15 October 2021: Articles 
Successful En Bloc Resection of Locally Advanced Pancreatic Tail Cancer with Colonic Perforation Following Neoadjuvant Chemotherapy: A Case Report
Unusual setting of medical care
Shigeyuki Harada1ABCDEF*, Taku Iida1ABCDF, Satsuki Asai2BCD, Kojiro Nakamura1ABCDF, Misa Ishihara2BCD, Junji Iwasaki1ABCDF, Atsushi Itami1ABCDF, Takahisa Kyogoku1ABCDFDOI: 10.12659/AJCR.933226
Am J Case Rep 2021; 22:e933226
Abstract
BACKGROUND: Distal pancreatic cancers may be unresectable at the time of diagnosis because these cancers are asymptomatic and readily infiltrate neighboring organs. Radical resection of a pancreatic tail cancer with colonic perforation is rare. We describe successful resection of a locally advanced pancreatic tail cancer with colonic perforation using a multidisciplinary approach.
CASE REPORT: A 66-year-old man presented to our hospital with a chief concern of high fever. Abdominal computed tomography revealed a pancreatic tail tumor infiltrating the neighboring organs and causing colonic obstruction with perforation, which resulted in an intra-abdominal abscess. Colonoscopy revealed obstruction of the descending colon by extramural invasion. Laboratory tests showed high tumor marker concentrations (carcinoembryonic antigen, 11.6 ng/dL; pancreatic cancer-associated antigen-2, >1600 U/mL). We clinically diagnosed locally advanced pancreatic tail cancer with an intra-abdominal abscess caused by colonic perforation. First, we performed transverse colostomy and percutaneous drainage. We then started neoadjuvant chemotherapy with FOLFIRINOX for tumor shrinkage and prevention of distant metastases. The therapeutic effect was a partial response, and no distant metastases was found. We therefore performed radical surgery comprising distal pancreatectomy with partial resection of neighboring organs. Although pathological examination revealed a pancreatic tail tubular adenocarcinoma with direct invasion of the neighboring organs, R0 resection was achieved. The patient was discharged with no perioperative complications. Tegafur/gimeracil/oteracil potassium were administered as adjuvant chemotherapy. The patient remained recurrence-free for 19 months after surgery.
CONCLUSIONS: We achieved successful en bloc resection of a locally advanced distal pancreatic cancer with colonic perforation by using a multidisciplinary approach.
Keywords: Colon, Neoadjuvant Therapy, Pancreatic Cancer, Adult, Antineoplastic Combined Chemotherapy Protocols, Humans, Pancreatectomy, Pancreatic Neoplasms
Background
Some distal pancreatic cancers are unresectable at the time of diagnosis because they are characteristically asymptomatic and readily infiltrate neighboring organs or blood vessels and metastasize to distant locations. Therefore, the prognosis of distal pancreatic cancer is poor [1]. Solcie et al have reported that infiltration of the colon by pancreatic tail cancers is not rare, occurring in up to about 17% of cases [2]. However, most pancreatic tail cancers with colonic obstruction caused by infiltration are not resectable because of the presence of distant metastases. Diagnosis of pancreatic tail cancer on the basis of evidence of colonic perforation is unusual [3]. Attaining R0 re-section of pancreatic cancers is important for achieving long-term survival after radical surgery [4]. However, R0 resection of pancreatic tail cancer with colonic perforation is relatively rarely achieved. Herein, we describe successful en bloc resection with negative surgical margins of a locally advanced pancreatic tail cancer with colonic perforation, which result in intra-abdominal abscess following neoadjuvant chemotherapy (NAC).
Case Report
A 66-year-old Japanese man presented to our hospital with a chief concern of high fever. Abdominal computed tomography (CT) revealed a pancreatic tail tumor. The pancreatic tail tumor was infiltrating the abdominal wall, spleen, left kidney, and splenic flexure of the transverse colon. Colonic obstruction occurred by pancreatic cancer invasion, resulting in an intra-abdominal abscess formation near the splenic flexure of the transverse colon (Figure 1). No distant metastases were detected in the lungs, peritoneum, or other organs. Lower gastrointestinal endoscopy revealed that the tumor had compressed and obstructed the descending colon from the serosal wall (Figure 2). No malignant cells were found in a mucous membrane biopsy. Additionally, laboratory testing showed high tumor marker concentrations (carcinoembryonic antigen, 11.6 ng/dL; carbohydrate antigen 19-9, <2.0 U/mL; pancreatic cancer-associated antigen-2 >1600 U/mL) (Table 1). Therefore, we clinically diagnosed a locally advanced pancreatic tail cancer with the colonic obstruction with perforation and intra-abdominal abscess formation as a result of infiltration of the splenic flexure of the transverse colon. First, we urgently performed a transverse colostomy and percutaneous drainage for the intra-abdominal abscess for infection control. When we performed percutaneous drainage, we did not perform a cytology exam of the intra-abdominal abscess. After strict infection control, we started first-line treatment as neoadjuvant chemotherapy for locally advanced pancreatic cancer with FOLFIRINOX in light of the patient’s performance status. FOLFIRINOX consisted of oxaliplatin at a dose of 85 mg per square meter, given as a 2-hour intravenous infusion, immediately followed by leucovorin calcium at a dose of 200 mg per square meter, given as a 2-hour intravenous infusion, with the addition, after 30 minutes, of irinotecan hydrochloride hydrate at a dose of 180 mg per square meter, given as a 90-minute intravenous infusion through a bypass injection. This treatment was immediately followed by fluorouracil at a dose of 400 mg per square meter given by intravenous bolus, followed by a continuous intravenous infusion of 2400 mg per square meter over 46 hours given every 2 weeks.
After 6 courses of FOLFIRINOX without any adverse events, the size of the main tumor in the pancreatic tail was reduced from 36 mm at baseline to 23 mm in diameter at the end of neoadjuvant therapy. According to the RECIST guidelines [5], partial response was achieved. Although there was persistent invasion of the abdominal wall, spleen, descending colon, and left kidney, no distant metastases were detected by preoperative CT after NAC. We therefore considered that we could perform radical surgery comprising distal pancreatectomy (DP) and re-section of other affected organs. We successfully performed DP with partial resection of the colon, stomach, jejunum, abdominal wall, left adrenal gland, and kidney and closure of the transverse colostomy. The resected specimen had a hard elastic mass in the pancreatic tail surrounded by the other organs, namely the stomach, jejunum, spleen, transverse colon, left kidney, and a part of abdominal wall (Figure 3A). Pathological examination of hematoxylin and eosin-stained sections of the resected specimen revealed that the main tumor, which was located in the pancreatic tail, was a tubular adenocarcinoma that had infiltrated the abdominal wall, spleen, transverse colon, and left renal capsule. Infiltration of the transverse colon into the muscularis propria was found (Figure 3B). Although the histological evaluation of resected specimen demonstrated colonic obstruction due to the stenosis of cancer infiltration, cancer infiltration was not histologically identified at the perforated site. The final pathological stage was T3N1M0, Stage IIB according to the eighth edition of the TNM classification of malignant tumors of UICC [6]. Although the tumor size was reduced by the NAC, the histological response to neoadjuvant chemotherapy was Evans grade I [7]. We succeeded in performing R0 resection with negative surgical margins by resecting all affected organs.
The postoperative course was uneventful. The patient was discharged on postoperative day 27 having had no perioperative complications. Adjuvant chemotherapy comprising tegafur/ gimeracil/oteracil potassium was administered for 6 months. There has been no evidence of recurrence or complications in the 19 months since radical surgery.
Discussion
Thanks to developments in medical technology in recent years, we are now able to detect and treat many kinds of cancer at an early stage. However, because most pancreatic tail cancers are asymptomatic, some are classified as locally advanced cancers at the time of diagnosis [1]. Attaining R0 resection of pancreatic cancers is important for achieving long-term survival after radical surgery [4]. The International Study Group for Pancreatic Surgery has established a clear definition of extended DP associated with resection of any of the following involved organs: stomach, colon, small bowel, left adrenal gland, left kidney, diaphragm, and contiguous liver. Major arterial or venous resections are also included in the definition. Despite increased perioperative morbidity, extended pancreatectomy is warranted to achieve long-term survival of patients with pancreatic ductal adenocarcinoma if R0 resection can be achieved [8]. Therefore, DP with resection of multiple viscera should be considered with the aim of achieving R0 re-section in fit patients with locally advanced pancreatic cancer.
Several investigators have demonstrated that resection of multiple viscera in patients with pancreatic cancer may increase postoperative complications. This applies particularly to patients who undergo resection of a kidney or the colon, who require intraoperative transfusions, and whose operative procedures are lengthy. Nevertheless, these patients’ long-term prognoses may be better than after standard DP [9,10]. However, extended DP did not increase the rates of postoperative pancreatic fistula, post-pancreatectomy hemorrhage, or major complications [11]. Although the safety and effectiveness of extended DP are still controversial, extended DP with the aim of achieving R0 resection and long-term survival is permissible. However, the indications for such radical surgery should be carefully considered, keeping in mind the possibility of complications such as anastomotic leakage, pancreatic fistula, and other major complications.
We have herein reported successful en bloc resection by extended DP following NAC of a pancreatic tail cancer with colonic obstruction, perforation, and formation of an intra-abdominal abscess secondary to infiltration of the splenic flexure of the transverse colon and other affected organs, without perioperative complications. Although this case was locally advanced case, we considered the case to be resectable by multivisceral organ resection without NAC. However, locally advanced cases often have early local and distant recurrences after surgery. Therefore, we consider and expect that neoadjuvant chemo-therapy can contribute to not only the tumor reduction, but also the prevention of distant metastases. Although the response was partial, we considered that in this case NAC could contribute to a sufficient surgical margin to achieve R0 resection without distant metastases.
Successful extended DP with a partial resection of the thoracic wall after downstaging by NAC using FOLFIRINOX was first reported in 2020 by Giuliani et al [12]. These authors stressed the importance of administering neoadjuvant strategies such as chemotherapy and radiotherapy with the aim of downstaging or reducing the tumor size in patients with locally advanced or borderline resectable pancreatic cancer [12]. Additionally, it has been shown that neoadjuvant therapy such as chemo-therapy or chemoradiotherapy facilitates attainment of negative margins after resection of originally borderline or locally advanced pancreatic cancer [13].
In the present patient, we selected and administered FOLFIRINOX based on a meta-analysis showing that neoadjuvant chemotherapy with FOLFIRINOX for locally advanced pancreatic cancer achieves better overall and R0 resection rates than does therapy with gemcitabine [14]. The objective response rate of the FOLFIRINOX group was better than that of the gemcitabine group (31.4% versus 9.4%) [15]. A meta-analysis reported that the complete response rate after treatment with FOLFIRINOX was 2.9%, the partial response rate was 35.9%, and the stable disease rate was 41.2% [16]. Another report showed that partial response was more common with FOLFIRINOX than with gemcitabine and nab-Paclitaxel (19% versus 6%) [17].
FOLFIRINOX as NAC is required to achieving radical resection and long-term survival because the operative outcomes and survival of the patients treated with neoadjuvant FOLFIRINOX are better than those of patients with borderline resectable/l ocally advanced cancer who undergo upfront resection [18].
Therefore, in this case, we were able to perform extended DP and achieve en bloc R0 resection with no complications using NAC with FOLFIRINOX with the aim of downstaging, tumor shrinkage, and prevention of distant metastases and early postoperative recurrence.
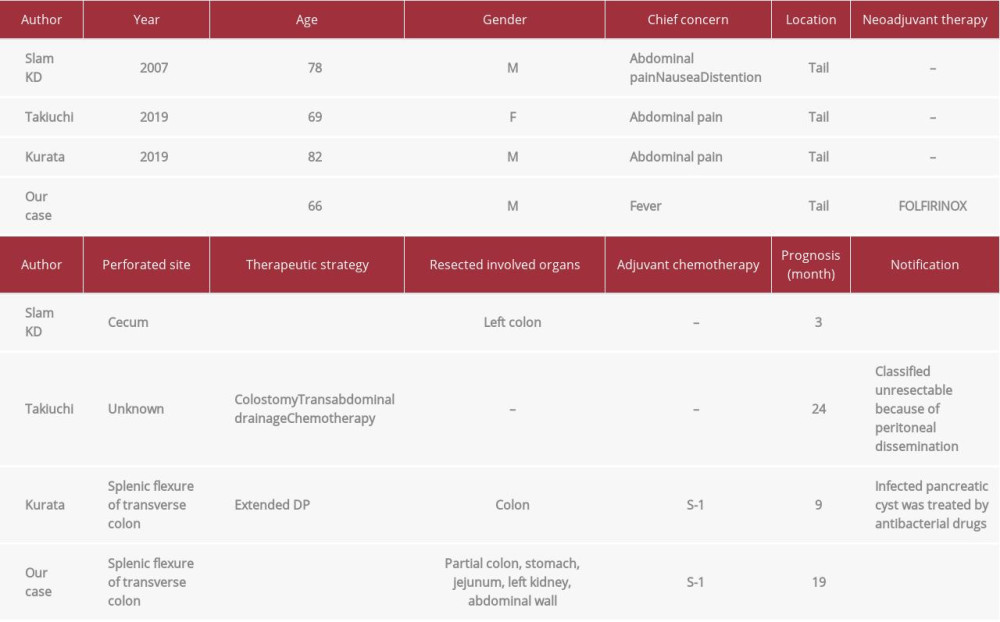
Abscess formation caused by colonic perforation is a very rare complication associated with pancreatic cancer. Searches for the terms “pancreatic cancer with colonic perforation” in PubMed from inception to 2020 yielded only 4 cases, including our case (Table 2) [19–21]. The pancreatic tumor was located in the pancreatic tail of all 4 patients. Two patients, including ours, had developed perforation at the splenic flexure of the transverse colon by direct infiltration [21]. The perforation in 1 patient had occurred at the cecum by increasing intra-colonic pressure [19]. Two patients, including ours, underwent urgent colostomy and percutaneous or transabdominal drainage [20]. The other 2 patients underwent right hemicolectomy or treatment with antibacterial drugs [19,21]. Because 1 patient had peritoneal dissemination, radical resection was not performed [20]. NAC was administered only in our case. Additionally, adjuvant chemotherapy was performed in 2 cases, including ours [21].
As mentioned above, because NAC is a requisite for locally advanced pancreatic cancer to achieve R0 resection and long-term survival, infection control is very important before NAC. In our case, by performing urgent percutaneous drainage of the intra-abdominal abscess and temporary colostomy for a strict infection control, NAC could be introduced promptly and safely. Of course, administration of adjuvant chemotherapy is also important for prevention of postoperative recurrence. Through multidisciplinary treatment, our present patient achieved recurrence-free survival for 19 months after surgery despite the locally advanced nature of the cancer.
Conclusions
In conclusion, although colonic perforation and the intra-abdominal abscess formation were very rare and difficult complications, we achieved successful en bloc R0 resection of a locally advanced distal pancreatic cancer with colonic perforation by using a multidisciplinary treatment that included infection control by colostomy, drainage, and NAC with FOLFIRINOX.
Figures
References:
1.. Ohata K, Uenishi T, Miyazaki T, [A resected case of the pancreatic tail cancer with obstruction of the large intestine.]: Nihon Gekakei Rengo Gakkaishi, 2014; 39(4); 761-66 [in Japanese]
2.. Solcie E, Capella C, Kloppel G, Tumors of the pancreas. In: Atlas of Tumor Pathology, Third Series Fascicle 20: Armed Forces Institute of Pathology, 1995; 85-86
3.. Kobayashi M, Matsuura K, Araki K, A long-term survival case of pancreas tail cancer with colonic obstruction: Japanese Journal of Gastroenterological Surgery, 1996; 29(3); 756-60
4.. Hank T, Hinz U, Tarantino I, Validation of at least 1 mm as cut-off for resection margins for pancreatic adenocarcinoma of the body and tail: Br J Surg, 2018; 105(9); 1171-81
5.. Eisenhauer EA, Therasse P, Bogaerts J, New response evaluation criteria in solid tumours: Revised RESIST guideline (version 1.1): Eur J Cancer, 2009; 45(2); 228-47
6.. James DB, Mary KG, Christian W: TNM Classification of Malignant Tumours, 2017, New Jersey, John Wiley & Sons, Ltd
7.. Evans DB, Rich TA, Byrd DR, Preoperative chemoradiation and pancreaticoduodenectomy for adenocarcinoma of the pancreas: Arch Surg, 1992; 127; 1335-39
8.. Hartwig W, Vollmer CM, Fingerhut A, International Study Group on Pancreatic Surgery. Extended pancreatectomy in pancreatic ductal adeno-carcinoma: Definition and consensus of the International Study Group for Pancreatic Surgery (ISGPS): Surgery, 2014; 156; 1-14
9.. Burdelski CM, Reeh M, Bogoevski D, Multivisceral resections in pancreatic cancer: Identification of risk factors: World J Surg, 2011; 35(12); 2756-63
10.. Solaini L, de Rooji T, Marsman EM, Pancreatoduodenectomy with colon resection for pancreatic cancer: A systematic review: International Hepato-Pancreato-Biliary Association, 2018; 20; 881-87
11.. Malinka T, Klein F, Andreou A, Distal pancreatectomy combined with multivisceral resection is associated with postoperative complication rates and survival comparable to those after standard procedures: J Gastrointest Surg, 2018; 22; 1549-56
12.. Giuliani T, Rubio ML, Oron EM, Extended distal pancreatectomy with thoracic wall resection after neoadjuvant FOLFIRINOX: Is there a limit of resection for pancreatic cancer after downstaging?: Anna Hepatobiliary Pancreat Surg, 2020; 24(1); 90-96
13.. Zhan HX, Xu JW, Wu D, Neoadjuvant therapy in pancreatic cancer: A systematic review and meta-analysis of prospective studies: Cancer Med, 2017; 6(6); 1201-19
14.. Suker M, Beumer BR, Sadot E, FOLFIRINOX for locally advanced pancreatic cancer: A systematic review and patient-level meta-analysis: Lancet Oncol, 2016; 17(6); 801-10
15.. Conroy T, Desseigne F, Ychou M, FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer: N Engl J Med, 2011; 364(19); 1817-25
16.. Hongxuan T, Zhu F, Biyuan L, Tao L, The benefits of modified FOLFIRINOX for advanced pancreatic cancer and its induced adverse events: A systematic review and meta-analysis: Sci Rep, 2018; 8(1); 8666
17.. Giampaolo P, Laura P, Wei Q, Response and survival associated with first-line FOLFIRINOX vs Gemcitabine and nab-Paclitaxel chemotherapy for localized pancreatic ductal adenocarcinoma: JAMA Surg, 2020; 155(9); 832-39
18.. Theodoros M, Ilaria P, Carlos FC, Predictors of resectability and survival in patients with borderline and locally advanced pancreatic cancer who underwent neoadjuvant treatment with FOLFIRINOX: Ann Surg, 2019; 269(4); 733-40
19.. Slam KD, Calkins S, Cason FD, LaPlace’s law revisited: Cecal perforation as an unusual presentation of pancreatic carcinoma: World J Surg Oncol, 2007; 5; 14
20.. Takiuchi D, Morimoto O, Eguchi S, [A case of chemotherapy with abscess drainage for pancreatic cancer detected due to peritonitis.]: Gan To Kagaku Ryoho, 2019; 46(13); 2458-60 [in Japanese]
21.. Kurata T, Asakawa T, Fujimori D, [Intraductal papillary mucinous carcinoma with penetration in the colon and retrograde infection – a case report.]: Gan To Kagaku Ryoho, 2019; 46(13); 2545-47 [in Japanese]
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250