06 February 2022: Articles 
Effectiveness of Hydro-Dissection of the Piriformis Muscle Plus Low-Dose Local Anesthetic Injection for Piriformis Syndrome: A Report of 2 Cases
Unusual or unexpected effect of treatment, Rare disease
Mihiro Kaga1ABCDEF*, Takeshi Ueda1DDOI: 10.12659/AJCR.935346
Am J Case Rep 2022; 23:e935346
Abstract
BACKGROUND: Piriformis syndrome causes severe buttock and low back pain and numbness of the lower limbs, leading to difficulty in walking. The lack of unified diagnostic criteria for piriformis syndrome until 2018 made it difficult to diagnose; therefore, it is often underestimated, and some patients do not receive appropriate treatment. Treatment methods include local anesthetic injection, steroid injection, and local botulinum toxin injection. However, the most effective drug for the treatment of severe piriformis syndrome has not been established. This report aimed to propose a new and more effective treatment for piriformis syndrome with a minimal risk of adverse effects.
CASE REPORT: We performed ultrasound-guided hydro-dissection of the superficial and deep surfaces of the piriformis muscle under local anesthesia (a mixture of 18 mL of saline and 2 mL of 1% lidocaine) in 2 flexion, adduction, and internal rotation test-positive patients with tenderness of the piriformis muscle. In both patients, symptoms improved quickly after injection. One required hospital treatment but gradually returned to previous activities of daily living (ADL) status 5 days after admission and was then discharged. The other patient received 2 injections weekly to improve ADL status with continued lifestyle guidance.
CONCLUSIONS: Hydro-dissection by ultrasound-guided injection of a very low concentration of local anesthetic is effective and has lower risk of adverse effects, thus making it more convenient for the treatment of piriformis syndrome than conventional treatments, such as local anesthetics, steroids, and botulinum toxin injection.
Keywords: Injections, Piriformis Muscle Syndrome, saline solution, Ultrasonography, Activities of Daily Living, Anesthesia, Local, Anesthetics, Local, Humans, Muscle, Skeletal
Background
First reported in 1928 [1], the term “piriformis syndrome” (PS) was first introduced in 1947 [2]. It is characterized by buttock pain and is responsible for 0.3–6% of all cases of buttock and low back pain [3–5]. In its severe form, it causes severe buttock and low back pain and numbness of the lower limbs, leading to difficulty in walking and inability to maintain a sitting or supine posture [6] and significant impairment of daily and social life. PS is due to the pressure exerted on the sciatic nerve, and the pathologies contributing to its development include anatomical abnormalities of the sciatic nerve and piriformis muscle [7], piriformis muscle injury due to trauma [8], piriformis muscle hypertrophy [9], and piriformis muscle spasms [10]. Adhesions between the piriformis muscle and the tissue around the sciatic nerve running proximal to the piriformis muscle have been reported to have a significant impact on PS [11–13]. There were no established diagnostic criteria for PS until 2018, when a systematic review revealed 4 defining symptoms: buttock pain, pain aggravated on sitting, external tenderness near the greater sciatic notch, pain on any maneuver that increases piriformis muscle tension, and limitation of straight leg raising [14]. Due to its rarity and difficulty to diagnose, its prevalence is underestimated [15], which may explain why some PS patients do not receive appropriate treatment. A delay in diagnosis may lead to chronic physical impairment, hyperesthesia, pain, and muscle weakness [16]. Therefore, physicians are required to provide early diagnosis and treatment for PS, which may include physiotherapy, drugs, and injection therapy. If conservative treatment fails, surgery (piriformis tenotomy and decompression of the sciatic nerve) is recommended [17].
Injection therapy includes injection of a local anesthetic, steroid, or botulinum toxin. However, the most effective infusion drug for PS treatment has not been established [18]. Ultrasound-guided injection therapy, which is commonly used for PS treatment, allows more accurate injection into the target site [19]. Furthermore, successful injection therapy indicates a correct diagnosis. Therefore, injection therapy is clinically significant, as it can be used as a diagnostic tool [18].
To the best of our knowledge this is the first report to review 2 cases of patients with PS who underwent successful treatment under an extremely low concentration of local anesthetic.
Case Reports
PATIENT A:
The patient was a 71-year-old man who had been working as a caregiver for >20 years. He had a medical history of hypertension and inguinal hernia, and a surgical history for hernioplasty during his childhood. He had no current history of oral medication and allergy. Five days before presenting to the hospital, he experienced left buttock pain, which prompted him to visit the Department of Emergency and General Internal Medicine at our hospital. He had no history of obvious trauma, and the abdominal CT showed no abnormalities; a diagnosis of musculoskeletal pain was made. The patient was prescribed analgesics and was consequently discharged. However, his buttock pain continued to worsen thereafter, making him unable to sit and sleep. Subsequently, he found it difficult to walk because the pain radiated to the left lower limb while ambulating. Therefore, he returned to the department the following day. His vital signs were normal during consultation. In the sitting position, the center of the mass of the trunk was positioned toward the right side, as the left buttock was out of the chair to evaluate his worsening buttock pain. A physical examination in the prone position showed compression of a taut band (ie, a rope-like induration) by the left piriformis muscle and reproducible tenderness at a point in the same region. Flexion, adduction, and internal rotation (FAIR) test was positive, and the straight leg raise (SLR) test of the left leg showed increased buttock pain at 45°. The results for manual muscle testing of the lower limbs and the lower limb tendon reflex were normal, without sensory disturbance.
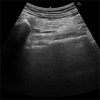
Based on the above results, he was diagnosed with PS. The pathology was determined as myofascial pain syndrome (MPS) of the piriformis muscle based on palpation, since the examination findings conformed to the characteristics of MPS [20]. Considering the possibility of myofascial adhesions related to MPS, hydro-dissection of the superficial and deep surfaces of the left piriformis muscle was performed in the prone position with an ultrasound-guided injection (18 mL of saline plus 2 mL of 1% lidocaine) using the out-of-plane technique (Figures 1, 2). Ultrasonography was performed before the injection to identify the sciatic nerve and inferior gluteal artery, thus avoiding accidental puncture. After the injection, the buttock pain rapidly disappeared, leading to decompression of the taut band by the left piriformis muscle and resolution of tenderness. The Numerical Rating Scale (NRS) score improved from 8 to 0. He could sit and walk without pain. After 1 week, he reported having slight buttock pain with NRS 2 during the follow-up; thus, he received another injection, which improved the NRS to 1. ADL was maintained without recurrence of pain by continuing lifestyle guidance after the second injection. At the time of writing, no relapse has occurred for 4 weeks after the second injection.
PATIENT B:
The patient was a 91-year-old woman who used a walker and lived alone. She had a history of reflux esophagitis, hypothyroidism, and chronic heart failure and oral administration of lansoprazole, levothyroxine, and furosemide, but no history of surgery or allergy. She had been experiencing left buttock pain for a few days before the visit, but without a history of obvious trauma. On the day of the visit, she developed difficulty in walking due to increased buttock pain. She was transported to the Emergency Department of our hospital after an attending physician requested emergency care. Her vital signs during transportation to our hospital were normal. She was carried on a stretcher in the supine position, as even minimal body movements aggravated left buttock pain. Physical examination showed compression of a taut band by the left piriformis muscle and reproducible tenderness at a point in the same region. FAIR test results were positive, and ultrasonography of the left piriformis muscle with internal or external rotation of the left hip joint in the prone position showed reduced piriformis muscle sliding compared with the right piriformis muscle due to adhesions. Therefore, she was diagnosed with PS due to piriformis muscle adhesions related to MPS, and hydro-dissection of the superficial and deep surfaces of the left piriformis muscle was performed, as in the other patient. After injection, the buttock pain rapidly resolved, and she could stand up from the supine position. She hesitated to sit because the buttock pain worsened. NRS improved from 9 to 4. However, she was still unable to walk and was then admitted to the Department of Emergency and General Internal Medicine at our hospital for rehabilitation purposes. After admission, her ADL status gradually improved through physiotherapy. However, she received an injection into the left piriformis muscle the next day due to persistent left buttock pain during walking 3 days after admission, which led to an NRS improvement from 2 to 0. Thereafter, she could walk without pain, but still with the aid of a walker. The patient was discharged 5 days after admission; however, the pain-free period after discharge is unknown because the attending physician continued to treat the patient thereafter.
Discussion
Both patients exhibited all 4 defining symptoms of PS, which were consistent with a diagnosis of PS. Patient B, who had more severe symptoms than patient A, required in-hospital treatment and a longer waiting period for symptom improvement. However, in both patients, the injection of a very low concentration of local anesthetic released pressure on the sciatic nerve, which eventually subsided and allowed the patients to completely return to their previous ADL status. To the best of our knowledge, this is the first report of patients with PS successfully treated by injection of a very low concentration of local anesthetic.
The injection used in this study mostly consisted of saline (ie, a low concentration of local anesthetic diluted in saline). In both patients, the pathology of PS may have been due to myofascial adhesions related to MPS of the piriformis muscle. MPS is characterized by trigger points, and a close relationship between trigger points and fascial adhesions has been reported [20–23]. In addition to subsequent decompression of the piriformis muscle and the tissue around the sciatic nerve running close to the piriformis muscle, the performance of hydro-dissection to release myofascial adhesions may have contributed to the treatment success. The piriformis muscle affects the external rotation of the hip joint; therefore, ultrasonography of the bilateral piriformis muscles with internal or external rotation of the hip joint allows the assessment of piriformis muscle sliding and the presence or absence of adhesions [24]. In addition, treatment with an injection of saline alone is not covered by health insurance in Japan; hence, the injection solution used in this study was a local anesthetic diluted with saline. Nevertheless, injection of saline alone may be used as treatment for PS, as both patients immediately responded to the injection used in this study, which may indicate that the injection led to the quick release of adhesions and decompression. The effectiveness of hydro-dissection for fascial adhesions and entrapment neuropathy has recently gained attention, with reported successful use for carpal tunnel syndrome and hamstring injury [25–27]. Similarly, there are some case reports on the pain-relieving effects of an injection of a mixed saline solution (with saline as a major component) with no significant drug effect. Hydro-dissection with a very low concentration of local anesthetic injection may be additionally useful for clarifying the anatomical mechanism of pain, since its effectiveness may be linked to its cause: fascial adhesions and entrapment neuropathy. Hydro-dissection with a very low concentration of local anesthetic injection should be actively used for patients with confirmed muscle compression of the taut band, suspected myofascial pain, and reduced muscle sliding detected by ultrasonography.
Previously reported adverse effects include local anesthetic intoxication [28], infection and muscle atrophy after steroid injection [29,30], and weakness and pain after botulinum toxin injection [31]. However, the solution used mostly consisted of saline, which may have lower risk of the previously mentioned adverse effects. Furthermore, steroid injection should be administered at appropriate intervals, while the injection solution used in the present cases allows repeated injections within a short time period.
Compared with blind landmark-guided injection, ultrasound-guided injection, which was performed in this study, is safer because it allows accurate injection into the superficial and deep layers of the piriformis muscle and is associated with a lower risk of puncture of the sciatic nerve around the piriformis muscle, inferior gluteal artery, and inferior gluteal vein [32], while reducing the adverse effects of injection-induced neuropathy [33].
This case series report has some limitations. First, only 2 cases were reported; therefore, future studies with larger sample sizes should examine the therapeutic effects of very low-concentration local anesthetic injections. Second, the follow-up period was too short to identify the causes of PS and provide adequate lifestyle guidance. In addition, as a previous study reported a higher risk of recurrence within a few months after injection therapy [34], future studies with a longer follow-up period should evaluate the recurrence rate of PS. Last, there was no comparison with patients receiving other injection solutions to distinguish the advantages and disadvantages of our method in comparison to others.
Conclusions
Hydro-dissection by ultrasound-guided injection of a very low concentration of local anesthetic is effective and has lower risk of adverse effects, thus making it more convenient for the treatment of piriformis syndrome than conventional treatment methods, such as local anesthetic, steroids, and botulinum toxin injection.
References:
1.. Yeoman W, The relation of arthritis of the sacroiliac joint to sciatica, with an analysis of 100 cases: Lancet, 1928; 2; 1119-22
2.. Robinson DR, Pyriformis syndrome in relation to sciatic pain: Am J Surg, 1947; 73; 355-58
3.. Papadopoulos EC, Khan SN, Piriformis syndrome and low back pain: A new classification and review of the literature: Orthop Clin North Am, 2004; 35; 65-71
4.. Pace JB, Nagle D, Piriform syndrome: West J Med, 1976; 124; 435-39
5.. Vij N, Kiernan H, Bisht R, Surgical and non-surgical treatment options for piriformis syndrome: A literature review: Anesth Pain Med, 2021; 11; e112825
6.. Boyajian-O’Neill LA, McClain RL, Coleman MK, Thomas PP, Diagnosis and management of piriformis syndrome: an osteopathic approach: J Am Osteopath Assoc, 2008; 108; 657-64
7.. Natsis K, Totlis T, Konstantinidis GA, Anatomical variations between the sciatic nerve and the piriformis muscle: A contribution to surgical anatomy in piriformis syndrome: Surg Radiol Anat, 2014; 36; 273-80
8.. Robinson DR, Pyriformis syndrome in relation to sciatic pain: Am J Surg, 1947; 73; 355-58
9.. Russell JM, Kransdorf MJ, Bancroft LW, Magnetic resonance imaging of the sacral plexus and piriformis muscles: Skeletal Radiol, 2008; 37; 709-13
10.. Fishman LM, Anderson C, Rosner B, BOTOX and physical therapy in the treatment of piriformis syndrome: Am J Phys Med Rehabil, 2002; 81; 936-42
11.. Shah SS, Consuegra JM, Subhawong TK, Epidemiology and etiology of secondary piriformis syndrome: A single-institution retrospective study: J Clin Neurosci, 2019; 59; 209-12
12.. Benson ER, Schutzer SF, Posttraumatic piriformis syndrome: Diagnosis and results of operative treatment: J Bone Joint Surg Am, 1999; 81; 941-49
13.. Haghnegahdar A, Sedighi M, Motalebi H, Piriformis muscle syndrome: A recurrent case after surgical release: J Surg Case Rep, 2015; 2015; rjv105
14.. Hopayian K, Danielyan A, Four symptoms define the piriformis syndrome: An updated systematic review of its clinical features: Eur J Orthop Surg Traumatol, 2018; 28; 155-64
15.. Fishman LM, Schaefer MP, The piriformis syndrome is underdiagnosed: Muscle Nerve, 2003; 28; 646-49
16.. Chaitow L: Soft tissue manipulation: A practitioner’s guide to the diagnosis and treatment of soft-tissue dysfunction and reflex activity, 1988, Rochester, Vt, Healing Arts Press
17.. Fahmi A, Rahmadhan MA, Aprianto DR, Complete resolution of recurrent piriformis syndrome after piriformis resection with 3 years’ follow up: A case report: Int J Surg Case Rep, 2020; 77; 576-79
18.. Probst D, Stout A, Hunt D, Piriformis syndrome: A narrative review of the anatomy, diagnosis, and treatment: PM R, 2019; 11(Suppl. 1); S54-S63
19.. Bardowski EA, Byrd JWT, Piriformis injection: An ultrasound-guided technique: Arthrosc Tech, 2019; 8; e1457-e61
20.. Gerwin RD, Diagnosis of myofascial pain syndrome: Phys Med Rehabil Clin N Am, 2014; 25; 341-55
21.. Shah JP, Thaker N, Heimur J, Myofascial trigger points then and now: A historical and scientific perspective: PM R, 2015; 7; 746-61
22.. Stecco A, Gesi M, Stecco C, Stern R, Fascial components of the myofascial pain syndrome: Curr Pain Headache Rep, 2013; 17; 352
23.. Stecco C, Stern R, Porzionato A, Hyaluronan within fascia in the etiology of myofascial pain: Surg Radiol Anat, 2011; 33; 891-96
24.. Battaglia PJ, Mattox R, Haun DW, Dynamic ultrasonography of the deep external rotator musculature of the hip: A descriptive study: PM R, 2016; 8; 640-50
25.. Lam KHS, Hung CY, Chiang YP, Ultrasound-guided nerve hydrodissection for pain management: Rationale, methods, current literature, and theoretical mechanisms: J Pain Res, 2020; 13; 1957-68
26.. Courseault J, Kessler E, Moran A, Labbe A, Fascial hydrodissection for chronic hamstring injury: Curr Sports Med Rep, 2019; 18; 416-20
27.. Wu YT, Chen SR, Li TY, Nerve hydrodissection for carpal tunnel syndrome: A prospective, randomized, double-blind, controlled trial: Muscle Nerve, 2019; 59; 174-80
28.. Gitman M, Fettiplace MR, Weinberg GL, Local anesthetic systemic toxicity: A narrative literature review and clinical update on prevention, diagnosis, and management: Plast Reconstr Surg, 2019; 144; 783-95
29.. Stout A, Friedly J, Standaert CJ, Systemic Absorption and side effects of locally injected glucocorticoids: PM R, 2019; 11; 409-19
30.. Fry CS, Nayeem SZ, Dillon EL, Glucocorticoids increase skeletal muscle NF-κB inducing kinase (NIK): Links to muscle atrophy: Physiol Rep, 2016; 4; e13014
31.. Yiannakopoulou E, Serious and long-term adverse events associated with the therapeutic and cosmetic use of botulinum toxin: Pharmacology, 2015; 95; 65-69
32.. Dillow JM, Rosett RL, Petersen TR, Ultrasound-guided parasacral approach to the sciatic nerve block in children: Paediatr Anaesth, 2013; 23; 1042-47
33.. Greensmith JE, Murray WB, Complications of regional anesthesia: Curr Opin Anaesthesiol, 2006; 19; 531-37
34.. Filler AG, Haynes J, Jordan SE, Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment: J Neurosurg Spine, 2005; 2; 99-115
Errate
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943420
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








