16 November 2021: Articles 
Reversible Cerebral Vasoconstriction Syndrome in a Background of Eclampsia Responding to Milrinone Infusion
Unusual or unexpected effect of treatment
Kawther M. Hadhiah1ABCDEF*, Ziyad A. Alshagawi2ABCDEF, Saleh K. Alzahrani2ABCDEF, Majd M. Alrayes2ABCDEF, Hassan W. AldandanDOI: 10.12659/AJCR.934528
Am J Case Rep 2021; 22:e934528
Abstract
BACKGROUND: Reversible cerebral vasoconstriction syndrome (RCVS) is a rare neurological disorder with a complex physiopathology that is not fully understood. Suggested underlying mechanisms include failure of autoregulation, endothelial dysfunction, and oxidative stress. It is characterized by reversible multifocal constriction of the cerebral arteries, and can be triggered by many conditions, including, vasoactive medications (eg, triptans), cerebrovascular events, primary headache disorders, and metabolic causes (eg, hypercalcemia). RCVS can also be associated with pregnancy-related conditions, such as thrombotic thrombocytopenic purpura, eclampsia, and pre-eclampsia. Thunderclap headache is the most common clinical manifestation; however, other symptoms can result from complications of the disease, such as stroke, brain edema, and seizures. Several case reports have been published of an association between RCVS and eclampsia, but to the best of our knowledge, only 3 cases were successfully treated with intravenous milrinone and this is the only patient reported in Saudi Arabia.
CASE REPORT: We report a case of 25-year-old primigravida woman who presented with acute-onset headache, nausea, elevated blood pressure, and generalized tonic clonic seizure. She was diagnosed as having RCVS secondary to eclampsia based on clinical and radiological features. She was initially started on nimodipine, which is usually the first-line management of RCVS, as well as magnesium sulfate and levetiracetam; however, she only achieved full recovery after starting intravenous milrinone.
CONCLUSIONS: Milrinone is one of the emerging drugs for treatment of RCVS, and this case report delineates the potential of using the drug, especially in cases refractory to standard therapy.
Keywords: Eclampsia, magnesium sulfate, Milrinone, Cerebrovascular Disorders, Female, Headache Disorders, Primary, Humans, Pregnancy, Vasoconstriction
Background
Pregnancy and the postpartum period cause significant physiological changes that carry a risk for vascular and cerebrovascular complications that have detrimental effects on the mother and the fetus. A well-known complication is pre-eclampsia/eclampsia, and the rarest complication is reversible cerebral vasoconstriction syndrome (RCVS), also known as Call-Fleming syndrome or postpartum cerebral angiopathy, which is a group of disorders characterized by multifocal constriction of cerebral arteries, typically manifesting as thunderclap headache. Other clinical manifestations are related to the possible neurological sequela of the disease, including ischemic stroke, brain edema, convexity subarachnoid hemorrhage, lobar hemorrhage, and seizures [1]. High blood pressure is also a common finding, which may be due to an associated condition such as eclampsia or cocaine use; however, it can also be the result of acute pain distress. Many conditions have been linked to RCVS, including pregnancy and its associated complications such as eclampsia and pre-eclampsia [2], primary headache disorders (eg, migraine and primary thunderclap headache), the use of vasoconstrictive medications (eg, triptans, phenylpropanolamine, amphetamine), metabolic derangements (eg, hypercalcemia), and cerebrovascular phenomena (eg, cerebral venous thrombosis, cervical artery dissection, and posterior reversible encephalopathy syndrome) [3]. The pathophysiology of RVCS is poorly understood; however, suggested underlying mechanisms include failure of autoregulation, endothelial dysfunction, and oxidative stress.
We report a rare case of a woman presenting with both pre-eclampsia/eclampsia and RCVS prior to delivery and day 1 post-partum, respectively. To the best of our knowledge, there are only 12 cases worldwide with the combination of eclampsia and RVCS. This is the fourth reported patient to be successfully treated with intravenous milrinone and the first one to be reported in Saudi Arabia.
Case Report
A 25-year-old primigravida woman with no past medical history presented to our Emergency Department at 38 weeks of gestation with a 1-day history of headache, nausea, epigastric abdominal pain shortness of breath, and hypertension (blood pressure: 180/100).
She was admitted to the delivery room as a case of pre-eclampsia with severe features, where she had new-onset generalized tonic clonic seizures with no focal neurological deficit, so she was diagnosed with eclampsia, was intubated, and underwent emergency cesarean section, with magnesium sul-fate infusion and labetalol bolus to control her blood pressure. She achieved a magnesium level of 6 and her deep tendon reflexes were depressed, so the magnesium sulfate infusion had to be stopped. After a couple of hours, she had another episode of generalized tonic clonic seizures, so she received a loading dose of levetiracetam (20 mg/kg) with initiation of propofol infusion. CT brain and CT venogram were done as she was stabilized; CT brain showed convexity subarachnoid hemorrhage (Figure 1), with negative CT venogram.
The next day during sedation vacation, she continued to be comatose and a CT angiogram was done, which showed a stable convexity subarachnoid hemorrhage and diffuse vasoconstriction in different territories of the circle of Willis, with no aneurysm (Figure 2). TCD showed an MCA velocity of 200 cm/s (Table 1) and EEG showed features of encephalopathy with no electrographic seizure. She received nimodipine, which is usually the first-line treatment for RCVS along with other CCBs such as nicardipine. However, there was no change in TCD readings within 48 h.
Because the patient did not improve on nimodipine, she was started on i.v. milrinone bolus 75 mcg/kg/min and then infusion up to 1.75 mcg/kg/min, depending on her blood pressure and daily TCD. She had an arterial line inserted to guide us in case of an unexpected drop in blood pressure.
An MRI brain was done later and showed resolution of convexity SAH, with no vasogenic edema or diffusion restriction (Figure 3). Her TCD readings showed significant improvement 5 days after initiation of therapy (Table 1). Clinical improvement was also noticed, as she started opening her eyes spontaneously and obeying commands, and no focality was found on neurological examination. However, she developed MRSA pneumonitis with increase oxygen requirement for which she was kept intubated and underwent a tracheostomy due to respiratory issues.
During her intensive care course, there were no further episodes of high blood pressure, as she was maintained on magnesium sulfate, amlodipine and methyldopa along with the i.v. milrinone infusion. There were no more episodes of generalized tonic clonic seizures, as she was maintained on levetiracetam 1000 mg twice daily. After discharge, she had a modified Rankin scale of 0.
Tests results are shown in Table 2, including CT: Convexity SAH (Figure 1), CT venogram: negative for sinus thrombosis CT angiogram: diffuse vasoconstriction involved all cerebral arteries (Figure 2) MRI brain: un-remarkable (Figure 3), and TCD readings (Table 1).
Discussion
We present the case of a patient with well-documented eclampsia associated with RCVS that was improved with intravenous milrinone infusion and discuss how similar these 2 conditions can be in clinical presentation [3], which includes headache, hypertension, seizures, and focal neurological deficits. Eclampsia as defined by the American College of Obstetricians and Gynecologists (ACOG) is the occurrence of new-onset seizures or coma, both of which can occur in RCVS, in a patient who has been diagnosed with pre-eclampsia. Reversible cerebral vasoconstriction syndrome (RVCS) is characterized by multifocal vasoconstriction that gives the cerebral arteries the appearance of a “string of beads” [5]. The patho-physiology is poorly understood; it includes dysregulation of cerebral vascular tone, endothelial dysfunction, and oxidative stress leading to blood-brain barrier injury [6]. It has a female predominance, with a female: male sex ratio of 2: 1, with some reports showing a ratio as high as 10: 1. In females, it most commonly presents in the early to mid-forties and in men it presents a decade earlier, but it can occur at any age, including childhood [7]. It is considered an under-diagnosed entity due to the clinical and the pathophysiological overlap with pre-eclampsia/eclampsia, especially when the CT scan is negative [6]. RCVS usually peaks within 2 weeks postpartum and resolves spontaneously after 3 months. However, RVCS needs to be treated, as most patients have brain pathology such as infarction, convexity SAH, lobar intracranial hemorrhage, or brain edema [5]. In our patient there were clinical and radiological findings supporting the diagnosis of RCVS, including the correlation with pregnancy and the concurrent eclampsia, new-onset headache, and seizures with radiological vasoconstriction confirmed by transcranial Doppler (TCD) and CT angiogram. The treatment of RVCS is very controversial and it is mainly based on case series and expert opinion. It may include trail of triple-H as in SAH-related vasospasm, nimodipine (60 mg every 4 h for 21 days), corticosteroids, immunoglobulins, and in refractory cases endovascular therapy either intra-arterial verapamil, nicardipine, or angioplasty. In the literature, there are only 3 patients successfully treated with milrinone (phosphodiesterase inhibitor-3); 2 of them were post- partum women and 1 was a post-transplant patient on tacrolimus [5]. Our patient was started on nimodipine; however, there was no improvement in TCD readings after 48 h; therefore, a decision was made to start i.v. milrinone bolus 75 mcg/kg/min and then infusion up to 1.75 mcg/kg/min.
We believe that milrinone contributed to the improvement of our patient through various mechanisms. In addition to its anti-inflammatory effect, phosphodiesterase inhibitor type 3 has a vasodilatory effect that may have contributed to the resolution of cerebral vasospasm. The most worrisome adverse event related to milrinone use in these patients is hypotension, which can have detrimental effects on cerebral blood flow, leading to more ischemia. Close monitoring and adding inotropic medications can prevent a sudden drop in blood pressure.
Conclusions
Milrinone is increasingly used in the treatment of RCVS, especially for conditions that are refractory to the current standard of care, and this case report may help advance the treatment of RCVS.
Figures
References:
1.. Singhal AB, Cerebral vasoconstriction syndrome: Top Stroke Rehabil, 2004; 11(2); 1-6
2.. Singhal AB, Hajj-Ali RA, Topcuoglu MA, analysis of 139 cases: Arch Neurol, 2011; 68(8); 1005-12
3.. Singhal AB, Bernstein RA, Postpartum angiopathy and other cerebral vasoconstriction syndromes: Neurocrit Care, 2005; 3(1); 91-97
4.. Fletcher JJ, Kramer AH, Bleck TP, Solenski NJ, Overlapping features of eclampsia and postpartum angiopathy: Neurocrit Care, 2009; 11; 199-209
5.. McIlroy E, Sethuraman R, Woograsingh R, Severe postpartum head-ache and hypertension caused by reversible cerebral vasoconstriction syndrome: A case report: A A Case Rep, 2017; 9(10); 289-91
6.. Hawkes MA, Hlavnicka AA, Wainsztein NA, Reversible cerebral vasoconstriction syndrome responsive to intravenous milrinone: Neurocrit Care, 2019; 32; 348-52
7.. Arrigan MT, Heran MKS, Shewchuk JR, Reversible cerebral vasoconstriction syndrome: An important and common cause of thunderclap and recurrent headaches: Clin Radiol, 2018; 73(5); 417-27
Figures
Tables
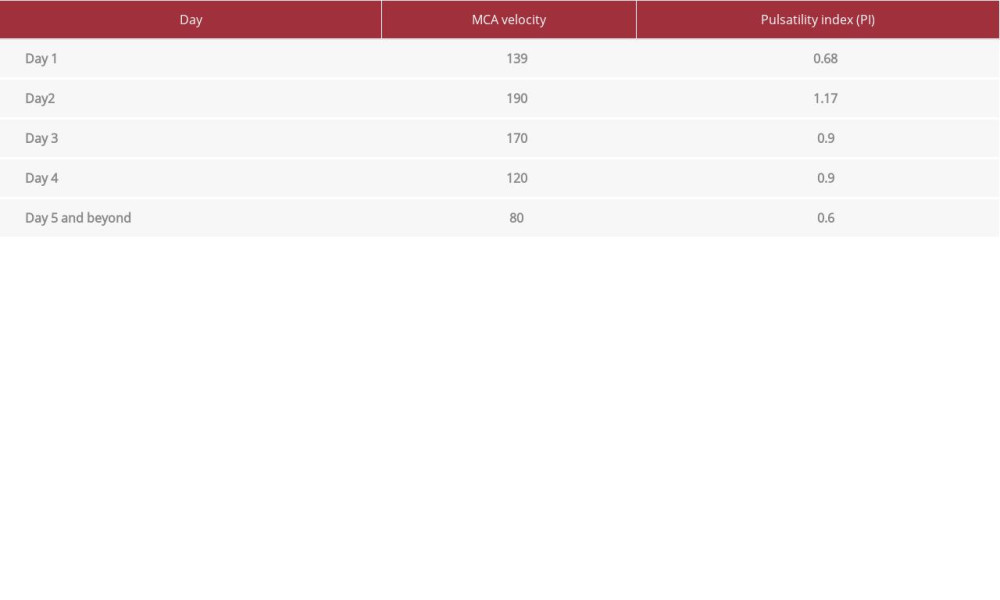 Table 1.. TCD readings(Left MCA at depth of 45 mm via temporal window, the right temporal window was difficult).
Table 1.. TCD readings(Left MCA at depth of 45 mm via temporal window, the right temporal window was difficult). Table 2.. Laboratory work* Urine albumin was not done due to unavailability of the reagent.
Table 2.. Laboratory work* Urine albumin was not done due to unavailability of the reagent.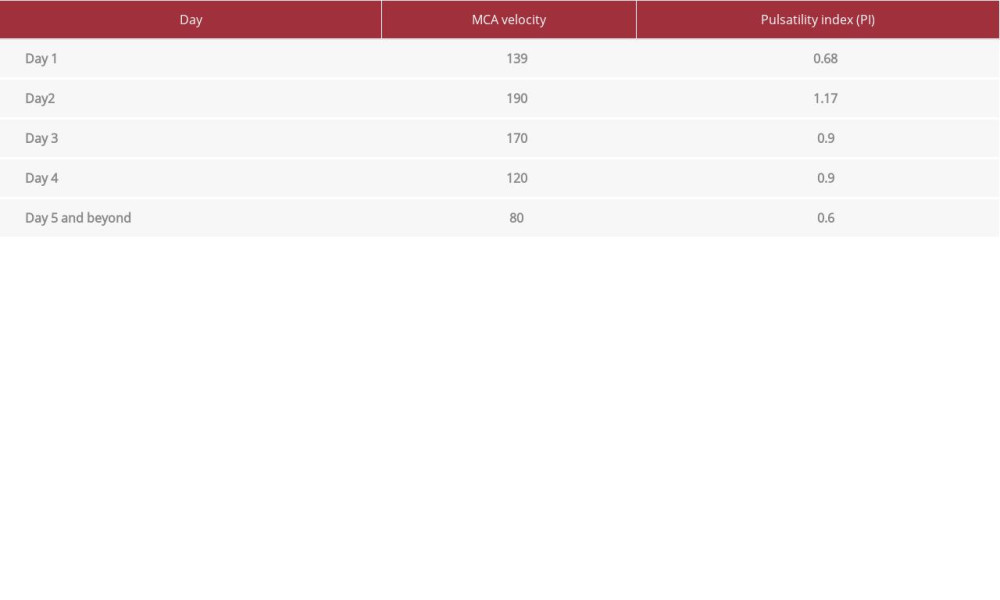 Table 1.. TCD readings(Left MCA at depth of 45 mm via temporal window, the right temporal window was difficult).
Table 1.. TCD readings(Left MCA at depth of 45 mm via temporal window, the right temporal window was difficult). Table 2.. Laboratory work* Urine albumin was not done due to unavailability of the reagent.
Table 2.. Laboratory work* Urine albumin was not done due to unavailability of the reagent. In Press
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942966
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942032
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








