02 August 2023: Articles 
A Rare Case of Moyamoya Disease in a Hispanic Woman: Unveiling Non-Asian Ethnicity and Atypical Risk Factors
Rare disease
William P. Ott1EF*, Shannay Bellamy1BEF, Chike B. Onyali1ABFDOI: 10.12659/AJCR.940353
Am J Case Rep 2023; 24:e940353
Abstract
BACKGROUND: Moyamoya disease is a rare and progressive cerebrovascular disorder caused by narrowed or blocked arteries supplying the brain. First described in Japan, the disease’s incidence is higher in Asian countries and primarily affects children, although adults can also be afflicted. Following a literature review, very little was found regarding non-Asian ethnicities and the lack of typically associated risk factors that are known correlates of Moyamoya disease.
CASE REPORT: We present the case of a 41-year-old Hispanic woman with a history of type 1 diabetes mellitus and asthma who presented to the Emergency Department with concerns of recurrent transient episodes of left upper extremity weakness and paresthesia followed by confusion. The patient's blood pressure on arrival was 215/134 mmHg, and heart rate was 124 beats per min. Computed tomography of the head was unremarkable, but a computed tomography angiogram of the head demonstrated several areas of severe and bilateral stenosis with radiographic appearances, suggestive of Moyamoya disease. Magnetic resonance imaging of the brain would later illustrate two 6×2-mm ischemic infarcts in the right posterior centrum semiovale.
CONCLUSIONS: Moyamoya disease in the non-Asian population is rarely reported. We present a case of this condition in a patient of Hispanic ethnicity. Although it is generally considered a non-atherosclerotic disease, some literature suggests that atherosclerotic disease may also contribute to the development and possible acceleration of clinical features of Moyamoya disease. Given our patient’s risk factors, we postulated that our patient’s presentation was likely multifactorial, with both non-sclerotic and atherosclerotic disease.
Keywords: Circle of Willis, ischemic stroke, moyamoya disease, Adult, Female, Child, Humans, ethnicity, Hispanic or Latino, Cerebral Angiography, Risk Factors
Background
Moyamoya disease (MMD) is a rare disease of the cerebral vasculature characterized by progressive bilateral stenosis of the anterior vessels of the Circle of Willis, with subsequent predisposition to cerebral ischemia and infarction [1]. The condition is more common in patients of Eastern Asian descent, and females are more commonly affected than males. MMD has been associated with neurofibromatosis, Down syndrome, sickle cell disease, renal artery stenosis, antiphospholipid syndrome, and autoimmune diseases, such as type 1 diabetes mellitus [1,2]. We present a case of a 41-year-old Hispanic woman with a history of type 1 diabetes mellitus and asthma who presented with recurrent episodes of transient neurological deficits, ultimately being found to have angiographic findings suggestive of MMD.
Case Report
This is a case of a 41-year-old Hispanic woman with a history of insulin-dependent diabetes mellitus and asthma who presented to the Emergency Department (ED) with concerns of recurrent transient episodes of left upper extremity weakness and paresthesia followed by confusion. She had been driving when she suddenly experienced left upper extremity weakness and heaviness, followed by paresthesia and numbness extending from her left arm to the left side of her neck. She stopped her car to call for help, and after a few minutes, the symptoms had completely resolved. However, she could not recall why she had pulled over. Over the next several hours, 2 nearly identical episodes prompted her to seek medical attention in the ED. She reported a family history of multiple strokes in her mother, which began in her thirties. She denied any tobacco, alcohol, or illicit drug use.
On presentation, she had a blood pressure of 215/134 mmHg, heart rate of 124 beats per min, temperature of 36.6°C, and oxygen saturation of 99% on room air. She was fully oriented and in no acute distress, with no focal neurological deficits on examination. Her blood pressure improved with the administration of labetalol 5 mg intravenously. While in the ED, she had 3 witnessed episodes of left upper extremity weakness and numbness, each lasting a few minutes before completely resolving spontaneously. With each reported episode, there was an associated rise in blood pressure.
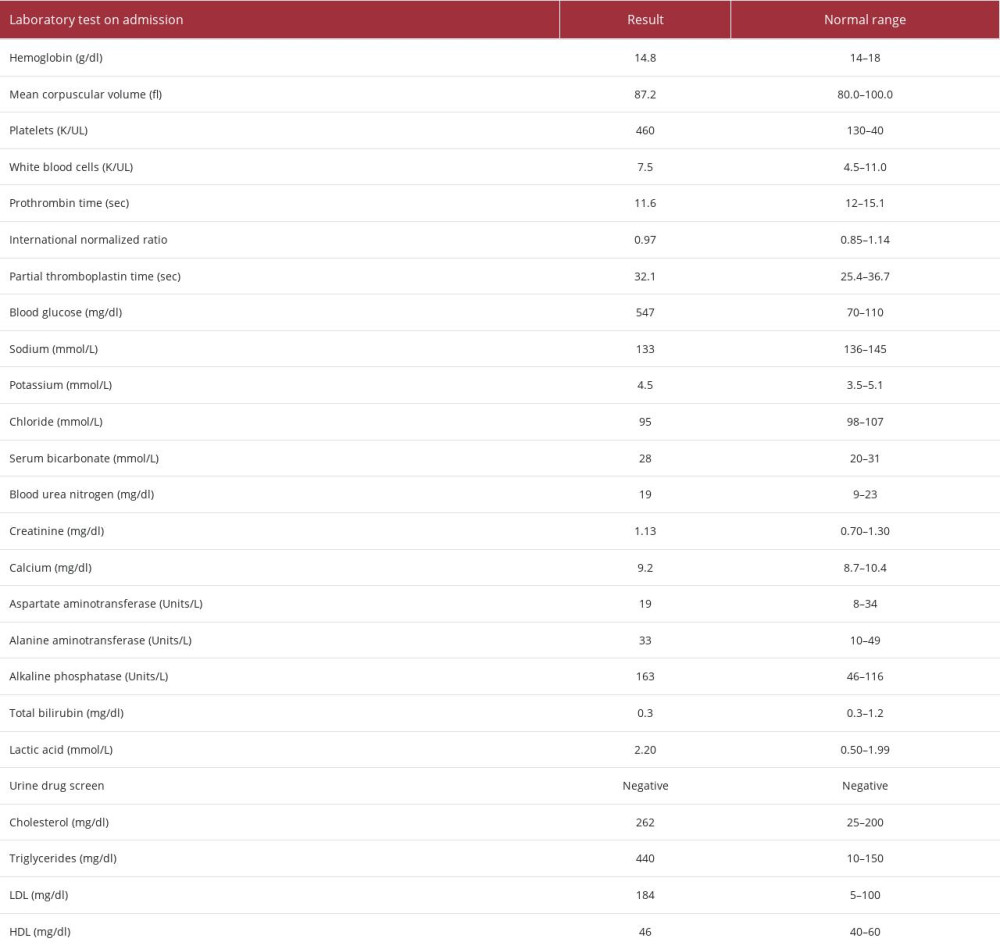
Laboratory investigations on admission were significant for hyperglycemia, with a blood glucose level of 547 mg/dL, hyper-lipidemia, and elevated lactic acid level (Table 1). Computed tomography (CT) of the head showed no acute infarct or hemorrhage. However, CT angiography (CTA) of the head demonstrated extensive high-grade and near occlusive stenoses in the right greater than left internal carotid arteries and middle cerebral arteries, with numerous apparent tiny likely collateral arteries with “puff of smoke” appearance highly suspicious for MMD (Figure 1). Magnetic resonance imaging (MRI) of the brain was significant for two 6×2-mm ischemic infarcts in the right posterior centrum semiovale (Figure 2). Further evaluation of the cerebral vasculature with a magnetic resonance angiography (MRA) of the head demonstrated high-grade stenosis of the bilateral cavernous carotid arteries, supraclinoid carotid arteries, and proximal segments of the middle cerebral arteries (Figure 3). She was commenced on dual antiplatelet therapy with aspirin, clopidogrel, and the antihypertensive losartan. The Neurology and Neurovascular Surgery teams were consulted. She underwent a cerebral angiogram, with 3-dimensional reconstruction to help guide potential future therapeutic interventions. The findings of the cerebral angiogram were similar to those seen in the MRA.
With no further episodes of neurological symptoms and improvement of blood pressure and blood glucose control, she was discharged home with recommendations of close follow-up with the Neurosurgery Department regarding plans for direct/ indirect cerebral revascularization therapies.
Discussion
MMD is an extremely uncommon cerebrovascular disease, with an incidence of about 0.086 per 100 000 persons in the United States [1]. It is most common among East Asians, with the highest prevalence in children of Japanese descent (incidence of 6.03 per 100 000). It is rare in North Americans and Europeans and even rarer in Hispanic Americans, with a prevalence of 0.03 per 100 000 [3,4]. Incidence tends to peak in 2 different age groups: children around 5 years of age and then again in adults in their fourth decade of life [5]. Our patient fits appropriately within this bimodal distribution of age group incidences, but was unique in regard to her ethnicity.
The underlying cause of MMD is unknown. Its higher prevalence among East Asians and familial involvement suggests that genetics may play a role in the development of the disease [6]. Specifically, numerous studies have proposed that variants in the RNF213 gene on chromosome 17 (proposed to be inherited in an autosomal dominant manner) may predispose to the development of MMD in these populations [7]. Additional associations with loci on chromosomes 3, 6, and 8 and specific human leukocyte antigen haplotypes have been described. Despite this, there are reports of identical twins with only 1 affected sibling, thus providing support for the idea that environmental factors precipitate the clinical facilitation of this condition in potentially predisposed individuals [5].
MMD most commonly affects the intracranial portion of the internal carotid arteries, anterior cerebral arteries, and proximal portion of the middle cerebral artery, sparing the posterior arteries of the Circle of Willis [1,2]. Progressive stenosis of these cerebral arteries leads to downstream cerebral ischemia. As a result, new blood vessels form as a compensatory response to cerebral hypoperfusion. However, these new collateral vessels are usually fragile and can easily rupture [1].
The diagnosis of MMD relies heavily on cerebral angiography. MRA can demonstrate areas of stenosis and the collateral vasculature seen in MMD. Combined with MRI of the brain, MRA can demonstrate brain parenchymal lesions suggestive of stroke. CTA is reserved for cases in which MRA is not readily available [2,8]. Despite the diagnostic ability of MRA, conventional angiography remains the criterion standard test for the diagnosis of MMD [2]. It is important to note though that the English version of the 2009 diagnosis criteria published in 2012 states that cerebral angiography can actually be omitted when MRI/MRA findings meet 3 specific criteria: MRA showing stenosis or occlusion of the intracranial internal carotid arteries or proximal portions of the anterior/ middle cerebral artery; MRA showing abnormal vascular networks in the basal ganglia; and the bilaterality of the aforementioned [9]. In our case, abnormal vascular networks of the basal ganglia were not mentioned specifically; therefore, for further delineation and mapping, the patient proceeded to a cerebral angiogram.
Transient ischemic attacks and stroke are the most common presenting features of MMD [10]. Strokes in MMD are considered non-atherosclerotic, with ischemic strokes being more common in the pediatric population and hemorrhagic strokes being more common in adults [4]. Hemorrhagic strokes in MMD are secondary to rupture of the collateral vessels or rupture of aneurysms that form in the stenotic cerebral arteries [4].
Another common clinical finding in patients with MMD is hypertension, as seen in our case. Renovascular disease, particularly renal artery stenosis, has been identified as the potential cause of hypertension in about 5% of cases [11]. Genetic variants of the RNF213 gene are also thought to affect the renal vasculature resulting in renal artery stenosis. In patients without renal artery stenosis, elevated blood pressure is thought to be a compensatory mechanism to increase perfusion to the ischemic brain parenchyma [5]. We suspect the elevated blood pressure readings, which worsened during the times of transient neurologic deficits in our patient, were likely the result of this latter mechanism. The workup of potential secondary causes of the patient’s hypertension, after a shared decision-making agreement, was agreed to be completed in an outpatient setting following discharge.
Additionally, patients with MMD have comorbidities that can predispose them to atherosclerotic disease, including hyperlipidemia and diabetes mellitus [12,13]. Although not pathologically proven, atherosclerotic disease of the intracranial arteries has been proposed as a potential contributor to the development of MMD [8]. Interestingly, our patient had many risk factors for MMD. Her history of type 1 diabetes mellitus (one of the autoimmune diseases commonly identified in MMD, with which she reported being diagnosed in her teenage years) and a family history of multiple strokes in her mother, suggesting a possible familial relation, may implicate non-atherosclerotic MMD. However, her uncontrolled hypertension, diabetes mellitus (with subsequent bouts of dehydration), and hyperlipidemia suggest the possibility of atherosclerotic MMD. In this case, we postulate that her MMD may likely have been multifactorial, involving both non-atherosclerotic and atherosclerotic diseases.
Medical management of cerebral ischemia in MMD consists of lifestyle modifications and management of comorbidities, such as hypertension, diabetes, and hyperlipidemia [14]. Aspirin and other antiplatelet drugs, including cilostazol, have been commonly used in the management of MMD [15]. A large-scale study done by Seo et al in the Korean population in 2021 regarding antiplatelet therapy, particularly cilostazol, was associated with significant survival benefits in patients with MMD [16]. Despite these findings, surgical revascularization is the main therapy for MMD and is associated with better outcomes than medical management alone [15].
Conclusions
MMD is rare and is more uncommon when non-Asian and adult populations are analyzed. Significant importance is levied on lifestyle optimization, which entails tight control of known comorbidities that can exacerbate this disease, as well as on medical and surgical management to prevent any worsening or future damage to the brain. Our case highlights not only the unique patient demographics that this disease can uncommonly present with but also how its effects can easily be worsened when common comorbidities, such as hypertension and diabetes mellitus, are not well controlled.
Figures
References:
1.. Berry JA, Cortez V, Toor H, Moyamoya: An update and review: Cureus, 2020; 12(10); e10994
2.. Shoukat S, Itrat A, Taqui AM, Moyamoya disease: A clinical spectrum, literature review and case series from a tertiary care hospital in Pakistan: BMC Neurol, 2009; 9; 15
3.. Said S, Cooper CJ, Alkhateeb H, Moyamoya in Hispanics: Not only in Japanese: Neurol Int, 2014; 6(2); 5369
4.. Fox BM, Dorschel KB, Lawton MT, Wanebo JE, Pathophysiology of vascular stenosis and remodeling in Moyamoya disease: Front Neurol, 2021; 12; 661578 [Erratum in: Front Neurol. 2021;12:812027]
5.. Santoro JD, Lee S, Mlynash M, Blood pressure elevation and risk of moyamoya syndrome in patients with trisomy 21.: Pediatrics., 2018; 142(4); e20180840
6.. Zhang H, Zheng L, Feng L, Epidemiology, diagnosis and treatment of moyamoya disease.: Exp Ther Med., 2019; 17(3); 1977-84
7.. Roy V, Ross JP, Pépin R, Moyamoya disease susceptibility gene RNF213 regulates endothelial barrier function.: Stroke, 2022; 53(4); 1263-75
8.. Scott RM, Smith ER, Moyamoya disease and moyamoya syndrome: N Engl J Med, 2009; 360(12); 1226-37
9.. Kuroda S, Fujimura M, Takahashi J, Diagnostic criteria for Moyamoya disease – 2021 revised version: Neurol Med Chir (Tokyo), 2022; 62(7); 307-12
10.. Kim JS, Moyamoya disease: Epidemiology, clinical features, and diagnosis: J Stroke, 2016; 18(1); 2-11
11.. Liu E, Zhao H, Liu C, Research progress of moyamoya disease combined with renovascular hypertension: Front Surg, 2022; 9; 969090
12.. Chan J, D’Ambrosio Rodriguez F, Sahni D, Boucher-Berry C, Moyamoya disease with coexistent hypertriglyceridemia in pediatric patient: Case Rep Endocrinol, 2016; 2016; 7974182
13.. Bolem N, Nga VDW, Chou N, Coexisting Moyamoya syndrome and type 1 diabetes mellitus: A case report and review of the literature: Asian J Neurosurg, 2020; 15(1); 194-97
14.. Dalal F, Frazier G, Dass SR, Case report: Moyamoya disease in a 47-year-old woman.: Am Fam Physician., 2022; 106(2) Online
15.. Pang CH, Cho WS, Kang HS, Kim JE, Benefits and risks of antiplatelet medication in hemodynamically stable adult moyamoya disease.: Sci Rep, 2021; 11(1); 19367
16.. Seo WK, Kim JY, Choi EH, Association of antiplatelet therapy, including cilostazol, with improved survival in patients with moyamoya disease in a nationwide study.: J Am Heart Assoc., 2021; 10(5); e017701
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942921
22 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943346
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250