16 September 2022: Articles 
A Pituitary Abscess Caused by : A Case Report
Challenging differential diagnosis, Unusual setting of medical care, Rare disease
Fayez M. AlelyaniDOI: 10.12659/AJCR.936743
Am J Case Rep 2022; 23:e936743
Abstract
BACKGROUND: Pituitary abscess (PA) is a rare pituitary lesion accounting for less than 1% of all pituitary diseases and is associated with high mortality rates. The non-specific clinical symptoms and radiological features preclude accurate diagnosis of the disease. Hence, surgical intervention is still considered the criterion standard method for PA diagnosis. Most PAs occur as a primary disease or due to complications such as surgery, sepsis, and adjacent inflamed lesions.
CASE REPORT: A 53-year-old man presented to the Emergency Department with a headache associated with nausea, vomiting, and constipation. The patient had no visual disturbances, polyuria, polydipsia, nocturia, or abnormal discharges. Computed tomography (CT) and magnetic resonance imaging (MRI) showed a large suprasellar mass. The patient underwent left-side trans-nasal transsphenoidal microscopic surgery for mass removal. An abscess with discharge was noticed and sent for microbiological evaluation, revealing an infection with a commensal enteric bacterium that rarely causes nosocomial infection, known as Morganella morganii. The patient was discharged after completing the intravenous antibiotic course and was given oral antibiotics.
CONCLUSIONS: Pituitary abscess is a rare pituitary lesion. However, taking the history of recent meningitis, sinusitis, and/or surgery may help to reach an early diagnosis, prompt surgical intervention, and vital therapeutic steps to reduce mortality rates and improve patient’s outcomes. PA should always be considered when patients demonstrate signs of pituitary dysfunction associated with signs of infection. Furthermore, antibiotics should be administered immediately once the PA case is confirmed and should last for at least 6 weeks postoperatively.
Keywords: brain abscess, Magnetic Resonance Imaging, Morganella morganii, Pituitary Diseases, Anti-Bacterial Agents, Humans, Male, Middle Aged, Tomography, X-Ray Computed
Background
This report is about a 53-year-old man who presented to the Emergency Department at King Fahad General Hospital, Madinah, Saudi Arabia, with a headache associated with nausea and vomiting for the last 3 days.
A pituitary abscess (PA) is a rare intracranial mass that accounts for less than 1% of all pituitary diseases and is associated with high mortality rates [1,2]. Simmonds reported the first known case of PA in 1914 [3]. Since then, more than 200 cases have been identified and reported in the literature [4]. PA may occur as a primary disease or through hematogenous spread from other infected or inflamed lesions, such as in sphenoiditis, meningitis, or sinusitis [5–7]. Several PA case reports cited the isolation of pathogens such as Staphylococcus spp. and Streptococcus spp., Moraxella catarrhalis, Mycobacterium tuberculosis, and fungi such as Aspergillus fumigatus [5,6,8,9].
Preoperative diagnosis of PA can be quite complicated, as it can be very difficult to distinguish PA from other pituitary lesions based on clinical and radiological features [10]. Thus, surgical intervention is still considered the most reliable method for PA diagnosis. However, surgical intervention can be associated with drawbacks such as postoperative tissue disruption, carotid artery injuries, and cerebrospinal fluid leakage.
This case report discusses the early diagnosis and therapeutic protocol for such rare lesions.
Case Report
A 53-year-old man presented to the Emergency Department at King Fahad General Hospital, Madinah, Saudi Arabia, with a headache associated with nausea and vomiting for the last 3 days. Based on the patient’s description, his headache started gradually over 2 weeks, with no response to analgesic drugs. The patient reported he had no visual disturbances, polyuria, polydipsia, nocturia, or abnormal discharges, and never had any previous episodes. His vital signs were body temperature 36.8°C, blood pressure 119/72 mmHg, and heart rate 53 bpm.
Upon medical examination, the confrontation visual fields test result was within the normal acceptable range, and the fundos-copy showed bilateral normal fundus, with intact extraocular movement. There were no other complications such as cushingoid or acromegaly features, galactorrhea, or gynecomastia.
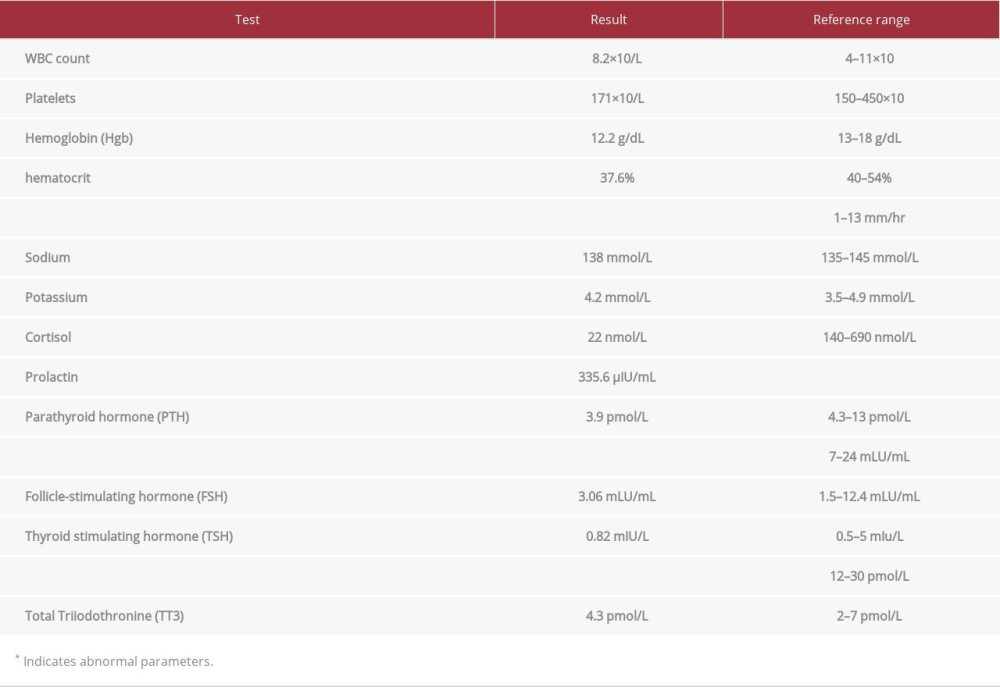
His initial computed tomography (CT) plain scan showed a large suprasellar mass. The CT with contrast showed a suprasellar lesion measuring 1.7×1.5 cm with vivid peripheral enhancement causing expansion of the sellar bone (Figures 1, 2). Multiplanar and multi-sequence magnetic resonance imaging (MRI) of the pituitary without contrast revealed a sellar lesion causing compression and mass effect over the optic chiasm. The lesion demonstrated high signal intensity in the T1-weighted images and heterogeneous low signal intensity in the T2-weighted images (Figure 3), suggesting pituitary macroadenoma with apoplexy. Table 1 shows results of routine laboratory tests performed prior to the initial treatment.
The patient underwent a surgical operation to remove the pituitary macroadenoma through left-side trans-nasal transsphenoidal microscopic surgery. Briefly, the nostril mucosa and sphenoid sinus mucosa were removed, followed by creation of a small dural opening with a size 11 blade to remove the exposed sellar floor. A yellow discharge leaking from the site of the incision was noticed, collected, and sent for microbiological evaluation. To clean the cavity, irrigation with a copious amount of saline was performed, followed by suctioning any remaining pus discharge and washing with 2 g of Vancomycin diluted in 500 ml normal saline. To prevent postoperative cerebrospinal fluid leakage, a fat and fibrin glue product (Tisseel) (Baxter, Austria) was applied to repair and reconstruct the sellar floor. Finally, bilateral nasal packing was applied to the nostrils.
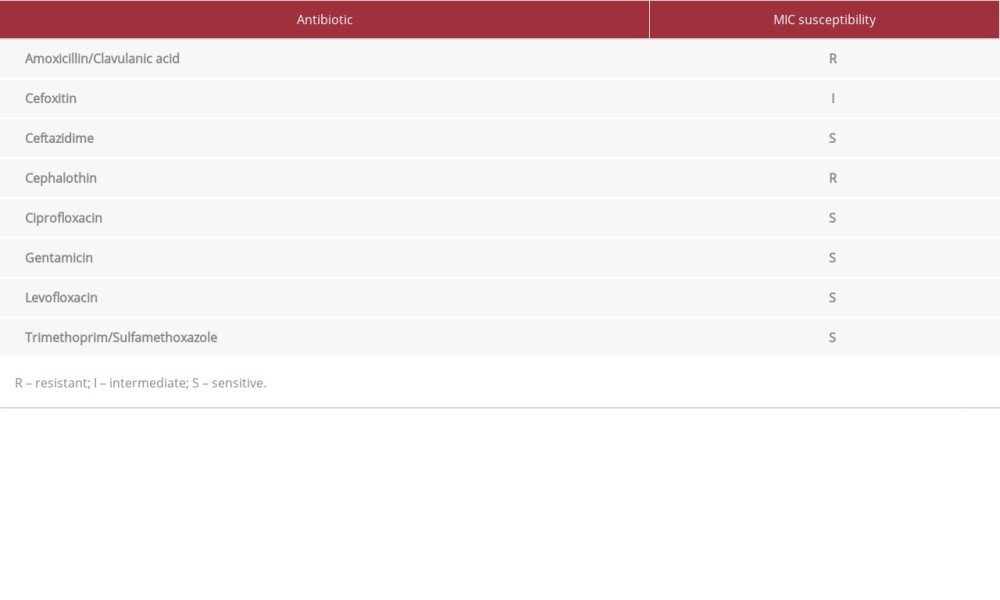
In the microbiology laboratory, the drained abscess specimen showed no microorganisms. However, the specimen showed bacterial colonies after culture for 18-24 h. Identification and susceptibility testing was performed using Vitek 2, revealing
Postoperatively, the patient was admitted to the Intensive Care Unit for 24 h for overnight observation. He was subjected to empirical i.v. antibiotics treatment containing vancomycin (1500 mg), ceftazidime (2 g), and metronidazole (500 mg) every 8 h. After acquiring the bacterial culture and the sensitivity results, vancomycin was discontinued, while ceftazidime and metronidazole were continued for 6 weeks.
At 4-week follow-up, the patient exhibited no symptoms, and the MRI did not reveal any enhanced residual abscess pockets, suggesting a complete resolution (Figures 4, 5). The patient was discharged after completing the intravenous antibiotic course and was given oral antibiotics (metronidazole and ciprofloxacin) for 1 month.
Discussion
PA is an extremely rare clinical condition that occurs as a primary disease or secondary to other remote infected areas such as in sphenoiditis, sinusitis, or meningitis [5–7]. In our case, we suggest that PA was a result of chronic sinusitis complication, which was indicated by operative and radiological findings. A CT scan showed bilateral mucosal thickening of maxillary and ethmoid sinuses, while MRI showed fluid accumulation in the paranasal sinuses. These findings indicate asymptomatic chronic sinusitis, which might explain the pathogenesis of PA in this patient.
Radiological techniques provide limited ability to distinguish PA from other pituitary tumors. However, a study performed by Shimamura et al suggested the high uptake of thallium-210 single-photon emission CT by an abscess provides a useful way to differentiate pituitary lesions [12]. Diffusion-weighted imaging (DWI)/apparent diffusion coefficient (ADC) might have been useful in differentiation, but it was not available. In our case, T1 with contrast showed ring enhancement, which suggests abscess formation, unlike homogeneous enhancement in pituitary tumors, but it is important to note that macroadenomas with the hemorrhagic component can have similar features.
Several pathogens have been isolated from patients with confirmed PA [5,6,8,9]. In our case, the gram-negative bacillus
Conclusions
Although pituitary abscess is a rare pituitary lesion, early diagnosis and a prompt surgical intervention are vital therapeutic steps that can reduce mortality rates and improve patient outcomes. PA should always be considered when patients demonstrate signs of pituitary dysfunction associated with signs of infection. Furthermore, antibiotics should be administered immediately after PA is confirmed and should last for at least 6 weeks postoperatively.
Figures
References:
1.. Dalan R, Leow MK, Pituitary abscess: Our experience with a case and a review of the literature: Pituitary, 2008; 11; 299-306
2.. Liu F, Li G, Yao Y, Diagnosis and management of pituitary abscess: Experiences from 33 cases: Clin Endocrinol (Oxf), 2011; 74; 79-88
3.. Hazra S, Acharyya S, Primary pituitary abscess in an adolescent boy: A rare occurrence: BMJ Case Rep, 2012; 2012; bcr201200713
4.. Sherrod BA, Makarenko S, Iyer RR, Primary pituitary abscess in an adolescent female patient: Case report, literature review, and operative video: Childs Nerv Syst, 2021; 37; 1423-28
5.. Vates GE, Berger MS, Wilson CB, Diagnosis and management of pituitary abscess: A review of twenty-four cases: J Neurosurg, 2001; 95; 233-41
6.. Agyei JO, Lipinski LJ, Leonardo J, Case report of a primary pituitary abscess and systematic literature review of pituitary abscess with a focus on patient outcomes: World Neurosurg, 2017; 101; 76-92
7.. Oka A, Akamatsu M, Kanai K, A case of bacterial sphenoid sinusitis accompanied by a pituitary abscess: Otolaryngology Case Reports, 2022; 23; 100432
8.. Kawano T, Shinojima N, Hanatani S: Surg Neurol Int, 2021; 12; 617
9.. Gotecha S, Chugh A, Punia P, A rare case of primary pituitary tubercular abscess mimicking a pituitary adenoma: Neurol India, 2021; 69; 1414-20
10.. Dutta P, Bhansali A, Singh P, Pituitary abscess: Report of four cases and review of literature: Pituitary, 2006; 9; 267-73
11.. Patil AB, Nadagir SD, Lakshminarayana S, Syeda FM: J Neurosci Rural Pract, 2012; 3; 370-72
12.. Shimamura N, Ogane K, Takahashi T, Pituitary abscess showing high uptake of thallium-201 on single photon emission computed tomography – case report: Neurol Med Chir (Tokyo), 2003; 43; 100-3
13.. Lin TY, Chan MC, Yang YS: Eur J Clin Microbiol Infect Dis, 2015; 34; 231-36
Figures
In Press
06 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942937
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250