18 September 2023: Articles 
Large Pericardial Effusion Secondary to Generalized Myxedema from Undiagnosed Hashimoto’s Thyroiditis
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Rare coexistence of disease or pathology
Gabriel Velez-Oquendo1E*, Vikas Kilaru1E, Kara YeDOI: 10.12659/AJCR.940631
Am J Case Rep 2023; 24:e940631
Abstract
BACKGROUND: Pericardial effusions are considered to be present when accumulated fluid within the pericardial sac exceeds the small amount that is normally present, causing impairment in the diastolic filling of the right heart. This case demonstrates an uncommon presentation of a large pericardial effusion by showing its relationship to myxedema in a patient with untreated hypothyroidism.
CASE REPORT: A 42-year-old man with a past medical history of hypertension, diabetes mellitus, and opioid abuse presented to the emergency department due to altered mental status, for which he received Narcan without resolution of symptoms. Computed tomography (CT) of the brain was without any acute intracranial abnormalities to explain the patient’s altered mental status. CT chest reported a pericardial effusion, with a subsequent transthoracic echocardiogram (TTE) showing a moderate-to-large circumferential effusion without right atrial/ventricular collapse and no cardiac tamponade physiology. On further investigation, he was found to have severe hypothyroidism with elevated thyroid peroxidase antibodies. Endocrinology was consulted to start IV levothyroxine and liothyronine to treat autoimmune Hashimoto’s thyroiditis. Subsequent TTE after starting hypothyroidism treatment showed an ejection fraction (EF) of 45-50% with mildly reduced left ventricular systolic function and moderate-to-large pericardial effusion, with no evidence of tamponade physiology. After treatment of hypothyroidism, the thyroid panel, EF, and pericardial effusion improved significantly.
CONCLUSIONS: This case illustrates the potential for suffering a large pericardial effusion secondary to generalized myxedema in a patient with severe hypothyroidism from undiagnosed Hashimoto’s thyroiditis. It is important to recognize this condition for appropriate therapy and prevention of worsening cardiac conditions.
Keywords: Hashimoto disease, Hypothyroidism, Myxedema, Pericardial Effusion, Male, Humans, Adult, thyroxine
Background
The pericardial space normally contains a few milliliters of fluid that acts as a lubricant between the inner and outer pericardial tissue, but diseases and/or conditions such as pericarditis, myocardial infarction, and metabolic disturbances can lead to the pericardium filling with hundreds of milliliters of exudative or transudative fluid [1]. This is called a pericardial effusion, which can be easily recognized with multimodal imaging strategies like a chest X-ray (which can show an enlarged cardiac shadow when a significant pericardial effusion is present), computed tomography of the chest (CT chest), and/or transthoracic echocardiographic (TTE) imaging [1].
Physiologically, the pericardial fluid is formed by ultrafiltration that occurs at the site of the pericardial capillaries [2]. Most of the fluid is normally reabsorbed at the venous end, and some of the retained fluid is drained out via lymphatic drainage [2]. Any underlying condition such as hypothyroidism can cause inflammation inside the pericardial cavity, leading to increased fluid accumulation and thus causing pericardial effusion [2]. The severity of pericardial effusion secondary to hypothyroidism is dependent on the progression and severity of the disease. Therefore, pericardial effusions are frequently found in generalized myxedema, which occurs in a more severe stage of hypothyroidism [2]. To evaluate these patients, a chest X-ray and electrocardiogram (ECG) are considered. Abnormalities in the chest X-ray and the ECG are further investigated by an echocardiogram and/or CT of the chest. According to guidelines, pericardial effusion should be managed by treating the underlying etiology [3]. For patients with myxedema coma, it is suggested to start combined therapy with levothyroxine and liothyronine, as performed in this patient’s medical treatment.
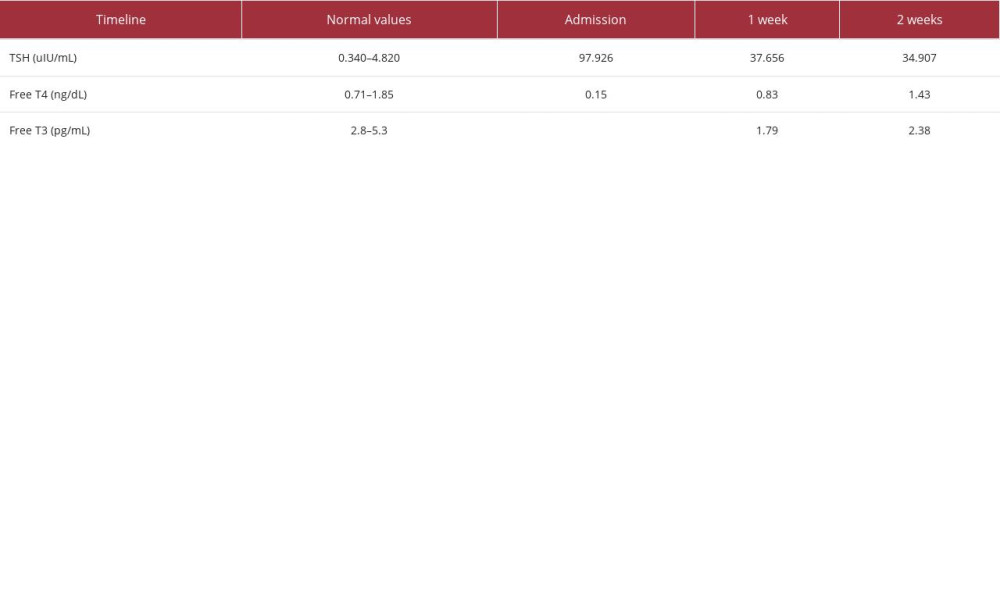
Monitoring a patient’s cardiovascular system after starting treatment for severe hypothyroidism secondary to Hashimoto’s thyroiditis is important in the setting of increasing serum thyroid hormone concentrations, which can precipitate the risk of dysrhythmias. Serum Free T4 and T3 should be measured every 1–2 days to confirm that the therapeutic regimen is working [3]. Serum thyroid-stimulating hormone (TSH) typically falls at a rate of approximately 50% per week in hypothyroid patients receiving a full replacement dose of thyroid hormone [3]. Failure of the serum TSH to fall accordingly is an indication of inadequate therapy. Clinical and biochemical improvement are typically evident within 1 week, as noted in this patient’s case.
In this case report we present a patient without a known past medical history of autoimmune disorders, who presented to the emergency department with a diagnosis of myxedema coma, suffering from a large pericardial effusion, who received treatment for the underlying etiology, and echocardiography started to show improvement in the fluid collection.
Case Report
A 42-year-old man with a past medical history of longstanding hypertension, uncontrolled diabetes mellitus type II with recurring A1c level >9%, progressive weight gain, generalized edema, and opioid use disorder on Buprenorphine/naloxone combination medical treatment presented to the emergency department due to altered mental state and lethargy, for which he received Narcan, without resolution of symptoms. His blood pressure was 116/67 mmHg, heart rate was 65 beats/min, oxygen saturation was 99% on 3 L of oxygen supplementation, and his body temperature was 36.4°C. A physical exam was noticeable for dry mucous membranes, bilateral eye drainage, distant heart sounds, distended abdomen, and bilateral lower-extremity erythema.
Laboratory testing revealed an elevated TSH level (97.926 uIU/ml), decreased free T4 (0.15 ng/dL), decreased free T3 (<0.20 pg/mL), elevated high-sensitivity troponin I (254 ng/L), ammonia level <10u/dL, N-terminal proBNP 1493 pg/mL, and a negative urine drug screening test. The initial electrocardiogram (ECG) showed sinus rhythm with low-voltage QRS (Figure 1). A CT brain was negative for any acute intracranial abnormalities to explain the patient’s altered mental status. Chest radiography showed an enlarged cardiac silhouette (Figure 2). Consequently, a CT of the chest without contrast showed a moderate-to-large pericardial effusion (Figure 3), which prompted further investigation.
Following the results of the chest CT showing a large pericardial effusion, a transthoracic echocardiogram (TTE) was performed. The TTE showed an estimated ejection fraction (EF) of 45–50%, with mildly reduced left ventricular systolic function, normal diastolic function, no right ventricular or right atrial collapse, and a large pericardial effusion (approximately 20 mm in size), without evidence of cardiac tamponade (Figure 4). On further laboratory investigation, the patient’s thyroid-stimulating hormone was found to be significantly elevated, with severely decreased free T4 and free T3 (Table 1). An ABG on admission showed acidosis (pH 7.324), hypercapnia (pCO2 53.8), and normal HCO3 (27.9). Subsequently, the patient was intubated for airway protection due to metabolic encephalopathy causing the patient to have an ineffective airway.
Subsequent work-up showed negative blood cultures, and negative test results for influenza, COVID-19, and respiratory syncytial virus, but showed elevated thyroid peroxidase antibodies (5649 U/mL) consistent with autoimmune Hashimoto’s thyroiditis, and a positive glutamic acid decarboxylase antibody assay; unfortunately, an ultrasound of the thyroid gland was not performed. Endocrinology was consulted to start the patient on treatment with intravenous levothyroxine (50 mcg every 6 h), liothyronine (2.5 mcg every 8 h), and hydrocortisone (25 mg every 6 h). A TTE 1 week later showed an ejection fraction (EF) of 45–50% with mildly reduced left ventricular systolic function and moderate circumferential pericardial effusion, with no evidence of tamponade physiology. At this time, steroids and liothyronine were discontinued and the patient was started on oral levothyroxine 200 mcg daily. With continued treatment of the patient’s hypothyroidism, his thyroid hormone levels improved, as expected. A final TTE showed an improved ejection fraction of 50–55%, normal systolic function, and a smaller pericardial effusion compared to prior studies (Figure 5). ECG on discharge continued showing normal sinus rhythm with low-voltage QRS (Figure 6). Guideline-directed medical therapy was started and the patient remained stable from a cardiac standpoint upon discharge.
The patient had an outpatient follow-up visit as he continued to experience shortness of breath on exertion, and generalized edema despite being compliant with his medication. He did not report any acute symptoms or changes in his condition.
Since discharge, he had an unremarkable course from a cardiology standpoint, with no new complications or deterioration in his condition. Physical exam was unremarkable other than bilateral trace pedal edema. ECG showed normal sinus rhythm, low-voltage QRS, and nonspecific T wave abnormalities, which were unchanged from previous tests done during the hospital course. A repeat echocardiogram was scheduled for 6 months to monitor for recurrent pericardial effusion, but the patient died soon afterward due to unknown causes and/or information about the cause of death on the chart.
Discussion
Conditions such as hypothyroidism can affect pericardial fluid homeostasis, in which the pericardial space fills with exudative or transudative fluid, leading to pericardial effusion [1]. Pericardial effusions can have a gradual or rapid onset, with the latter encountered in more emergent settings due to the inability of the fibrous pericardium to stretch and accommodate an increase in fluid volume [3]. Non-inflammatory etiologies of pericardial effusions include congestive heart failure, direct pericardial injuries, or metabolic abnormalities such as hypothyroidism, as in this case [4,5].
Hypothyroidism occurs when the thyroid gland becomes hypoactive and does not produce enough thyroid hormone. Hypothyroidism has several causes, including Hashimoto’s disease, thyroiditis, and primary thyroid disease, among others. Hashimoto’s disease, an autoimmune disorder, is the most common cause of hypothyroidism and is diagnosed by the presence of anti-thyroid peroxidase and anti-thyroglobulin antibodies [6]. When this condition goes unnoticed, patients can develop severe hypothyroidism and present with myxedema coma. Myxedema coma, a rare but lethal complication of hypothyroidism, classically presents with multiple-organ abnormalities and progressive deterioration in mental status [7].
In hypothyroidism, low intravascular oncotic pressure secondary to decreased albumin synthesis causes fluid extravasation into the interstitial space [7]. The preferred imaging modality to diagnose a suspected pericardial effusion and/or cardiac tamponade is echocardiography, as was performed in this patient [1,3].
The mainstay of treatment for myxedema coma is thyroid hormone replacement therapy, preferably combined with levothyroxine (T4) and liothyronine (T3). The typical initial dose of T4 is 200–400 mcg intravenously, followed by daily intravenous doses of 50–100 mcg. T3 is given intravenously at the same time; the initial dose is 5–20 mcg, followed by 2.5–10 mcg every 8 h. Serum T4 and T3 should be measured every 1–2 days to confirm that the therapy is working [8].
Once there is an improvement, the patient can be treated with oral T4 alone, with dosing determined based on body weight, age, coexistent cardiovascular disease, and the most recent intravenous dose, as was performed in this case. For our patient, glucocorticoids in stress doses were administered until the coexisting adrenal insufficiency was excluded [3].
Although this patient had a history of opioid use disorder, he had scheduled appointments with his primary care physician to maintain compliance with his treatment, which included Buprenorphine and naloxone. Additionally, the initial urine drug screen on admission was negative for any substances, and there was no response from intranasal naloxone. For such reasons, substance use disorder was not on the differential of a possible etiology of this patient’s diagnosed myxedema coma during hospitalization.
Management of the pericardial effusion in hemodynamically stable patients includes treating identifiable underlying etiologies such as hypothyroidism along with close follow-up with routine TTE, as illustrated in this case. Non-steroidal anti-inflammatory agents were not used as part of this patient’s medical management because etiologies such as pericarditis, direct cardiac injury, and inflammatory causes were low on the differential of this patient’s large pericardial effusion.
Conclusions
This case report demonstrates a patient with a past medical history of uncontrolled diabetes mellitus type 2 and previous opioid use disorder, who suddenly presented to the emergency department with an altered mental state, and a large pericardial effusion secondary to generalized myxedema from un-diagnosed hypothyroidism, in whom the effusion recovered by treating the underlying metabolic disturbance. This report highlights the complexity of the treatment and management of pericardial effusion in patients with generalized myxedema from Hashimoto’s thyroiditis.
In the setting of an increasing population suffering from metabolic disturbances and autoimmune conditions, it is important to screen for thyroid disorders in patients with signs of myxedema, and for pericardial effusions in severe hypothyroidism to prevent cardiovascular collapse.
Figures
References:
1.. Rehman I, Nassereddin A, Rehman A, Anatomy, thorax, pericardium.: StatPearls [Internet]., 2022, Treasure Island (FL), StatPearls Publishing [Updated 2022 Jul 25].
2.. Kaur H, Chakwop Ngassa H, Elmenawi KA, Hypothyroidism-related cardiac tamponade.: Cureus, 2021; 13(10); e18611
3.. Ross D, Myxedema coma. UpToDate. , 4 Oct. 2022, Www.uptodate.com
4.. Cremer PC, Kwon DH, Multimodality imaging of pericardial disease.: Curr Cardiol Rep, 2015; 17; 24
5.. Klein AL, Abbara S, Agler DA, American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: Endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography.: J Am Soc Echocardiogr, 2013; 26; 965-1012
6.. Tsang TS, Enriquez-Sarano M, Freeman WK, Consecutive 1127 therapeutic echocardiographically guided pericardiocenteses: Clinical profile, practice patterns, and outcomes spanning 21 years.: Mayo Clin Proc, 2002; 77; 429-36
7.. , Hypothyroidism (Underactive Thyroid)., U.S. Department of Health and Human Services. https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism#common
8.. Mincer DL, Jialal I, Hashimoto thyroiditis.: StatPearls [Internet]., 2023, Treasure Island (FL), StatPearls Publishing [Updated 2022 Jun 21].
Figures
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250