21 June 2022: Articles 
Primary Central Nervous System Burkitt Lymphoma, Presenting with Long-Term Fluctuating Level of Consciousness: A Case Report and Literature Review on Challenges in Diagnosis and Management
Challenging differential diagnosis, Rare disease
Salem M. Bahashwan12ABCEF*, Osman O. RadhwiDOI: 10.12659/AJCR.936401
Am J Case Rep 2022; 23:e936401
Abstract
BACKGROUND: Burkitt lymphoma (BL) is an aggressive subtype of B-cell non-Hodgkin lymphoma (NHL) rarely affecting the central nervous system (CNS) as a primary disease. Over the past years, only a few cases of primary CNS Burkitt lymphoma were reported. There is a challenge in early recognition and diagnosis of this type of brain lymphoma. Furthermore, there is no specific treatment protocols for primary CNS Burkitt lymphoma, which adds to the difficulty in managing those patients. We introduce a case of a 65-year-old who presented with fluctuating memory disturbance diagnosed as cerebral Burkitt lymphoma.
CASE REPORT: A 65-year-old man developed a gradual decrease in his level of consciousness over a span of 4 days, associated with fluctuating memory disturbances. A CT scan showed a hyperdense mass in the region of the trigon of the left lateral ventricle and marked obstructive hydrocephalus involving the temporal, occipital horns, and the left lateral ventricle, with no evidence of other suspicious lesions. A brain biopsy of the lesion revealed features of encephalitis initially, but the patient presented later with worsening symptoms, and a repeated brain biopsy showed features of Burkett lymphoma, with normal pan-CT scan.
CONCLUSIONS: Primary CNS Burkitt lymphoma (PCNSBL) is a rare disease with no clear evidence in the literature of how to deal with it. Reporting such cases provides a better understanding of how to approach such unusual presentations. Treatment of PCNSBL is challenging and even with the currently adopted approaches, the disease still has a very poor outcome.
Keywords: Burkitt Lymphoma, Central Nervous System Neoplasms, chemoradiotherapy, Aged, Biopsy, Central Nervous System, Consciousness, Humans, Male, Tomography, X-Ray Computed
Background
Primary central nervous system lymphoma (PCNSL) is a rare form of aggressive extranodal non-Hodgkin lymphoma (NHL), representing only 2% to 3% of all cases [1]. PCNSL usually presents in elderly patients with an average age of 65 years [2]. It is usually of a diffuse large B-cell type that arises in the brain, leptomeninges, eyes, or spinal cord in the absence of systemic involvement [3]. PCNSLs subgroups include diffuse large B-cell lymphoma (DLBCL) (which is the more common subtype), Burkitt lymphoma, and T cell lymphomas [1,3–5].
Burkitt lymphoma is an aggressive subtype of B-cell NHL rarely affecting the central nervous system (CNS) as a primary disease [6–22], and can be distinguished from DLBCL by histo-pathology and immunohistochemistry, which is characterized by CD10+/bc-2-/bcl-6+ with a high Ki-67 proliferation index, and may show Epstein-Barr virus-encoded messenger RNA (EBER) and fluorescence in situ hybridization (FISH), and has the starry-sky appearance in some, but not all, cases, which is due to the presence of macrophages with relatively clear cytoplasm [23]. Over the past years, only a few cases of Burkitt lymphoma were reported as a primary disease affecting the CNS in both adults and children [6–33]. Unfortunately, there is a challenge in early recognition and diagnosis of such type of brain lymphoma, resulting in a delay in treatment and therefore, a poor prognosis [34]. Furthermore, there is no specific treatment protocol for primary CNS Burkitt lymphoma, which adds to the difficulty in managing those patients [35]. Here, we present a case of a 65-year-old man with primary CNS Burkitt lymphoma at the region of the trigone of the left lateral ventricle abutting the splenium of the corpus callosum. We also discuss the details of diagnosis and treatment approaches in this patient which included high-dose methotrexate and a ventriculoperitoneal (VP) shunt. In addition, a literature review is written to compare this case of PCNSBL to other similar case reports regarding treatment options and overall response to treatment in those patients.
Case Report
A 65-year-old-man, known to have diabetes mellitus and benign prostatic hyperplasia, developed a gradual decrease in his level of consciousness over a span of 4 days, associated with fluctuating memory disturbances that started 1 month prior to presentation. There was no associated headache, fever, abnormal movements, night sweating or weight loss. The patient was vitally stable on presentation with normal blood pressure, heart rate, temperature, and oxygen saturation; however, his Glasgow coma scale (GCS) was 13/15 due to eye opening only to verbal command and confusion; the other aspects of his neurological examination were normal.
He was started on 4 mg of dexamethasone every 4 hours empirically and showed significant improvement in term of level of consciousness, and he regained fully his neurological functions with GCS 15/15. Dexamethasone was then tapered and completely stopped after a course of 10 days.
A CT scan of the brain showed a hyperdense mass in the region of the trigon of the left lateral ventricle and marked obstructive hydrocephalus involving the temporal and occipital horns, and the left lateral ventricle.
CT scans of the cervical, abdominal, pelvic, and thoracic regions did not show any evidence of metastatic disease.
Cytologic examination of the cerebrospinal fluid (CSF) showed no abnormal cells, glucose level in CSF was 3.6 mmol/l (normal range 2.8–4.4 mmol/l), and protein level in CSF was 2.03 g/l (normal range 0.15–0.6 g/l).
A couple of months later, the patient presented again with similar signs and symptoms with fluctuating level of consciousness, and his GCS was 13/15.
A magnetic resonance imaging (MRI) of the brain showed an interval increase in the left lateral ventricle lesion with development of mild diffuse dural enhancement (Figure 1A–1F).
A mini-craniotomy and a biopsy of the previously descried brain lesion was done; the pathology report revealed features of encephalitis and no evidence of malignancy.
Dexamethasone was started then tapered slowly, this improved the patient’s symptoms and confusion, and he was discharged and given an appointment to follow up as an out-patient while waiting for the biopsy results.
The patient presented again a few weeks later with decreased level of consciousness, GCS 13/15, with no constitutional or other neurological signs and symptoms.
A repeated CT scan of the brain showed left supratentorial hydrocephalus with an interval increase in size of the left intraventricular lesion which at this point measured 3.3×1.3 cm. A craniotomy and an excisional biopsy of the left ventricular lesion was done.
The histopathology report this time showed a diffuse infiltrate of lymphocytes with a starry-sky appearance at low power. The lymphocytes infiltrate was composed of sheets of monotonous, medium-sized lymphocytes with squares off borders, round nuclei, finely clumped chromatin, and several paracentral nucleoli. Numerous tangible macrophages, apoptotic bodies, and mitoses were also seen, all of which are features of Burkitt lymphoma (Figure 2A–2F). A panel of immunohisto-chemical stains showed sheets of CD20-positive B-cells that coexpress CD10 and BCL6, and negative for BCL2. Proliferation index by Ki67 was approximately 100%. C-MYC rearrangement was detected by FISH studies. All of these histopathological, immunohistochemical, and molecular findings were indicative of a Burkitt lymphoma. A bone marrow biopsy showed no evidence of involvement by lymphoma, and pan-CT scans did not show any other lesions.
A ventriculoperitoneal (VP) shunt was inserted, and corticosteroids were started immediately after surgery, which improved the patient’s level of consciousness.
A repeat lumbar puncture (LP) showed a glucose level of 2.8 mmol/l (2.8–4.4 mmol/l), protein level of 6.65 g/l (0.15–0.6 g/l), and no abnormal cells. Viral and bacterial cultures were negative.
A bone marrow biopsy showed no evidence of involvement by lymphoma, and pan-CT scans did not show any other lesions.
At this point, chemoimmunotherapy (rituximab, vincristine, and high-dose methotrexate) was started. On day 1, the patient received rituximab (375 mg/m2) followed by high-dose methotrexate (3.5 g/m2) and vincristine (total dose of 2 g) on day 2.
The patient showed excellent tolerance to treatment and complete clinical neurological response was noted at day 3 where the GCS was 15/15.
A Brain CT scan on day 10 of treatment showed improvement of the left cerebral hemispheric edema, the midline shift, and no interval development of new lesions.
The laboratory investigations on day 12 of treatment showed that patient started to have neutropenia, and his CBC revealed white blood cells count (WBC) of 1.12 K/uL (4–10 K/uL), neutrophil count of 0.45 K/uL (2.5–7 K/uL), hemoglobin of 8.5 g/dl (13–16.5 g/dl), and platelets count of 157 K/uL (150–450 K/uL).
On day 18 of treatment, the patient developed febrile neutropenia with a temperature of 38.9°C and a neutrophil count of 0.4 g/l. Empirical antibiotic treatment was started initially using Piperacillin/Tazobactam (Tazocin) followed by Meropenem and Vancomycin; however, the patient was transferred to the intensive care unit due to septic shock. Blood cultures later came back positive for a multi-resistant
Discussion
Burkett lymphoma is a very aggressive subtype of NHL which rarely presents as a primary central nervous system disease and is usually associated with a poor outcome [34]. Initial symptoms and clinical signs of PCNSBL are sometimes difficult to recognize, and can be associated with long-term and fluctuating symptoms as seen in this case, hindering early diagnosis and treatment [34]. And since only a limited number of cases are reported in the literature, not enough information is available regarding different clinical presentations, diagnosis, and treatment modalities.
The sensitivity of CSF cytology is variable but is generally low (2–32%) [36]. This can be a result of low fluid volume, delays in processing, or the patient’s exposure to corticosteroids prior to obtaining the specimen [36]. The yield of cytology specimens can be improved when serial samples are sent to the pathology lab and with the aid of immunohistochemistry and flow cytometry studies are performed if there is enough fluid volume [36].
Due to the above-mentioned reasons, a tissue biopsy for diagnosis is often needed. Central nervous system biopsies present a diagnostic challenge, especially when it comes to diagnosing lymphoma, because many times, the tissue is scant; therefore, preventing the use of an elaborate panel of immunohistochemical stain. Furthermore, many times, primary CNS Burkitt lymphomas are extensively necrotic, making biopsy interpretation even more challenging. Repeated tissue biopsy is sometimes needed to get a definitive diagnosis, as shown in our case, and other factors like steroid therapy can affect the quality of the biopsy. Lastly, biopsies may not be representative of the disease process if only the edges of the lesion are sampled, especially in deeper-seated lesions that are difficult to reach.
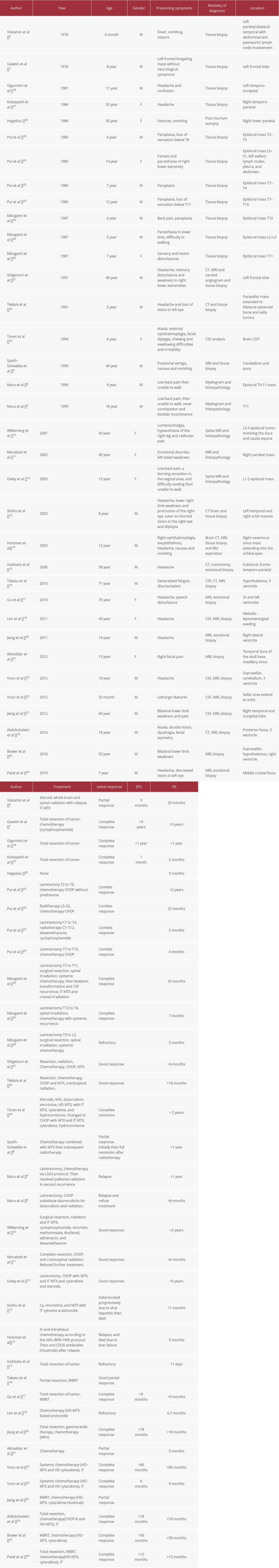
Multiple approaches have been used to treat PCNSBL in the literature (Table 1). Taking into consideration the rarity of this subtype and the lack of treatment guidelines [35], the treatment recommendations of PCNSL were followed in most of the reported cases, but even with these adopted modalities, the overall outcome was still unfavorable.
In the literature, patients with PCNSBL were mainly treated with high-dose methotrexate-based regimens (HD-MTX), either alone or in combination with surgery, radiotherapy, systemic and/or intrathecal (IT) chemotherapy.
Except for high-dose methotrexate therapy, most other therapeutic modalities are controversial, especially intrathecal chemotherapy and whole-brain radiotherapy (WBRT) [16].
Although most of the international guidelines and review articles discourage total surgical resection of PCNSL due to the infiltrative behavior, multifocality of the tumor, and the elevated risk of post-operative complications [37–39], some studies recommend and adopt such an approach and state that aggressive resection of PCNSL correlated with better progression-free survival (PFS) and overall survival (OS) compared to biopsy without total resection of the tumor [37,40].
Based on these data, total resection of tumor in PCNSBL could be beneficial in selected cases, in addition to the other treatment modalities, especially when the tumor is solitary and not deeply infiltrating the brain.
As there is no specific guideline in treating PCNSBL, and most of the reported cases of PCNSBL were treated according to the guidelines of PCNSL, the current recommendations in treatment of PCNSL put chemotherapy as the first line of treatment, either alone or in combination with radiotherapy [41]. HD-MTX remains the best single agent effective in treating these tumors as it effectively penetrates the blood brain barrier [42]. Another effective single agent is HD-Cytarabine; the combination of this agent with HD-MTX and WBRT has shown better complete remission rate and overall response rate compared to HD-MTX and WBRT alone (46% and 69% vs 18% and 40%, respectively [43].
WBRT alone does not produce remission; however, it is considered an additional approach to other modalities [44]. Most of the studies do not recommend WBRT due to the risk of neurotoxicity, especially in the elderly population [44–46]. In a phase III randomized trial, the addition of WBRT to those patients who were in complete remission (CR) after methotrexate-based chemotherapy showed no statistically significant improvement in OS [47]. In those who achieved partial response after methotrexate-based chemotherapy, the addition of WBRT revealed a benefit in term of PFS (
IT chemotherapy is usually not recommended in the treatment of PCNSL, as it only increases toxicity, with minimal to no survival benefits when added to i.v. chemotherapy [47,48].
Conclusions
PCNSBL is a rare entity of brain lymphomas that affects elderly individuals, which makes its diagnosis and treatment challenging, and most of the cases of PCNSBL reported in the literature were following the treatment recommendations of PCNSL. Reporting these cases enriches the literature and provides a better understanding on how to approach and treat those patients with PCNSBL. Treatment of PCNSBL is challenging and even with the available options and current adopted approaches, the disease still has a very poor outcome.
Figures
References:
1.. Villano JL, Koshy M, Shaikh H, Age, gender, and racial differences in incidence and survival in primary CNS lymphoma: Br J Cancer, 2011; 105(9); 1414-18
2.. Abla O, Weitzman S, Primary central nervous system lymphoma in children: Neurosurg Focus, 2006; 21(5); E8
3.. Hochberg FH, Miller DC, Primary central nervous system lymphoma: J Neurosurg, 1988; 68(6); 835-53
4.. Batchelor T, Loeffler JS, Primary CNS lymphoma: J Clin Oncol, 2006; 24(8); 1281-88
5.. Citterio G, Reni M, Gatta G, Ferreri AJM, Primary central nervous system lymphoma: Crit Rev Oncol Hematol, 2017; 113; 97-110
6.. Valsamis MP, Levine PH, Rapin I, Primary intracranial Burkitt’s lymphoma in an infant: Cancer, 1976; 37(3); 1500-7
7.. Gawish HHA, Primary Burkitt’s lymphoma of the frontal bone: Case report: J Neurosurg, 1976; 45(6); 712-15
8.. Takasu M, Takeshita S, Tanitame N, Primary hypothalamic third ventriclular Burkitt’s lymphoma: A case report with emphasis on differential diagnosis: Br J Radiol, 2010; 83(986); e043
9.. Gu Y, Hou YY, Zhang XB, Hu F, Primary central nervous system Burkitt lymphoma as concomitant lesions in the third and the left ventricles: A case study and literature review: J Neurooncol, 2010; 99(2); 277-81
10.. Giromini D, Peiffer J, Tzonos T, Occurrence of a primary Burkitt-type lymphoma of the central nervous system in an astrocytoma patient: A case report. Acta Neuropathol, 1981; 54(2); 165-67
11.. Lim T, Kim SJ, Kim K, Primary CNS lymphoma other than DLBCL: A descriptive analysis of clinical features and treatment outcomes: Ann Hematol, 2011; 90(12); 1391-98
12.. Jiang M, Zhu J, Guan YS, Zou LQ, Primary central nervous system Burkitt lymphoma with non-immunoglobulin heavy chain translocation in right ventricle: Case report: Pediatr Hematol Oncol, 2011; 28(5); 454-58
13.. Akhaddar A, Zalagh M, Belfquih H, Boucetta M, Burkitt’s lymphoma: A rare cause of isolated trigeminal neuralgia in a child: Childs Nerv Syst, 2012; 28(7); 1125-26
14.. Yoon JH, Kang HJ, Kim H, Successful treatment of primary central nervous system lymphoma without irradiation in children: Single center experience: J Korean Med Sci, 2012; 27(11); 1378-84
15.. Jiang L, Li Z, Finn LE, Primary central nervous system B cell lymphoma with features intermediate between diffuse large B cell lymphoma and burkitt lymphoma: Int J Clin Exp Pathol, 2012; 5(1); 72-76
16.. Alabdulsalam A, Zaidi SZA, Tailor I, Primary Burkitt lymphoma of the fourth ventricle in an immunocompetent young patient: Case Rep Pathol, 2014; 2014; 630954
17.. Bower K, Shah N, Primary CNS Burkitt lymphoma: A case report of a 55-year-old cerebral palsy patient: Case Rep Oncol Med, 2018; 2018; 5869135
18.. Späth-Schwalbe E, Genvresse I, Stein H, [Highly malignant primary Burkitt-type B-cell lymphoma.]: Dtsch Medizinische Wochenschrift, 1999; 124(15); 451-55 [In German]
19.. Patel P, Anand A, Parikh S, Primary central nervous system Burkitt lymphoma in HIV positive pediatric patient: a rare case report: J Pediatr Neurosci, 2019; 14(2); 86-89
20.. Kobayashi H, Sano T, Li K, Hizawa K, Primary Burkitt-type lymphoma of the central nervous system: Acta Neuropathol, 1984; 64(1); 12-14
21.. , An unusual mixed form of two intracranial primary malignant lymphomas – ScienceDirect Accessed December, 3, 2021https://www.sciencedirect.com/science/article/abs/pii/0090301984903951
22.. Pui CH, Dahl GV, Hustu HO, Murphy SB, Epidural spinal cord compression as the initial finding in childhood acute leukemia and non-Hodgkin lymphoma: J Pediatr, 1985; 106(5); 788-92
23.. Chuang SS, Ye H, Du MQ, Histopathology and immunohistochemistry in distinguishing Burkitt lymphoma from diffuse large B-cell lymphoma with very high proliferation index and with or without a starry-sky pattern: A comparative study with EBER and FISH: Am J Clin Pathol, 2007; 128(4); 558-64
23.. Mizugami T, Mikata A, Hajikano H, Primary spinal epidural Burkitt’s lymphoma: Surg Neurol, 1987; 28(2); 158-62
24.. , (4) Multiple brain tumors of different cell types with an unruptured cerebral aneurysm – Case report Accessed December 3, 2021https://www.researchgate.net/publication/21440827_Multiple_brain_tumors_of_different_cell_types_with_an_unruptured_cerebral_aneurysm_-_Case_report
25.. Tekkök IH, Tahta K, Erbengi A, Primary intracranial extradural Burkitt-type lymphoma. A unique presentation with unilateral loss of vision in a child: Childs Nerv Syst, 1991; 7(3); 172-74
26.. Toren A, Mandel M, Shahar E, Primary central nervous system Burkitt’s lymphoma presenting as Guillain-Barré syndrome: Med Pediatr Oncol, 1994; 23(4); 372-75
27.. Mora J, Wollner N, Primary epidural non-Hodgkin lymphoma: Spinal cord compression syndrome as the initial form of presentation in childhood non-Hodgkin lymphoma: Med Pediatr Oncol, 1999; 32(2); 102-5
28.. Wilkening A, Brack M, Brandis A, Unusual presentation of a primary spinal Burkitt’s lymphoma: J Neurol Neurosurg Psychiatry, 2001; 70(6); 794-97
29.. Monabati A, Rakei SM, Kumar PV, Primary burkitt lymphoma of the brain in an immunocompetent patient: Case report. J Neurosurg, 2002; 96(6); 1127-29
30.. Daley MF, Partington MD, Kadan-Lottick N, Odom LF, Primary epidural Burkitt lymphoma in a child: Case presentation and literature review: Pediatr Hematol Oncol, 2003; 20(4); 333-38
31.. Shehu BB, Primary central nervous system Burkitt’s lymphoma presenting with proptosis: Ann Trop Paediatr, 2003; 23(4); 319-20
32.. Huisman TAGM, Tschirch F, Schneider JFL, Burkitt’s lymphoma with bilateral cavernous sinus and mediastinal involvement in a child: Pediatr Radiol, 2003; 33(10); 719-21
33.. Gobbato PL, Pereira Filho ADA, De David G, Primary meningeal Burkitt-type lymphoma presenting as the first clinical manifestation of acquired immunodeficiency syndrome: Arq Neuropsiquiatr, 2006; 64(2B); 511-15
34.. Baehring JM, Batchelor TT, Diagnosis and management of neurolymphomatosis: Cancer J (United States), 2012; 18(5); 463-68
35.. Grommes C, DeAngelis LM, Primary CNS lymphoma: J Clin Oncol, 2017; 35(21); 2410-18
36.. Scott BJ, Douglas VC, Tihan T, A systematic approach to the diagnosis of suspected central nervous system lymphoma: JAMA Neurol, 2013; 70(3); 311-19
37.. Weller M, Martus P, Roth P, Surgery for primary CNS lymphoma? Challenging a paradigm: Neuro Oncol, 2012; 14(12); 1481-84
38.. Deangelis LM, Yahalom J, Heinemann MH, Primary CNS lymphoma: Combined treatment with chemotherapy and radiotherapy: Neurology, 1990; 40(1); 80-86
39.. Bataille B, Delwail V, Menet E, Primary intracerebral malignant lymphoma: Report of 248 cases: J Neurosurg, 2000; 92(2); 261-66
40.. Bellinzona M, Roser F, Ostertag H, Surgical removal of primary central nervous system lymphomas (PCNSL) presenting as space occupying lesions: A series of 33 cases: Eur J Surg Oncol, 2005; 31(1); 100-5
41.. DeAngelis LM, Primary central nervous system lymphoma: Curr Opin Neurol, 1999; 12(6); 687-91
42.. Batchelor T, Carson K, O’Neill A, Treatment of primary CNS lymphoma with methotrexate and deferred radiotherapy: A report of NABTT 96-07: J Clin Oncol, 2003; 21(6); 1044-49
43.. Ferreri AJ, Reni M, Foppoli M, High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: A randomised phase 2 trial: Lancet (London, England), 2009; 374(9700); 1512-20
44.. Batchelor T, Loeffler JS, Primary CNS lymphoma: J Clin Oncol, 2006; 24(8); 1281-88
45.. DeAngelis LM, Seiferheld W, Clifford Schold S, Combination chemotherapy and radiotherapy for primary central nervous system lymphoma: Radiation Therapy Oncology Group Study 93–10: J Clin Oncol, 2002; 20(24); 4643-48
46.. Reni M, Ferreri AJM, Guha-Thakurta N, Clinical relevance of consolidation radiotherapy and other main therapeutic issues in primary central nervous system lymphomas treated with upfront high-dose methotrexate: Int J Radiat Oncol Biol Phys, 2001; 51(2); 419-25
47.. Korfel A, Thiel E, Martus P, Randomized phase III study of whole-brain radiotherapy for primary CNS lymphoma: Neurology, 2015; 84(12); 1242-48
48.. Ferreri AJM, Reni M, Pasini F, A multicenter study of treatment of primary CNS lymphoma: Neurology, 2002; 58(10); 1513-20
Figures
Tables
In Press
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942824
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943118
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942826
14 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942770
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250