25 January 2023: Articles 
Pneumatosis Cystoides Intestinalis: A Case Report
Mistake in diagnosis, Diagnostic / therapeutic accidents, Rare disease, Educational Purpose (only if useful for a systematic review or synthesis)
Yoko Ohata1ABCDEFG, Hiroshi Higuchi2ABCDEFG, Sayaka Ogawa3ABCDEFG, Takashi Watari45ABCDEFG*DOI: 10.12659/AJCR.938207
Am J Case Rep 2023; 24:e938207
Abstract
BACKGROUND: Pneumatosis cystoides intestinalis (PCI) is a rare condition in which cystic gas is found in the submucosal and serosal tissues of the intestinal wall.
CASE REPORT: The patient, an 84-year-old woman, was referred to us because of abdominal distention and diarrhea lasting 2 weeks. On initial physical examination, there was marked abdominal distention without tenderness. Blood tests revealed no abnormalities, but simple abdominal radiographs showed gas in the small intestine. Contrast-enhanced computed tomography showed massive emphysema in the intestinal wall with no signs of portal gas or intestinal ischemia. The patient was diagnosed with PCI, and the prognosis was good. The patient showed improvement when managed with an elimination diet and follow-up.
CONCLUSIONS: Herein, we present the characteristics and diagnosis of PCI because the imaging findings of PCI can appear more severe than the actual condition, causing it to be mistaken for other serious diseases, which leads to unnecessary surgical procedures.
Keywords: Diagnosis, Pneumatosis cystoides intestinalis, Female, Humans, Aged, 80 and over, Tomography, X-Ray Computed, Intestines
Background
Pneumatosis intestinal cysticercosis (PCI) is a rare disease wherein cystic gas is observed in the submucosal or serosal tissue of the intestinal wall. It reportedly occurs at all ages, most commonly at 45±15 years of age. Non-surgical treatment results in remission in 70% of patients [1]. However, PCI is often mistaken for other serious diseases due to the associated “severe” imaging findings, which may lead to unnecessary surgical procedures [2]. Here, we present a case of PCI to illustrate the associated key findings and highlight the importance of differentiating PCI from other diseases.
Case report
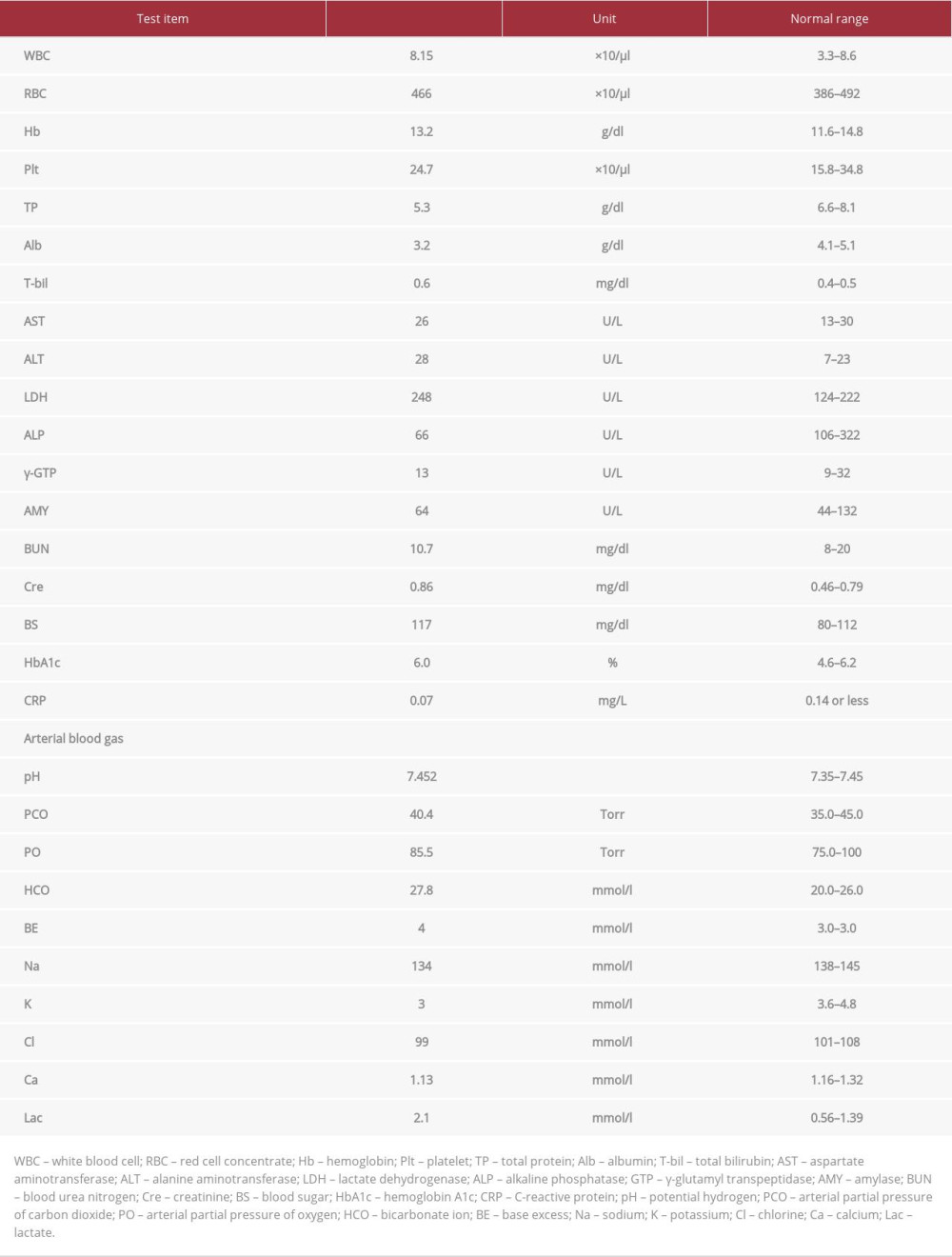
An 84-year-old woman was referred from a rehabilitation hospital to a tertiary care hospital with abdominal distension and diarrhea that had persisted for 2 weeks. She had an altered state of consciousness and was initially unable to speak; therefore, her subjective symptoms were unknown. Her vital signs were within normal ranges. During the initial physical examination, there was marked abdominal distension without perceptible tenderness. The patient’s medical history included dementia, pneumonia, and cerebral infarction. She was taking multiple medications, including prednisone, lansoprazole, and quetiapine. Blood test results (Table 1) showed that her blood urea nitrogen (10.7 mg/dL, normal: 6 to 24 mg/dL) and creatinine (0.86 mg/dL; normal: 0.7 to 1.3 mg/dL) were within normal limits. Blood gas analysis showed a mildly elevated lactate level (2.1 mmol/L, normal: 0.5–1 mmol/L). Simple abdominal radiography showed the presence of gas in the small bowel (Figure 1). Contrast-enhanced computed tomography (CT) showed free air, copious emphysema in the intestinal wall, and no portal gas or signs of intestinal ischemia (Figures 2, 3). After a multidisciplinary consultation involving surgeons, gastroenterologists, and radiologists, the patient was admitted to the hospital with a diagnosis of PCI with a good prognosis. Surgery was determined to be unnecessary, and the patient was managed with fasting and oral fluids. Oxygen was administered to reduce intestinal emphysema. As there were no signs of infection, no antimicrobials were administered. Three days later, a CT scan revealed that the abdominal distension and intestinal gas had decreased; therefore, oxygen administration was terminated, and food intake was initiated. On day 11 after admission, the patient’s abdominal symptoms improved, and she was discharged.
Discussion
PCI occurs in individuals 50 to 80 years of age, and its incidence is approximately 0.03% [3]. The cause is unknown, but it may involve multiple factors, including mechanical, biochemical, bacterial, and pulmonary disease-related influences [3]. In such cases, the differential diagnosis of other severe gastrointestinal diseases, such as intestinal ischemia, infarction, necrotizing enterocolitis, intestinal perforation, axial torsion, and sepsis, should be excluded by performing blood tests and imaging studies [4]. Table 2 shows the poor prognostic factors associated with PCI. Indicators for surgery include age over 60 years, vomiting, and a white blood cell count >12 000/μL [5].
Although PCI generally has a good prognosis, accurate diagnosis and timely surgery are important. Poor prognostic factors have been proposed, including intrahepatic portal gas, changes in blood test values, and negative predictors such as a pH <7.3, HCO3– level <20 mmol/L, and lactate level >2 mmol/L [6–8]. Despite the patient being elderly, she had normal vital signs and no subjective symptoms except lactate levels; therefore, surgery was not indicated for the patient. There were no findings of wall contrast failure or torsion indicative of intestinal ischemia on CT findings. Based on the diagnostic flowchart for PCI, the vascular risk score was 0 in STEP3 [9] (Figure 4). Therefore, the patient was monitored with follow-ups and imaging tests. The sensitivity and negative predictive value in STEP3 were 100%. In addition to abnormal clinical vital signs and severe abdominal pain, it is important to consider these indicators when planning treatment strategies, including surgery, to rapidly identify and manage severe PCI.
Conclusions
PCI is a rare condition with cystic gas in the intestinal wall and is often mistaken for other severe gastrointestinal diseases; therefore, physicians should carefully differentiate PCI from other severe diseases.
Figures
References:
1.. Boerner RM, Frie DB, Warshauer DM, Isaacs K, Pneumatosis intestinalis. Two case reports and a retrospective review of the literature from 1985 to 1995: Dig Dis Sci, 1996; 41; 2272-85
2.. Knechtle SJ, Davidoff AM, Rice RP, Pneumatosis intestinalis. Surgical management and clinical outcome: Ann Surg, 1990; 212; 160-65
3.. Im J, Anjum F, Pneumatosis intestinalis. [Updated 2022 Oct 24]: StatPearls [Internet], 2022, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK564381/
4.. Pear BL, Pneumatosis intestinalis: A review: Radiology, 1998; 207; 13-19
5.. Greenstein AJ, Nguyen SQ, Berlin A, Pneumatosis intestinalis in adults: Management, surgical indications, and risk factors for mortality: J Gastrointest Surg, 2007; 11; 1268-74
6.. Knechtle SJ, Davidoff AM, Rice RP, Pneumatosis intestinalis. Surgical management and clinical outcome: Ann Surg, 1990; 212; 160-65
7.. Ling F, Guo D, Zhu L, Pneumatosis cystoides intestinalis: A case report and literature review: BMC Gastroenterol, 2019; 19; 176
8.. Ferrada P, Callcut R, Bauza G, Pneumatosis intestinalis Predictive Evaluation Study: A multicenter epidemiologic study of the American Association for the Surgery of Trauma: J Trauma Acute Care Surg, 2017; 82; 451-60
9.. Wayne E, Ough M, Wu A, Management algorithm for pneumatosis intestinalis and portal venous gas: Treatment and outcome of 88 consecutive cases: J Gastrointest Surg, 2010; 14; 437-48
Figures
In Press
12 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943244
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943275
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943411
13 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942864
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250