03 July 2023: Articles 
Successful Extracorporeal Cytokine Hemoadsorption in a Marfan Syndrome Patient with COVID-19 Undergoing Redo Bentall Procedure
Management of emergency care
Ajmer Singh1BCE, Chinmaya Nanda1BCE, Yatin Mehta2BE*, Anil Bhan3ADEDOI: 10.12659/AJCR.940383
Am J Case Rep 2023; 24:e940383
Abstract
BACKGROUND: Patients with COVID-19 undergoing emergency or complex surgical procedures are at increased risk of developing perioperative complications. CytoSorb is a blood purification therapy used to remove circulating cytokines in conditions of hyperinflammation. This report is of a patient with COVID-19 requiring redo replacement of the aortic valve and aorta due to aortic aneurysm of the ascending aorta (Bentall procedure) associated with Marfan syndrome. The patient was successfully treated with extracorporeal cytokine hemoadsorption.
CASE REPORT: A 34-year-old man with Marfan syndrome, who had undergone a Bentall procedure in 2018, was admitted with symptoms of worsening dyspnea, tachycardia, fever, and confirmed COVID-19. Further diagnostic workup revealed dehiscence of the aortic root as well as moderate aortic regurgitation, in the context of a hyperinflammatory state. Anti-infective treatment was initiated. Given the severity of symptoms, COVID-19, echocardiography findings, and risk of aortic rupture, urgent Bentall surgery was performed. Additionally, a CytoSorb hemoadsorber was integrated into the cardiopulmonary bypass circuit to attenuate the anticipated systemic hyperinflammation. Intraoperatively, several blood products were administered due to excessive bleeding from the friable tissues and the pre-existing anemia and thrombocytopenia. Treatment was associated with marked improvements in vital parameters and inflammatory markers, and weaning from the ventilator and inotropes was possible after 48 hours. The remaining time in hospital was uneventful.
CONCLUSIONS: This report supports the findings from recent studies and reports that extracorporeal cytokine hemoadsorption has a role to play in reducing the systemic effects of cytokine storm associated with complex surgery involving cardiopulmonary bypass alongside severe infections, including COVID-19.
Keywords: Thoracic Surgery, COVID-19, Male, Humans, Adult, Marfan Syndrome, COVID-19, Aortic Valve Insufficiency, Aorta, Cytokines
Background
Patients with COVID-19 may have to undergo urgent surgical procedures under general anesthesia. Such patients are at increased risk of developing perioperative complications, often related to a dysregulated immune response, hyperinflammation, and vasoplegia [1]. In addition, specific protective measures need to be undertaken to protect the operating theater staff, leading to further complexity in already dire circumstances [2]. Extracorporeal cytokine hemoadsorption is an emerging technology utilized in the treatment of dysregulated inflammatory states, such as sepsis [3], but has also been shown to be beneficial in high-risk patients, especially in cardiac surgery [4,5]. By using adjunctive hemoadsorption, the perioperative cytokine release can be attenuated. CytoSorb is an extracorporeal cytokine hemoadsorption device with a bio-compatible sorbent designed to remove inflammatory mediators from the bloodstream [6]. By effectively reducing cytokine levels, CytoSorb aims to mitigate the harmful effects of excessive inflammation [6], known as cytokine storm, which can contribute to organ dysfunction and mortality in conditions such as sepsis, acute respiratory distress syndrome, and other hyperinflammatory states including COVID-19 [7–10]. We herein report on a male patient with COVID-19 infection who required an urgent redo replacement of the aortic valve and aorta due to aortic aneurysm of the ascending aorta (Bentall procedure) associated with Marfan syndrome, who was treated with extracorporeal cytokine hemoadsorption. The aim of this report is to present the potential benefit of preventive use of adjunctive hemoadsorption in a high-risk patient undergoing a complex procedure, to mitigate unfavorable postoperative outcomes. Informed consent was obtained from the patient.
Case Report
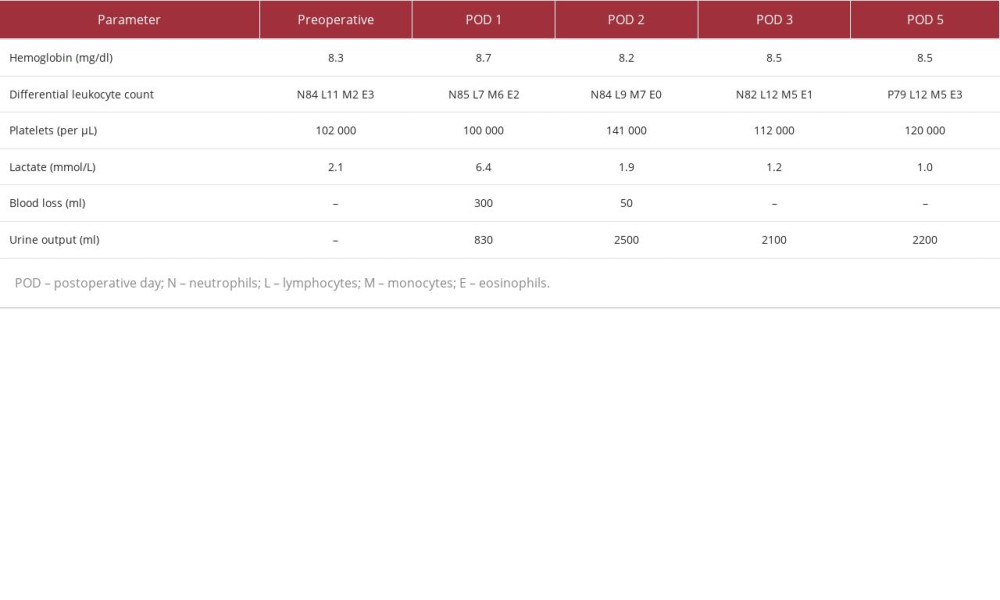
A 34-year-old man with known Marfan syndrome, who had undergone a Bentall procedure in 2018, was admitted with symptoms of worsening dyspnea (New York Heart Association class IV). On examination, he had tachycardia and fever and was suspected to have infective endocarditis. His vital parameters were: heart rate 118 beats/min, blood pressure 92/45 mmHg, peripheral oxygen saturation 85% on room air, and body temperature of 38.6°C. The real-time polymerase chain reaction test for COVID-19 was positive (ViralDtect-II Multiplex real-time PCR kit, Genes2Me). The patient was moved to a negative-pressure room in the intensive care unit (ICU). High-resolution computed tomography (CT) of the chest showed bilateral ground glass opacities with interlobular septal thickening and dependent consolidation. Transthoracic echocardiography showed a mechanical bileaflet prosthetic valve in the aortic position with suspected vegetations on the leaflets, dehiscence of the aortic root with a para-aortic abscess, and moderate aortic regurgitation; however, no pericardial effusion was seen. A CT aortogram revealed contrast leakage in the mediastinum adjacent to the aortic valve and the aortic root (Figure 1). The rest of the ascending aorta, arch, and descending aorta were normal in caliber and thickness (Figure 2). Laboratory diagnostics showed anemia, leukocytosis, thrombocytopenia, high procalcitonin, and interleukin-6 (IL-6) (Table 1). Bacterial cultures were negative; however, meropenem and vancomycin were started empirically, and a remdesivir infusion (loading dose 200 mg IV, followed by 100 mg once/day) was initiated to prevent virus replication. Given the severity of symptoms, echocardiography findings, risk of aortic rupture, and risk of sudden death, urgent cardiac surgery was advised. The calculated EuroSCORE II was 10.82%. A negative-pressure operating room with an active scavenging system was used for the redo Bentall surgery. Standard cardiac monitoring consisted of invasive arterial pressure, pulmonary artery catheter, transesophageal echo-cardiography, and cerebral oximetry. Cardiopulmonary bypass was instituted after cannulation of the axillary artery and fem-oral vein. Myocardial protection was achieved by moderate hypothermia, antegrade Custodiol® crystalloid cardioplegia (Dr. F. Köhler Chemie, Bensheim, Germany), and alpha-stat blood gas management. A CytoSorb® (CytoSorbents Inc., Princeton, NJ, USA) hemoadsorber was additionally integrated into the cardiopulmonary bypass circuit to attenuate the anticipated systemic hyperinflammation. The hemoadsorber was used for the entire duration of the cardiopulmonary bypass procedure. The surgical procedure consisted of redo sternotomy, thorough cleaning of the pus from the para-aortic region, extraction of the previous valve graft (23 mm SJM™ mechanical valve graft, SJM, Little Canada, MN, USA), creation of a neo-annulus using glutaraldehyde-treated bovine pericardium, and a redo Bentall procedure using a porcine root (25 mm Freestyle™ bioprosthesis, Medtronic Inc, Minneapolis, Minnesota, USA) as shown in Figure 3.
Intraoperatively, no evidence of infective endocarditis was seen. Aortic-cross clamp time was 165 min and cardiopulmonary bypass duration was 191 min. During the procedure, epinephrine (0.05 µg/kg/min) and norepinephrine (0.3 µg/kg/min) were administered for inotropic support. Intraoperatively, the patient required 10 units of red blood cells, 6 units of fresh frozen plasma, and 4 units of platelet apheresis transfusion due to excessive bleeding from the friable tissues and the pre-existing anemia and thrombocytopenia. Postoperatively, the patient was transferred back to the negative-pressure ICU room and was weaned from the ventilator and inotropes after 48 hours. Inflammatory markers (Figure 4) and hemodynamic parameters (Figure 5) showed a marked improvement after postoperative day 2 (Table 1). The remaining time in hospital was uneventful.
Discussion
This report supports the findings from recent studies and reports that extracorporeal cytokine hemoadsorption has a role to play in reducing the systemic effects of the cytokine storm associated with complex cardiopulmonary bypass-assisted cardiac surgery and severe infections, including COVID-19. The intra- and postoperative clinical course was good and clinical outcomes were deemed favorable despite the severity of the patient’s condition.
Previous studies in patients with aortic and valvular surgeries have also shown attenuation of the inflammatory response and removal of key cytokines with the use of CytoSorb [11–13].
COVID-19 infection causes significant damage to the cardiovascular system [14,15]. The cardiovascular complications of COVID-19 infection include, but are not limited to, aortic dissection, acute pericarditis, left ventricular failure, acute coronary syndrome, myocardial infarction, and thromboembolic events [14,15]. In critically ill COVID-19 patients with sepsis and superimposed bacterial infection, controlling the inflammatory response may be as important as targeting the virus [16]. A recent systematic review and meta-analysis has shown that COVID-19-positive patients undergoing cardiac surgery have a long postoperative length of stay in the ICU and hospital and overall poor outcomes with high morbidity and mortality [1]. The poor outcome in these patients may result from elevated metabolic demand caused by systemic inflammation combined with hypoxia caused by pneumonia, leading to endothelial dysfunction and myocardial damage [1]. The systemic inflammatory response associated with COVID-19, with its release of pro-inflammatory cytokines, should theoretically benefit from the use of CytoSorb hemoadsorption therapy. Published results are heterogeneous; however, the most recent publications with the largest number of COVID-19 patients analyzed so far report improved outcomes in patients treated with CytoSorb therapy [17,18].
Early signs for a potential benefit of CytoSorb in COVID-19 came from a case series with 10 patients treated during the initial phase of the pandemic. Besides a significant decrease in IL-6 plasma concentrations, a clear improvement was also found in lactate levels as well as the hemodynamic situation, while there were no significant changes found in red blood cell counts, white blood cell counts, or platelets, which is in line with the findings in our patient [19].
In addition, the high-risk nature of this patient, as indicated by the high EuroSCORE, the need for redo aortic surgery, the physiological and inflammatory stresses associated with the cardio-pulmonary bypass, an anticipated prolonged cardiopulmonary bypass duration, and the fact that it was an emergency, made it a suitable case for the use of the CytoSorb adsorber. In this regard, there is a good body of evidence on the beneficial prophylactic use of intraoperative CytoSorb hemoadsorption in patients undergoing invasive high-risk cardiothoracic procedures [11,20–23]. Besides other effects, these studies show an attenuation in the severity of postoperative sepsis [20], improved lung function and shortened duration of ventilator use411,21], mitigated inflammatory response [24], accelerated recovery of multiorgan and microcirculatory dysfunction [22], improved hemodynamic stability [23], and reduced sepsis-associated mortality [20,23]. Of note, based on a previous study [11] in which the majority of patients also underwent the Bentall procedure, the authors have already had a good experience with CytoSorb working well, in line with the previously observed outcomes. Also in the study by Saller et al, around 40% of patients underwent the Bentall procedure [13]. However, the patient described herein had a substantially higher risk of complications than those in the Saller et al study, due to the ongoing viral infection and the fact that the surgery was a redo.
Concerning limitations of our report, we are well aware of the fact that administration of multiple medications and the transfusion of blood products perioperatively might have influenced the measurements to a certain degree. Additionally, due to the nature of a case report, no control measurements can be used for comparison.
Conclusions
We observed control of hyperinflammation in a COVID-19 patient requiring urgent redo complex cardiac surgery. Despite the severity of the patient’s condition, the intra- and postoperative clinical course was good, and clinical outcomes were deemed favorable, potentially associated with intraoperative CytoSorb treatment. Further research showing the beneficial effects of hemoadsorption in complex cardiac surgery complicated by COVID-19 infection may be helpful.
Figures
References:
1.. Gupta AK, Leslie A, Hewitt JN, Cardiac surgery on patients with COVID-19: A systematic review and meta-analysis: ANZ J Surg, 2022; 92(5); 1007-14
2.. Setlur R, Jaiswal A, Jahan N, Preventing exposure to COVID-19 in the operation theatre and Intensive Care Unit: J Anaesthesiol Clin Pharmacol, 2020; 36(Suppl. 1); S127-S33
3.. Hawchar F, Rao C, Akil A, The potential role of extracorporeal cytokine removal in hemodynamic stabilization in hyperinflammatory shock: Biomedicines, 2021; 9(7); 768
4.. Haidari Z, Demircioglu E, Boss K, Intraoperative hemoadsorption in high-risk patients with infective endocarditis: PLoS One, 2022; 17(7); e0266820
5.. Boss K, Jahn M, Wendt D, Extracorporeal cytokine adsorption: Significant reduction of catecholamine requirement in patients with AKI and septic shock after cardiac surgery: PLoS One, 2021; 16(2); e0246299
6.. Jansen A, Waalders NJB, van Lier DPT, CytoSorb hemoperfusion markedly attenuates circulating cytokine concentrations during systemic inflammation in humans in vivo: Crit Care, 2023; 27(1); 117
7.. Ruiz-Rodríguez JC, Molnar Z, Deliargyris EN, The use of CytoSorb therapy in critically ill COVID-19 patients: Review of the rationale and current clinical experiences: Crit Care Res Pract, 2021; 2021; 7769516
8.. Napp LC, Bauersachs J, Extracorporeal hemoadsorption: An option for COVID-19-associated cytokine storm syndrome: Shock, 2020; 54(5); 700-1
9.. Ronco C, Bagshaw SM, Bellomo R, Extracorporeal blood purification and organ support in the critically ill patient during COVID-19 pandemic: Expert review and recommendation: Blood Purif, 2021; 50(1); 17-27
10.. Chang K, Li Y, Qin Z, Effect of extracorporeal hemoadsorption in critically ill patients with COVID-19: A narrative review: Front Immunol, 2023; 14; 1074465
11.. Mehta Y, Singh A, Singh A, Modulating the inflammatory response with hemadsorption (CytoSorb) in patients undergoing major aortic surgery: J Cardiothorac Vasc Anesth, 2021; 35(2); 673-75
12.. Trager K, Skrabal C, Fischer G, Hemoadsorption treatment of patients with acute infective endocarditis during surgery with cardiopulmonary bypass – a case series: Int J Artif Organs, 2017; 40(5); 240-49
13.. Saller T, Hagl C, Woitsch S, Haemadsorption improves intraoperative haemodynamics and metabolic changes during aortic surgery with hypothermic circulatory arrest: Eur J Cardiothorac Surg, 2019; 56(4); 731-37
14.. Xie Y, Xu E, Bowe B, Long-term cardiovascular outcomes of COVID-19: Nat Med, 2022; 28(3); 583-90
15.. Ramandi A, Akbarzadeh MA, Khaheshi I, Aortic dissection and COVID-19; A comprehensive systematic review: Curr Probl Cardiol, 2023; 48(6); 101129
16.. Tay MZ, Poh CM, Renia L, The trinity of COVID-19: Immunity, inflammation and intervention: Nat Rev Immunol, 2020; 20(6); 363-74
17.. Jarczak D, Roedl K, Fischer M, Effect of hemadsorption therapy in critically ill patients with COVID-19 (CYTOCOV-19): A prospective randomized controlled pilot trial: Blood Purif, 2023; 52(2); 183-92
18.. Alavi Darazam I, Kazempour M, Pourhoseingholi MA, Efficacy of hemoperfusion in severe and critical cases of COVID-19: Blood Purif, 2023; 52(1); 8-16
19.. Peng JY, Li L, Zhao X, Hemoperfusion with CytoSorb® in critically ill COVID-19 patients: Blood Purif, 2022; 51(5); 410-16
20.. Haidari Z, Leiler S, Mamdooh H: Interdiscip Cardiovasc Thorac Surg, 2023; 36(1); ivad010
21.. Doukas P, Hellfritsch G, Wendt D, Intraoperative hemoadsorption (Cytosorb™) during open thoracoabdominal aortic repair: A pilot randomized controlled trial: J Clin Med, 2023; 12(2); 546
22.. Soltesz A, Molnar ZA, Szakal-Toth Z, Influence of venoarterial extra-corporeal membrane oxygenation integrated hemoadsorption on the early reversal of multiorgan and microcirculatory dysfunction and outcome of refractory cardiogenic shock: J Clin Med, 2022; 11(21); 6517
23.. Manohar M, Jawali V, Neginahal S, Hemoadsorption in complex cardiac surgery – a single center experience: J Clin Med, 2022; 11(23); 7005
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250