17 July 2023: Articles 
Successful Treatment of Cirrhotic Chylous Ascites using Orlistat and Dietary Modifications: A Case Study and Literature Review
Rare disease
Yazan Nofal1ABCDEF, Sara Mahmoud2BF*, Safa Al-Rawi2BEF, Ali Rahil3ACDEFDOI: 10.12659/AJCR.938611
Am J Case Rep 2023; 24:e938611
Abstract
BACKGROUND: Chylous ascites (chyloperitoneum), a condition arising from lymphatic leakage in the peritoneal cavity, is rare in liver cirrhosis patients, accounting for less than 1% of cases. Treatment typically involves therapeutic paracentesis, dietary modifications, a low-fat, high-protein diet, and medium-chain triglyceride (MCT) supplementation. Orlistat, a fat absorption inhibitor, has been reported to show potential efficacy in treating chylous ascites.
CASE REPORT: We detail the case of a 59-year-old male patient admitted for decompensated liver disease and worsening ascites. Diagnostic paracentesis identified chylous ascites, indicated by a 3.5 mmol/L triglyceride level. Despite administering therapeutic paracentesis, dietary modifications, MCT supplementation, Spironolactone, and Terlipressin for a presumed hepatorenal syndrome, the patient's ascites remained chylous for two weeks. On administering orlistat, a significant reduction in ascites volume and chylous content was observed, with triglyceride levels dropping to 0.7 mmol/L.
CONCLUSIONS: Our case illustrates the potential of orlistat in managing chylous ascites in liver cirrhosis patients, marking only the second such case reported in the existing literature. It encourages further exploration of orlistat's therapeutic potential in treating chylous ascites.
Keywords: Chylous Ascites, Liver Cirrhosis, orlistat, Male, Humans, Middle Aged, Ascites, Triglycerides
Background
Chylous ascites, or chyloperitoneum, is seen in 1 in 20 0000 hospital admissions per year [1]. It is a rare form of ascites that appears in 0.5–1% of patients with cirrhosis as de novo or transformed from formerly clear fluids [2,3]. The pathophysiology is via a lymphatic obstruction and/or leakage that causes the accumulation of lipid-rich lymph in the peritoneal cavity [4]. In liver cirrhosis, the formation mechanism of chylous ascites is secondary to the rupture of lymph vessels due to a portal hypertensive state and high lymphatic flow [2]. Therefore, therapy should aim to reduce portal pressure and lymph formation.
Orlistat is a reversible inhibitor of gastric and pancreatic lipase, thus inhibiting dietary fat absorption, and it was found that the use of orlistat can be beneficial in treating chylous ascites [5]. We report a case of chylous ascites secondary to liver cirrhosis attributed to non-alcoholic fatty liver disease successfully treated with short-term orlistat.
Case Report
A 59-year-old man known to have type 2 diabetes mellites and liver cirrhosis attributed to non-alcoholic fatty liver disease, staged as CHILD C with portal hypertension and grade II esophageal varices. He was admitted to our hospital’s medical ward with a 1-day history of altered mental status, worsening abdominal distention, and decreased bowel motions. There was no reported history of abdominal pain, fever, night sweats, weight loss, bleeding, excessive protein intake, or trauma. There was also no history of smoking, alcohol consumption, or a family history of malignancy.
Physical examination revealed an oral temperature of 36.9°C, respiratory rate of 14 breaths per minute, blood pressure of 105/62 mmHg, oxygen saturation of 100% on ambient air, and body weight of 72 kg. The patient was lethargic, with a Glasgow coma scale of 8/15 (eye response: 1, verbal response: 2, motor response: 5) with generalized hypertonicity but no focal neurological deficit. An abdominal exam was significant for a tense, dull abdomen with distended flanks and positive fluid wave but no abdominal masses or organomegaly. The rectal exam showed no blood or masses. There was no lymphadenopathy.
The patient was managed as a case of hepatic encephalopathy precipitated by constipation. He received lactulose enemas and Ceftriaxone i.v. 2 g daily empirically. Ascitic fluid drainage was performed with concomitant albumin administration (Figure 1).
Lab tests upon admission are listed in Table 1. Diagnostic paracentesis is listed in Table 2.
An X-ray study of the chest and abdomen and ultrasound study of the abdomen and pelvis excluded lymphadenopathy or masses concerning for malignancy.
The patient was started on oral lactulose 30 ml PRN (pro re nata) to keep bowel movements 2–3 times per day, and a low-fat, high-protein diet, including medium-chain triglycerides (MCT). After 1 day of admission, his orientation and alertness improved.
On the second day of admission, i.v. Terlipressin 1 mg BID was initiated due to impaired renal function. An ultimate treatment with liver transplant was recommended because a transjugular intrahepatic portosystemic shunt (TIPS) was not a potential option given his degree of encephalopathy.
Ten days after admission and due to persistent accumulation of chylous ascites and lack of response to dietary modifications, orlistat was started at a dose of 120 mg BID. When the patient tolerated the medication and showed improvement, the dose was increased to 120 mg TID after 8 days and was continued for a total of 25 days from initiation. During this time, the volume of ascitic drainage decreased in the first 4 days. However, the volume started to increase again with non-chylous ascites. An ultrasound exam of the abdomen and pelvis revealed partial hepatoportal thrombosis. In addition, he developed a urinary tract infection evident by urinalysis (Table 3), complicated by sepsis. Blood cultures revealed hospital-acquired
The total amount of fluids extracted was 3000 mL before starting orlistat. Then, after 1 day of initiation, the volume decreased to 2000 mL and gradually reduced to 800 ml after 4 days. The chylous content in the acsitic drainage decreased significantly (ascitic fluid triglyceride level decreased from 3.5 to 0.7 mmol/L) 12 days after the initiation of orlistat. Twenty-five days after admission, the drainage tube was removed after total drainage of approximately 40,225 ml. His abdomen distension and ascites resolved. The patient was discharged against medical advice and traveled outside the country shortly thereafter.
Discussion
Chylous ascites is rare and often poses diagnostic and management dilemmas. The most common causes in Western countries are abdominal malignancy, lymphatic abnormalities, and cirrhosis, which account for over two-thirds of all cases [3]. However, infections (eg, tuberculosis and filariasis) are the most common causes in developing countries [6]. In our patient, the history, physical exam, imaging studies, and laboratory investigations upon admission excluded trauma, malignancy, and infectious etiologies such as tuberculosis. However, during the hospitalization, he developed non-chylous ascites. An ultrasound exam of the abdomen and pelvis revealed partial hepatoportal thrombosis, which could be the reason for the worsening ascites volume. In addition, the patient developed a urinary tract infection evident by urinalysis (Table 3), complicated by sepsis. A blood culture revealed hospital-acquired
Limitations of this case report include not sending urine cultures for testing and not repeating the ultrasound exam; the patient and his family were reluctant to do those investigations. Lab tests revealed increased ammonia levels and acute kidney injury (Table 1) managed as hepatorenal syndrome type 2. Diagnostic paracentesis revealed chylous ascites (Table 2). Chylous ascites is seen in 0.5–1.0% of liver cirrhosis cases associated with ascites [2,3]. It is unclear why only a small subset of patients with cirrhosis develops it [2]. Other reported causes of chylous ascites in cirrhotic patients include surgical interventions, portal vein thrombosis, hepatocellular carcinoma, tuberculosis, and constrictive pericarditis [7,10]. In the absence of these causes, chylous ascites is defined as ‘primary’ or ‘idiopathic’ [11]. In our patient, all clinical and laboratory data conclusively demonstrated liver cirrhosis as the main cause of chylous ascites.
The mechanism of the formation of chylous ascites may be due to increased hepatic and gastrointestinal lymph flow due to sinusoidal and post-sinusoidal portal hypertension [11,12]. Because of the high flow rates, the rupture of serosal lymphatic channels results in chylous ascites [2].
The diagnosis of chylous ascites is established as milky fluid with a triglyceride concentration of ≥2.2 mmol/L (200 mg/dl) [13]. The diagnostic criteria for some authors also included a fluid triglyceride to serum ratio >1.0, a cholesterol ratio <1.0, a leukocyte count ≥300 cells/mm3, or a predominance of lymphocytes with negative culture and cytology [14].
Chylous ascites present most frequently as progressive abdominal distention without pain (81% of cases) [6]. Other features include nonspecific abdominal pain, weight loss, diarrhea and steatorrhea, malnutrition, edema, nausea, enlarged lymph nodes, early satiety, fevers, and night sweats. Chylous ascites is usually not suspected until performing diagnostic paracentesis [1,4,15].
The goal of therapy is to treat the underlying pathology, along with the use of conservative measures. The management outline includes dietary modification consisting of a high-protein and low-fat diet with medium-chain triglycerides (MCT) as the initial approach for symptomatic relief of chylous ascites and acts by reducing the production and flow of chyle. Moreover, patients with cirrhotic chylous ascites should be managed with a low-sodium diet and diuretics such as furosemide and Spironolactone [11]. Total parenteral nutrition (TPN) should be reserved for patients who do not respond to the above measures to reduce lymph flow [15]. In this case, Spironolactone was initiated and then later discontinued due to impaired kidney function. TPN was not required since he was able to take oral food, so his diet was changed to a high-protein, low-fat diet.
Octreotide has been reported to treat chylous effusion in cases of portal vein thrombosis, malignancy, and cirrhosis [16,19]. Octreotide decreases portal hypertension and reduces triglyceride levels in ascitic fluid [19]. In addition, octreotide has a role in treating hepatorenal syndrome [20]. However; Octreotide was not available during our patient’s hospitalization.
Orlistat is commonly used for weight reduction by reversibly inhibiting gastric and pancreatic lipase through the inhibition formation of free fatty acids from dietary triglycerides in the intestinal lumen, thereby diminishing fatty acid availability for absorption [21]. It has poor systemic absorption; hence, the associated adverse effects are primarily gastrointestinal, such as loose, oily stools. Orlistat was reported to minimize ascites and triglyceride levels in a patient with chylous ascites due to cirrhosis [5]. To the best of our knowledge, there is only 1 similar published case report, of a 47-year-old man who had a new onset of chylous ascites and chylothorax with poor diet restriction compliance. His ascites’ triglycerides level was 6.6 mmol/L. Orlistat was later added to the treatment. Several days later, his chylous ascites resolved. Similar to our patient, his ascites triglyceride dropped to 0.74 mmol/L. This case suggests the potential benefit of adding orlistat in treating chylous ascites, especially in patients who cannot comply with dietary restrictions [5]. Furthermore, the introduction of orlistat in the treatment of iatrogenic chyle leaks after neck surgery and trauma to the thoracic duct has also been reported to reduce the chyle flow and consequently dramatically accelerates the fistula’s healing and closure [22,24].
In the previously reported case, the remaining high-volume clear ascites was managed by placing a transjugular intrahepatic portosystemic shunt (TIPS). TIPS was reported to be beneficial in a case series of 4 patients with chylous ascites [25]. However, TIPS was not applicable in our case, given his degree of encephalopathy.
Limitations of this case report include utilizing Terlipressin for the treatment of hepatorenal syndrome. Terlipressin may be beneficial in managing hepatic ascites [26], with limited evidence of its effect on the chylous component. To this date, there is only 1 case report (an Italian study published in Italian) that showed a benefit of utilizing Terlipressin in chylous ascites [27]. In our case, Terlipressin could have benefited ascites management; however, the effect on chylous component and volume was only evident after starting orlistat.
Conclusions
In conclusion, chylous ascites is a rare manifestation secondary to several causes, including liver cirrhosis. Our case shows that orlistat can be beneficial in changing the composition and reducing the volume of chylous ascites in a patient with good compliance with a low-fat diet and no suitability for the TIPS procedure. This case report is the second to describe the successful use of orlistat to treat chylous ascites in a cirrhotic patient. It emphasizes the potential role of orlistat in controlling chylous ascites in patients with liver cirrhosis and portal hypertension and will add to the evidence base for future use of this agent.
References:
1.. Press OW, Press NO, Kaufman SD, Evaluation and management of chylous ascites: Ann Intern Med, 1982; 96(3); 358-64
2.. Rector WG, Spontaneous chylous ascites of cirrhosis: J Clin Gastroenterol, 1984; 6(4); 369-72
3.. Sultan S, Pauwels A, Poupon R, Levy VG, [Chylous ascites in adults: Etiological, therapeutic and prognostic aspects. Apropos of 35 cases.]: Ann Gastroenterol Hepatol (Paris), 1990; 26(5); 187-91 [in French]
4.. Browse NL, Wilson NM, Russo F, al-Hassan H, Allen DR, Aetiology and treatment of chylous ascites: Br J Surg, 1992; 79(11); 1145-50
5.. Chen J, Lin RK, Hassanein T, Use of orlistat (xenical) to treat chylous ascites: J Clin Gastroenterol, 2005; 39(9); 831-33
6.. Steinemann DC, Dindo D, Clavien PA, Nocito A, Atraumatic chylous ascites: Systematic review on symptoms and causes: J Am Coll Surg, 2011; 212(5); 899-905.e1–4
7.. Sultan S, Pauwels A, Poupon R, Lévy VG, [Chylous ascites in cirrhosis. Retrospective study of 20 cases.]: Gastroenterol Clin Biol, 1990; 14(11); 842-47 [in French]
8.. Gómez soto FM, Sánchez FM, Franco Moreno AI, Ascitis quilosa como forma de presentación de un hepatocarcinoma: Gastroenterología y Hepatología, 2003; 26(4); 276-77
9.. Williams AT, Schneider RP, Chylous ascites should suggest constrictive pericarditis even in a patient with cirrhosis: J Clin Gastroenterol, 1990; 12(5); 581-84
10.. Díaz Curiel M, Fernández Guerrero ML, Suárez Fernández C, [Infections in liver cirrhosis]: Rev Clin Esp, 1984; 172(5); 241-50 [in Spanish]
11.. Cárdenas A, Chopra S, Chylous ascites: Am J Gastroenterol, 2002; 97(8); 1896-900
12.. Ikeda R, Michitaka K, Yamauchi Y, Changes in gastrointestinal lymph and blood vessels in patients with cirrhotic portal hypertension: J Gastroenterol, 2001; 36(10); 689-95
13.. Almakdisi T, Massoud S, Makdisi G, Lymphomas and chylous ascites: Review of the literature: Oncologist, 2005; 10(8); 632-35
14.. Yilmaz M, Akbulut S, Isik B, Chylous ascites after liver transplantation: incidence and risk factors: Liver Transpl, 2012; 18(9); 1046-52
15.. Aalami OO, Allen DB, Organ CH, Chylous ascites: A collective review: Surgery, 2000; 128(5); 761-78
16.. Leong RWL, House AK, Jeffrey GP, Chylous ascites caused by portal vein thrombosis treated with octreotide: J Gastroenterol Hepatol, 2003; 18(10); 1211-13
17.. Mincher L, Evans J, Jenner MW, Varney VA, The successful treatment of chylous effusions in malignant disease with octreotide: Clin Oncol (R Coll Radiol), 2005; 17(2); 118-21
18.. Ghimire S, Shah H, Paudel S, Chylous ascites and pleural effusion treated with intravenous octreotide: Cureus, 2020; 12(6); e8669
19.. Zhou DX, Zhou HB, Wang Q, The effectiveness of the treatment of octreotide on chylous ascites after liver cirrhosis: Dig Dis Sci, 2009; 54(8); 1783-88
20.. Ojeda-Yuren AS, Cerda-Reyes E, Herrero-Maceda MR, An integrated review of the hepatorenal syndrome: Ann Hepatol, 2021; 22; 100236
21.. Heck AM, Yanovski JA, Calis KA, Orlistat, a new lipase inhibitor for the management of obesity: Pharmacotherapy, 2000; 20(3); 270-79
22.. Yang YH, Park SY, Kim DJ, Chyle leakage after esophageal cancer surgery: Korean J Thorac Cardiovasc Surg, 2020; 53(4); 191-99
23.. Belloso A, Saravanan K, de Carpentier J, The community management of chylous fistula using a pancreatic lipase inhibitor (orlistat): Laryngoscope, 2006; 116(10); 1934-35
24.. Tam D, Scamp T, Tan J, Chyle leak after breast augmentation: Aesthet Surg J, 2009; 29(2); 113-15
25.. Kikolski SG, Aryafar H, Rose SC, Transjugular intrahepatic portosystemic shunt for treatment of cirrhosis-related chylothorax and chylous ascites: Single-institution retrospective experience: Cardiovasc Intervent Radiol, 2013; 36(4); 992-97
26.. Qi X, Bai Z, Zhu Q, Practice guidance for the use of terlipressin for liver cirrhosis-related complications: Therap Adv Gastroenterol, 2022; 15 17562848221098253
27.. Giangreco E, Neri S, Castellino P, Terlipressin in therapy for cirrhotic chylous ascites: A case report: Gazzetta Medica Italiana, 2011; 170(6); 457-60
Tables
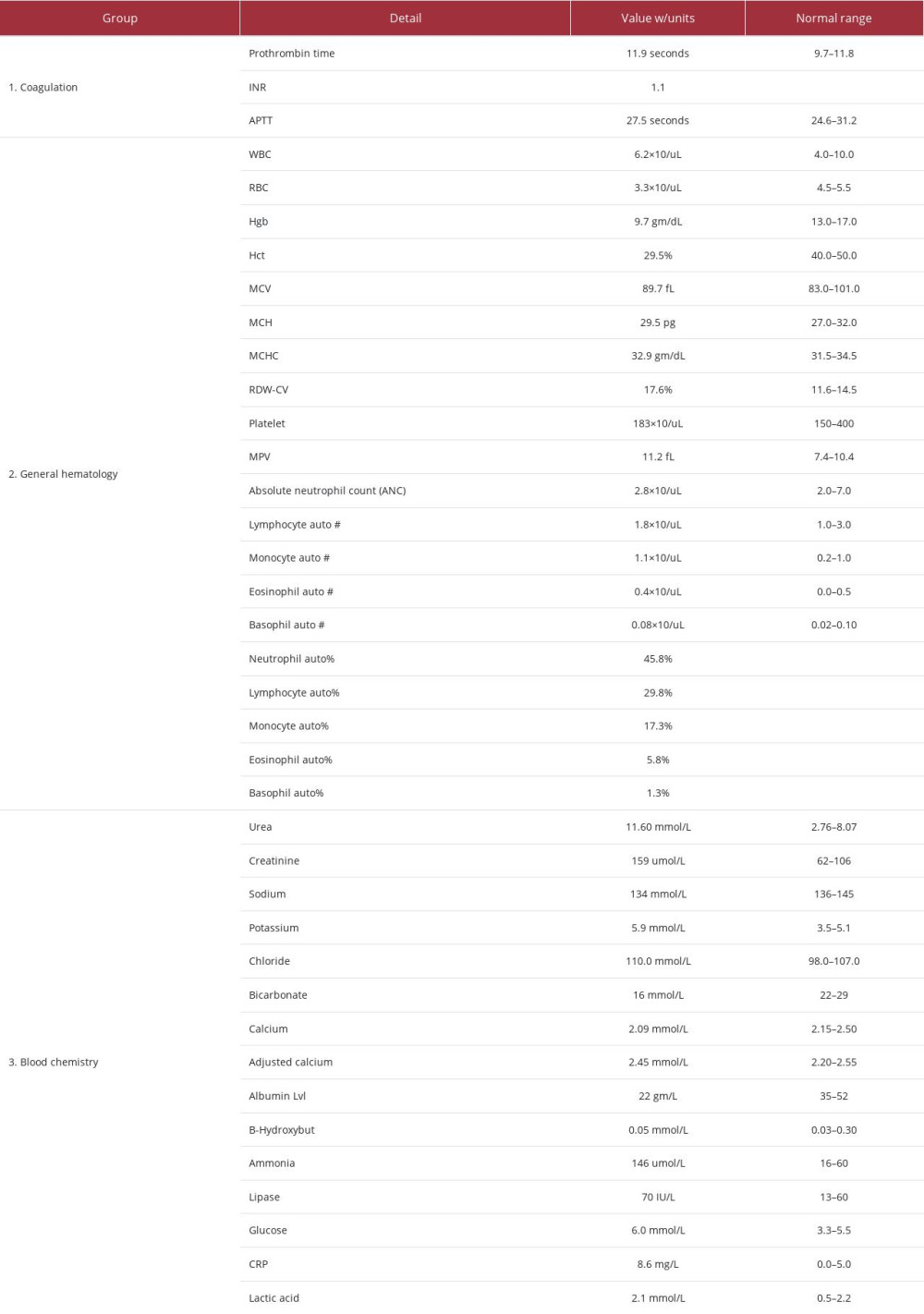 Table 1.. Lab test results upon admission.
Table 1.. Lab test results upon admission.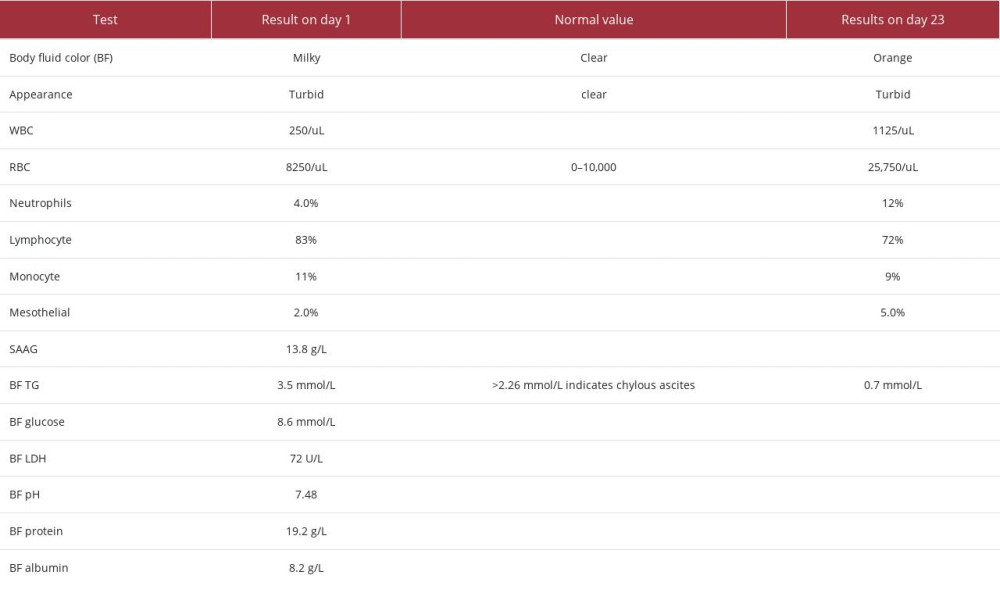 Table 2.. Body fluid triglyceride level day 1 and 12 after initiation of orlistat.
Table 2.. Body fluid triglyceride level day 1 and 12 after initiation of orlistat.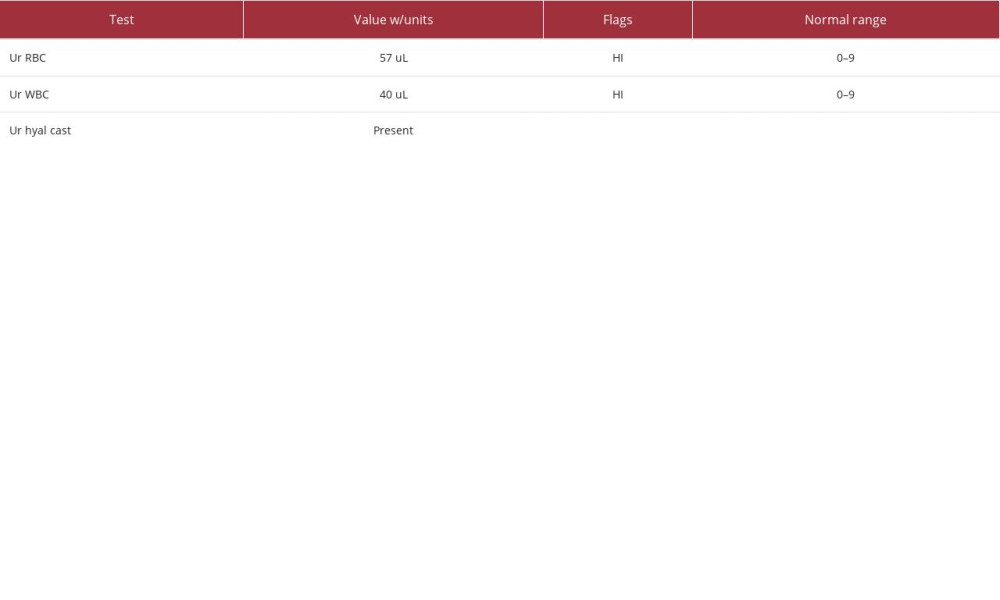 Table 3.. Urinalysis day 17 of hospital admission.
Table 3.. Urinalysis day 17 of hospital admission.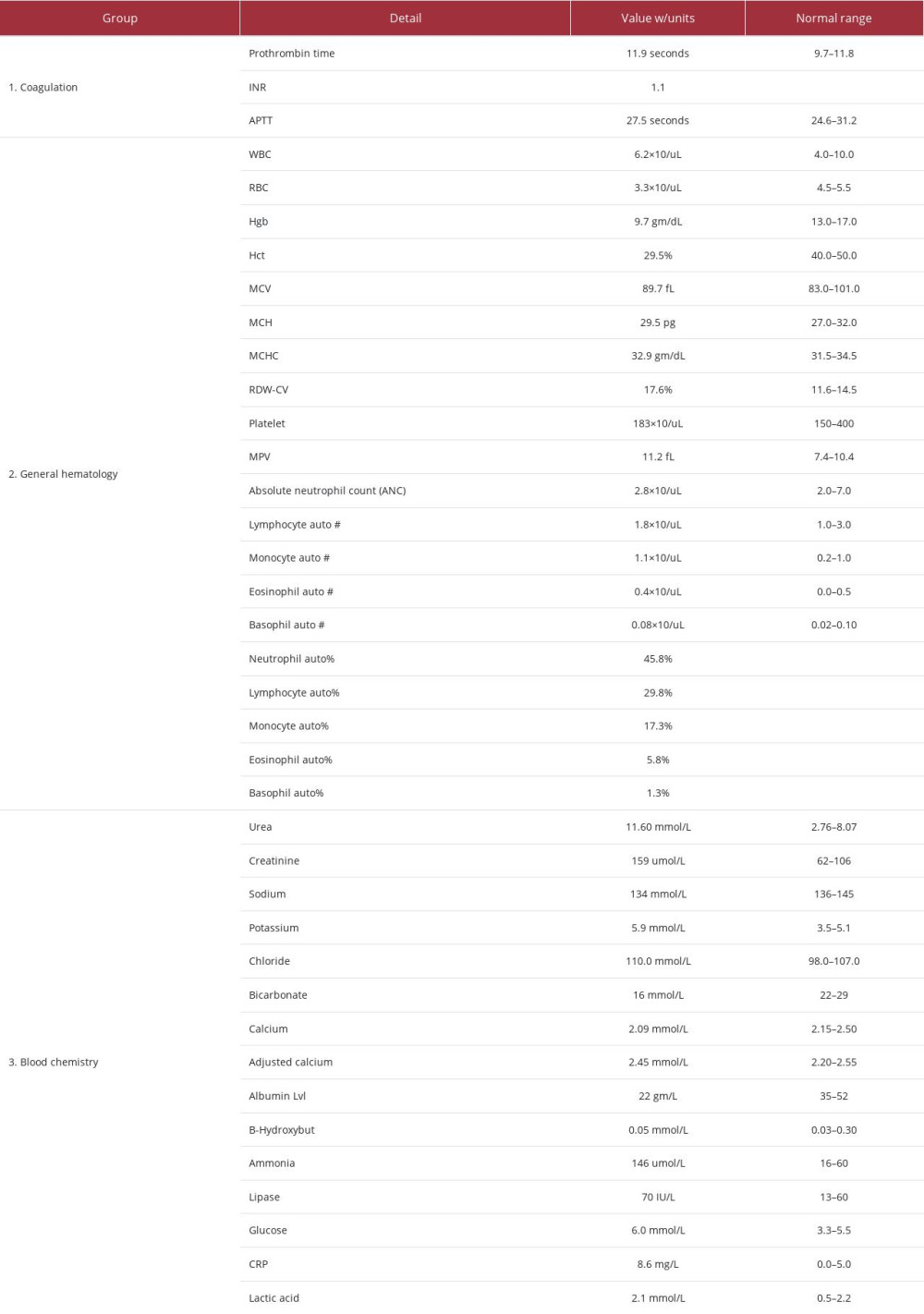 Table 1.. Lab test results upon admission.
Table 1.. Lab test results upon admission.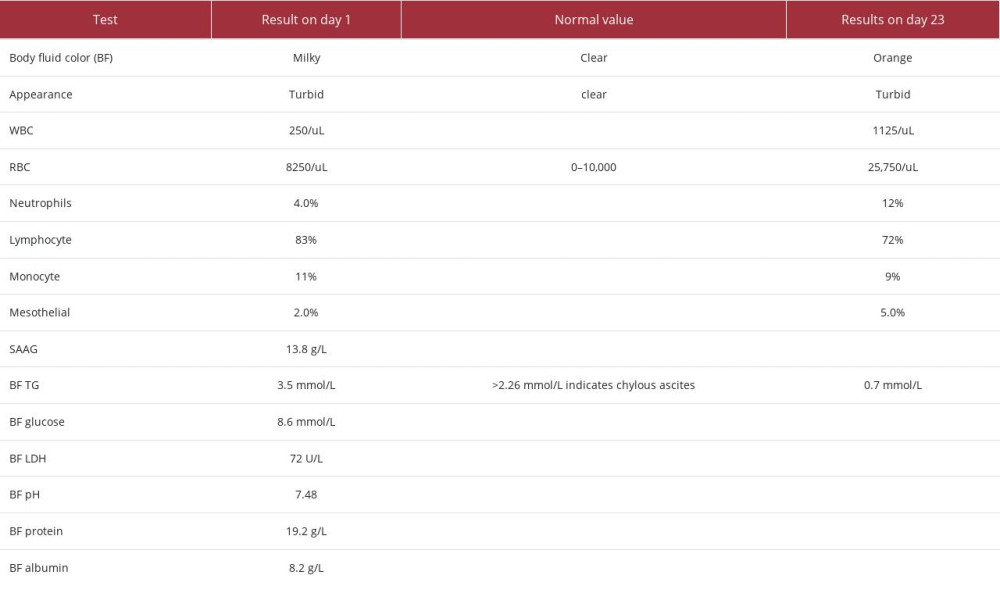 Table 2.. Body fluid triglyceride level day 1 and 12 after initiation of orlistat.
Table 2.. Body fluid triglyceride level day 1 and 12 after initiation of orlistat.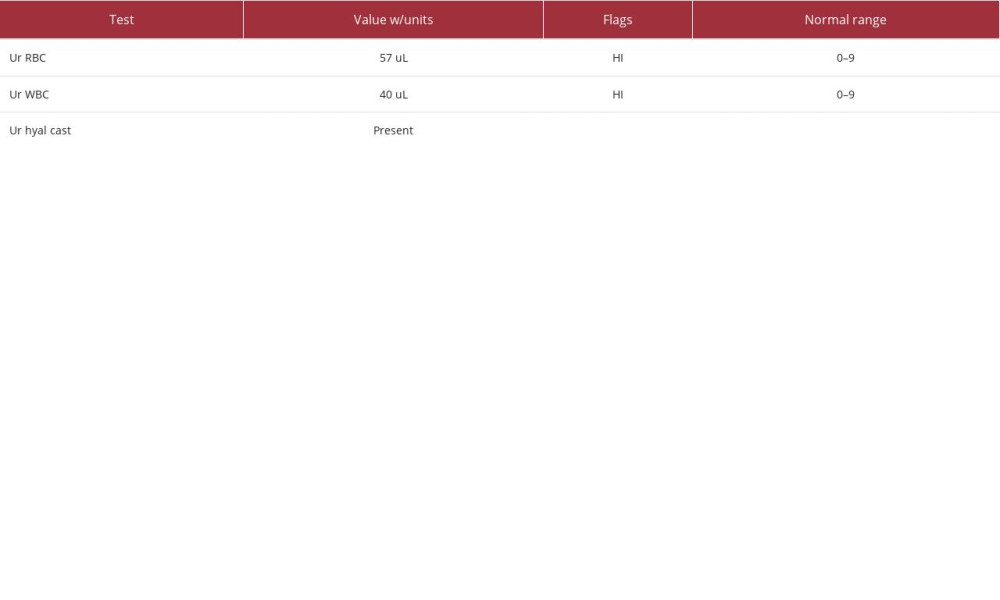 Table 3.. Urinalysis day 17 of hospital admission.
Table 3.. Urinalysis day 17 of hospital admission. In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
22 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943346
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








