14 July 2023: Articles 
Spontaneous Pancreatic Hemorrhage: Successful Conservative Management in Two Cases
Challenging differential diagnosis, Unusual or unexpected effect of treatment, Rare disease
Xiaojia Xiao1ABDF, Yao Liu2E, Yuan Ye1B, Jinglan Wu1F, Zhijun Suo1BD*DOI: 10.12659/AJCR.940109
Am J Case Rep 2023; 24:e940109
Abstract
BACKGROUND: Spontaneous pancreatic and peripancreatic hemorrhage (SPH) is a rare subtype of spontaneous retroperitoneal hemorrhage. With diverse clinical manifestations and no specific presentations, early diagnosis of SPH becomes challenging. Patient-specific underlying causes and vital signs guide the SPH treatment approach.
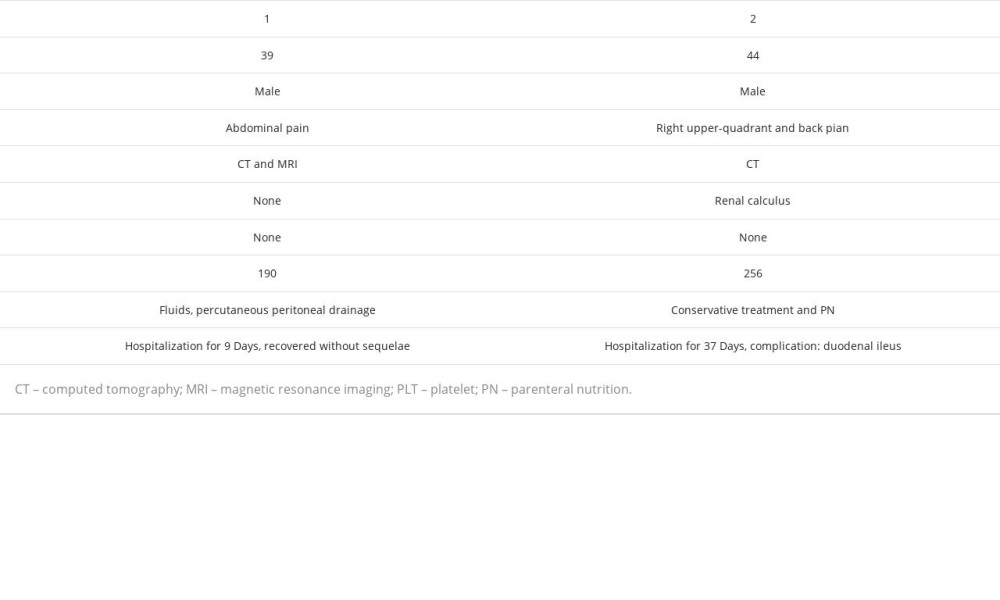
CASE REPORT: Case 1: A 39-year-old man reported unexplained hypogastralgia at the emergency department (ED). An abdominal MRI revealed a mixed hematoma and cystic lesions between the pancreatic head and descending duodenum, attributed to ruptured mucinous cystic neoplasms. Extensive hematoceles were identified around the liver and abdominal pelvis on an enhanced CT scan. After undergoing fasting, rehydration, proton pump inhibitor and somatostatin intravenous injections, and peritoneal puncture, his condition improved. He was discharged nine days post-admission. Case 2: A 44-year-old man arrived at the ED with back pain and right upper quadrant pain. Enhanced CT indicated peritoneal fluid and a hematoma between the pancreatic head and descending duodenum. He initially received conservative treatment. However, on the eighth day, he reported recurrent abdominal pain. Follow-up CT showed an enlarged hematoma and gastric content accumulation. The patient was fasted and put on parenteral nutrition, and by the 37th day of hospitalization, he had fully recovered and was discharged. Both patients, having stable hemodynamics, fully recovered following conservative management, with no surgical intervention required.
CONCLUSIONS: Given its varied clinical presentations, SPH can easily be misdiagnosed. However, successful conservative management can lead to full recovery, as demonstrated in these case reports.
Keywords: Abdominal Pain, Hemorrhage, Pancreas, Retroperitoneal Neoplasms, Male, Humans, Adult, conservative treatment, Gastrointestinal Hemorrhage, Hematoma
Background
Early diagnosis is difficult but necessary for acute abdominal diseases. Spontaneous retroperitoneal hemorrhage (SRH) is one of the acute abdominal diseases, which refers to spontaneous retroperitoneal blood vessel rupture and bleeding. It is a relatively rare disease with an incidence rate of about 0.1–6.6% and a mortality rate of about 20% [1]. The main causes of SRH include trauma, iatrogenic injury, cancer, dialysis and anticoagulant therapy. SRH usually occurs at parenchymal organs and blood vessels [2]. Previous reported cases of spontaneous parenchymal organ hemorrhage mostly occurred in the adrenal gland and kidney, while few cases of spontaneous pancreatic and peripancreatic hemorrhage (SPH) were reported. Moreover, most of the reported cases and studies with SPH were treated through digital subtraction angiography (DSA) and percutaneous embolization or surgery [3,4]. Here, we present 2 cases with SPH admitted in Union Shenzhen Hospital of Huazhong University of Science and Technology from March 2021 to March 2022, which were successfully reversed with conservative treatment.
Case Reports
CASE 1 (PATIENT 1):
A 39-year-old man was admitted with abdominal pain for 2 days without an obvious trigger such as trauma or alcoholism, who had no previous medical history or family or personal history of a connective tissue disorder. The patient underwent abdominal puncture in the external hospital before 1 day, which indicating bloody ascites combined with decreased hemoglobin. He was transferred to our hospital the next day after fasting and fluid resuscitation. Physical examination showed normal vital signs. Abdominal assessment showed only mild tenderness in the left upper quadrant. Blood test results showed a 123 000 per mL white blood cells, 9.0 mg/dL hemoglobin, and normal blood platelet and coagulation function. Amylase and lipase began to elevate to 256U/L and 1163U/L on hospital day 4. Abdominal magnetic resonance imaging (MRI) showed mixed hematoma and cystic lesions located between the pancreatic head and the descending duodenum (Figure 1A), 50×40 mm in size, which revealed hematoma from ruptured mucinous cystic neoplasms. Enhanced computed tomography (CT) showed extensive hematocele around the liver and abdominal pelvis (Figure 1B). Angiography showed no aneurysm or active bleeding.
On the second day of admission, he received peritoneal puncture therapy, and 450 ml of non-coagulant fluid was drained on the first day. The biochemical analysis of the ascites indicated that amylase, white cell count, and red blood cell count were 32 U/L, 3842 per mL, and 4 150 000 per mL, respectively, and Rivalta test was positive. During this period, the hemoglobin level decreased twice, with the lowest hemoglobin level of 8.2 mg/dl. The patient received the treatments of fasting, rehydration, intravenous injection of proton pump inhibitors to decrease gastric volume and somatostatin to reduce pancreas secretion. The patient’s condition improved and he was discharged 9 days after admission. After 1 year of follow-up, he was living and working normally.
CASE 2 (PATIENT 2):
A 44-year-old man presented with back pain for 5 h and right upper-quadrant pain for 4 h without any causes, accompanied by abdominal distension, profuse sweating, and vomiting.
There was no history of trauma, alcoholism, or anticoagulant use, nor family history or personal history of connective tissue disease. Physical examination revealed normal vital signs. An abdominal examination found tension of abdominal muscle, obvious tenderness and rebound pain in the right upper abdomen, but no obvious mass. Blood test results showed the white cell counts, blood platelets, and hemoglobin level were 178 000 per mL, 15.4g/L, and 256 000 per mL, respectively. The levels of amylase, lipase, coagulation function and tumor marker were normal at admission. CT suggested a small amount of peritoneal fluid and a hematoma located between in pancreatic head and the descending duodenum (Figure 2A). After admission, the patient received conservative treatment, including fasting, rehydration, transfusion, intravenous injection of proton pump inhibitors, and somatostatin. He developed abdominal pain again after 8 days, accompanied by abdominal distention, nausea, vomiting, and increasing abdominal pain after eating. Abdominal CT showed an enlarged hematoma (50×30 mm) between the pancreatic head and the descending duodenum, and accumulated gastric contents (Figure 2B).
Angiography showed no aneurysm or active bleeding. The patient could not receive enteral nutrition support through gastric tube due to gastric outlet obstruction. Therefore, he had to receive parenteral nutrition. The daily gastric residual volume was 500–2000 mL, and gradually decreased to 100 mL on the 27th day of hospitalization. On days 31, he began to try an oral fluid diet, with alleviated abdominal pain and stable hemodynamics. He recovered and discharged on hospital day 37.
Discussion
The causes of SPH include trauma, iatrogenic injury, cancer, dialysis, and anticoagulant therapy, which can be divided into neoplastic and non-neoplastic factors. The main non-neoplastic factors are pancreatic pseudocysts and peripancreatic pseudoaneurysms. The causes of aneurysms in peripancreatic arteries are atherosclerosis, pancreatitis, celiac compression, congenital, mycotic, trauma, rheumatoid vasculitis, iatrogenic, and fibromuscular hyperplasia [5]. Pancreatic cystic lesions are often found in spontaneous rupture and hemorrhage of pancreatic tumors. The most common lesions are serous cyst-adenomas (SCAs), intraductal papillary mucinous neoplasms (IPMNs), and mucinous cystic neoplasms (MCNs). Cha et al reported a case of SPH with SCAs, IPMNs, and pNETs [4]. The patients in the present report were all males and had no specific history of trauma or anticoagulant therapy. In Patient 1, MCN was first found by abdominal MRI. About 80–90% of MCN lesions occur in the tail of the pancreas, manifested as single or multiple thick-walled cysts with thick cystic fluid, high CEA, and low amylase [6]. However, no obvious cause was found in Patient 2 and the hematoma might have been idiopathic.
Based on anatomical location, the foramen of Winslow allows communication between the lesser sac and the subhepatic space [7]. Usually, the retroperitoneum is not connected to the abdominal cavity. When the content of the retroperitoneal space increases, it can enter the abdominal cavity through the foramen of Winslow, which is why the free abdominal fluid accumulated after SPH in these 2 Patients. Asymptomatic patients with small lesions were regularly observed and received conservative treatment, but when the lesion rapidly increases in the short term, patients with obvious symptoms and complications (eg, portal hypertension, biliary obstruction, gastrointestinal obstruction, hemorrhagic shock, septic shock) need invasive intervention [7].
SRH has various clinical manifestations and is easily misdiagnosed, with subsequent delayed treatment [8,9]. It usually consists of a sudden onset of severe upper abdominal pain, which often radiates to the lateral lower back and causes diaphragm irritation, and is sometimes accompanied with gastrointestinal symptoms and descending hemodynamics. If the hematoma compresses the femoral nerve, it will cause pain, paralysis, and dyskinesia in the lower extremities and hip joints. The mortality rate of SRH was reported to be 5.6% within 7 days and 19.1% within 6 months [10]. Therefore, rapid and accurate diagnosis is critical for the prognosis of SRH. Emergency abdominal ultrasound is usually the first examination method, with low sensitivity in retroperitoneal diseases [11]. In the 2 patients in this report, free peritoneal effusion could be detected by ultrasound, but due to the interference of gas in the gastrointestinal tract, it is difficult to detect pancreatic lesions. CT scanning is considered to be the most reliable imaging method to diagnose SRH, and it plays a crucial role in detection of active bleeding and pathological conditions [2]. Moreover, in patients with unstable hemodynamics, DSA can be used to identify the bleeding site, which can then be treated via arterial embolization or stent placement [12]. In the patients in this report, we promptly performed CT and MRI examinations to determine the characteristics and location of the hematoma, and angiography was used to determine if there was active bleeding.
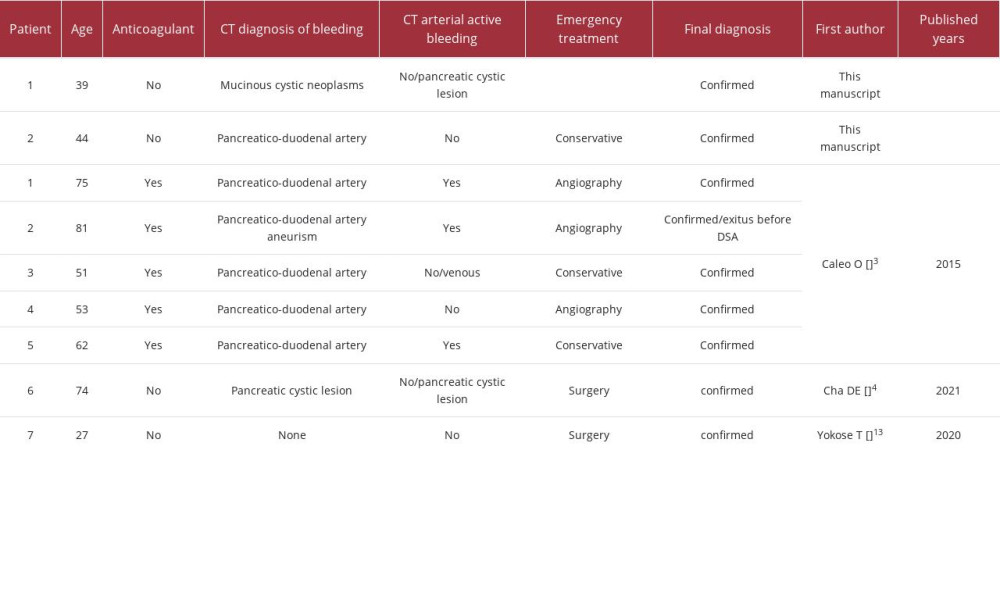
The treatment of SRH consists of conservative treatment, interventional radiology, and surgery, depending on the etiology and hemodynamic stability of the hemorrhage. Interventional radiology is a safe and effective treatment, involving selective intra-arterial embolization and deployment of stent-grafts over the punctured vessel [3]. Only patients who develop severe complications such as abdominal hypertension syndrome and obstruction after conservative or interventional treatment require surgical treatment [4,13]. A 74-year-old man underwent pancreaticoduodenectomy due to the risk of malignancy and the possibility of re-bleeding [4]. However, in SRH patients in stable condition, conservative treatment is more likely to achieve clinical improvement through correcting coagulation function, fluid resuscitation, and blood transfusion [14]. Similarly, our 2 patients were treated successfully through conservative treatment, although the etiologies were different. These cases are compared and displayed in the Table 2.
Conclusions
SPH is special type of SRH that can present with a variety of clinical manifestations, even with minimal bleeding. It is important to quickly diagnose and differentiate this disease from other pancreatic diseases. Moreover, under stable hemodynamics, conservative treatment can enable patients to achieve improvement.
Figures
References:
1.. Gonzalez C, Penado S, Llata L, The clinical spectrum of retroperitoneal hematoma in anticoagulated patients: Medicine (Baltimore), 2003; 82(4); 257-62
2.. Gimeno Argente V, Bosquet Sanz M, Ramírez Backhaus M, [Spontaneous retroperitoneal hemorrhage: Our experience at last 10 years]: Actas Urol Esp, 2007; 31(5); 521-27 [in Spanish]
3.. Caleo O, Bocchini G, Paoletta S, Spontaneous non-aortic retroperitoneal hemorrhage: Etiology, imaging characterization and impact of MDCT on management. A multicentric study: Radiol Med, 2015; 120(1); 133-48
4.. Cha DE, Horn C, Passeri M, Triple threat: pancreatic cystic lesion presenting with spontaneous hemorrhage is found to harbor three distinct neoplasms: World J Surg Oncol, 2021; 19(1); 15
5.. Neschis DG, Safford SD, Golden MA, Management of pancreaticoduodenal artery aneurysms presenting as catastrophic intraabdominal bleeding: Surgery, 1998; 123(1); 8-12
6.. van Huijgevoort NCM, Del Chiaro M, Wolfgang CL, Diagnosis and management of pancreatic cystic neoplasms: Current evidence and guidelines: Nat Rev Gastroenterol Hepatol, 2019; 16(11); 676-89
7.. Tirkes T, Sandrasegaran K, Patel AA, Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging: Radiographics, 2012; 32(2); 437-51
8.. Horsley-Silva JL, Ngamruengphong S, Frey GT, Paz-Fumagalli R, Lewis MD, Segmental arterial mediolysis: A case of mistaken hemorrhagic pancreatitis and review of the literature: JOP, 2014; 15(1); 72-77
9.. Mitura K, Romanczuk M, Ruptured ectopic pregnancy mimicking acute pancreatitis: Ginekol Pol, 2009; 80(5); 383-85
10.. Sunga KL, Bellolio MF, Gilmore RM, Spontaneous retroperitoneal hematoma: Etiology, characteristics, management, and outcome: J Emerg Med, 2012; 43(2); e157-61
11.. Dolapsakis C, Giannopoulou V, Grivakou E, Spontaneous retroperitoneal hemorrhage: J Emerg Med, 2019; 56(6); 713-14
12.. Chan YC, Morales JP, Reidy JF, Management of spontaneous and iatrogenic retroperitoneal haemorrhage: Conservative management, endovascular intervention or open surgery?: Int J Clin Pract, 2008; 62(10); 1604-13
13.. Yokose T, Kitago M, Oshima G, Urgent distal pancreatectomy for intraperitoneal hemorrhage due to the spontaneous rupture of a pancreatic metastatic tumor from synovial sarcoma: a case report: BMC Surg, 2020; 20(1); 175
14.. Lukies M, Gipson J, Tan SY, Spontaneous retroperitoneal haemorrhage: Efficacy of conservative management and embolisation: Cardiovasc Intervent Radiol, 2023; 46(4); 488-95
Figures
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250