tracheal stenosis in Pfeiffer syndrome: Clin Genet, 1990; 38(2); 145-48
9.. Flaherty K, Singh N, Richtsmeier JT, Understanding craniosynostosis as a growth disorder: Wiley Interdiscip Rev Dev Biol, 2016; 5(4); 429-59
10.. Lajeunie E, Heuertz S, El Ghouzzi V, Mutation screening in patients with syndromic craniosynostoses indicates that a limited number of recurrent FGFR2 mutations accounts for severe forms of Pfeiffer syndrome: Eur J Hum Genet, 2006; 14(3); 289-98
11.. Zankl A, Jaeger G, Bonafé L, Novel mutation in the tyrosine kinase domain of FGFR2 in a patient with Pfeiffer syndrome: Am J Med Genet A, 2004; 131(3); 299-300
12.. Gonzales M, Heuertz S, Martinovic J, Vertebral anomalies and cartilaginous tracheal sleeve in three patients with Pfeiffer syndrome carrying the S351C FGFR2 mutation: Clin Genet, 2005; 68(2); 179-81
13.. Wenger TL, Dahl J, Bhoj EJ, Tracheal cartilaginous sleeves in children with syndromic craniosynostosis: Genet Med, 2017; 19(1); 62-68
14.. Vega-Lopez GA, Cerrizuela S, Tribulo C, Aybar MJ, Neurocristopathies: New insights 150 years after the neural crest discovery: Dev Biol, 2018; 444(Suppl.1); S110-43
15.. Noorily MR, Farmer DL, Belenky WM, Philippart AI, Congenital tracheal anomalies in the craniosynostosis syndromes: J Pediatr Surg, 1999; 34; 1036-39
16.. Elloy MD, Cochrane LA, Wyatt M, Tracheal cartilaginous sleeve with cricoid cartilage involvement in Pfeiffer syndrome: J Craniofac Surg, 2006; 17; 272-74
17.. Hines EA, Jones MN, Harvey JF, Crouzon syndrome mouse model exhibits cartilage hyperproliferation and defective segmentation in the developing trachea: Sci China Life Sci, 2019; 62; 1375-80
18.. Koga H, Suga N, Nakamoto T, Clinical expression in Pfeiffer syndrome type 2 and 3: surveillance in Japan: Am J Med Genet A, 2012; 158A(10); 2506-10
19.. Hodach RJ, Viseskul C, Gilbert EF, Studies of malformation syndromes in man XXXVI: The Pfeiffer syndrome, association with Kleeblattschädel and multiple visceral anomalies. Case report and review: Z Kinderheilkd, 1975; 119; 87-103
Figures
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250