30 November 2023: Articles 
Uncommon Coexistence of Pleomorphic Adenoma and Warthin’s Tumor in a Painfully Swollen Left Parotid Gland: A Surgical Case Report
Rare coexistence of disease or pathology
Gilbert Georg Klamminger12BCDEF, Christian IssingDOI: 10.12659/AJCR.940985
Am J Case Rep 2023; 24:e940985
Abstract
BACKGROUND: Benign pleomorphic adenoma is the most common primary tumor of the salivary glands and mainly arises in the parotid gland. Warthin’s tumor, or papillary cystadenoma lymphomatosum, represents <30% of benign parotid tumors. The simultaneous occurrence of multiple parotid tumors is rarely described – depending on the corresponding histology (different/identical), the time of their occurrence (synchronous/metachronous), as well as their location (unilateral/bilateral), multiple parotid tumors can be further sub-classified.
CASE REPORT: We describe the case of a 54-year-old female patient with progressive and painful swelling of the left parotid gland for the last 6 months. During extra-oral examination, a bulging, displaceable mass of approximately 3 cm was determined. A subsequent MRI (magnetic resonance imaging) examination revealed a multifocal lesion but failed to provide a decisive clue as to the tumor entity of the lesion, and a lateral (superficial) parotidectomy was performed. Postoperative histomorphological interpretation allowed the final pathological diagnosis of synchronous, unilateral occurrence of a pleomorphic adenoma as well as a Warthin’s tumor.
CONCLUSIONS: This report presents a rare case of synchronous unilateral parotid tumors and supports that benign pleomorphic adenoma and Warthin’s tumor are the most common associations. Since clinical examination, MRI imaging, and even cytological assessment could be misleading in the detection of synchronous ipsilateral multiple parotid gland tumors, our report also highlights the importance of timely and accurate diagnosis with histopathology to plan surgery and to exclude malignant transformation, which is a rare but important association with both types of primary salivary gland tumor.
Keywords: Adenolymphoma, Adenoma, Pleomorphic, Pathology, Salivary Glands
Background
Only a small proportion of all tumors of the head and neck region occur in the salivary glands; however, up to 85% of these tumors are located within the parotid glands [1]. The benign epithelial lesions pleomorphic adenoma (PA) and Warthin’s tumor (WT), the latter named after A. Warthin who published 2 cases of
Although tumors of the salivary glands usually occur as solitary lesions, multiple parotid tumors have been reported in the literature [7–15]. Depending on the underlying patient population and therefore based on different incidences, multiple parotid tumors have been described with frequencies of 3.4% (Yu et al; cohort of 2055 patients, Peking) up to 5% (Ethunandan et al; cohort of 606 patients, Chichester) [11,13]. Terminologically and etiologically, a further characterization of the lesion(s) is made according to their time of development and appearance (synchronous/metachronous), according to their localization (bilateral/ipsilateral), as well as according to their distinct histological entity (identical/different) [16]. Here, we report the rare clinical case of a 54-year-old woman with a 6-month history of painful swelling of the left parotid gland due to synchronous benign pleomorphic adenoma and Warthin’s tumor.
Case Report
MEDICAL HISTORY AND CLINICAL PRESENTATION:
A 54-year-old female patient presented to the otorhinolaryngology clinic at the University Hospital (Goethe University, Frankfurt am Main, Germany) after reporting a history of a progressive and painful swelling of the left parotid gland for the last 6 months with a marked increase in size in recent weeks. The patient denied allergies or regular intake of medication. The extra-oral examination revealed a bulging, displaceable mass of the left parotid gland with a diameter of about 3 cm. The mass was located in the caudal part of the left parotid gland, and a small (<1 cm) inconspicuous lymph node was located in the immediate neighborhood. On palpation, the mass appeared solid, well-displaced, and not pressure-dolent. The overlying skin was intact and not pathologically altered. The ENT (ear, nose, and throat) status showed no signs of pathological affection; in particular, the function of the facial nerve was not affected. Despite a small inconspicuous lymph node in the left glandula parotidea, there were no pathologic lymph nodes or other lesions detected cervically. On the intra-oral examination, the oral mucosa was non-irritant except for minimal redness of the posterior pharyngeal wall, and the tonsils were small and regular. The dental status was unremarkable. An externally performed MRI scan of the neck showed a quasi-spherical mass, measuring 1.5×1.5×2 cm, with moderate contrast enhancement (T1 low-intensity and T2 high-intensity, compatible with a suspected diagnosis of WT) within the tail of the left parotid gland, as well as a small contrast-enhancing lesion in the middle part of the parotid gland (Figure 1) [17]. All other salivary glands showed no abnormalities in the MRI. At the second presentation in our clinic, the described mass was assessed by ultrasound, and a 1.4×1.2 cm homogeneous lesion was detected (Figure 2). After explaining conservative and surgical treatment options, the patient opted for a definite surgical procedure; accordingly, a lateral (superficial) parotidectomy was planned to remove the tumor, while sparing the facial nerve (VII). Intraoperatively, the multifocal occurrence of the lesion was acknowledged and 3 tissue fragments were sent from the operating room to pathology for histopathological evaluation. The specimens appeared beige-brownish on gross examination and originated intraparotidally from the left part of the parotid gland, the lower pole, and preauricularly from the left parotid gland.
On hematoxylin and eosin (H&E) staining, the tissue removed from the lower pole proved to be an encapsulated tumor with bilayered oncocytic epithelia based on a dense lymphoid stroma with germinal centers (Figure 3). The oncocytic epithelium did not show a distinct nuclear pleomorphism or marked hyperchromasia as signs of malignancy. Intermittently, cystic eosinophilic areas demarcated by an epithelial wall as well as granulomatous-appearing areas were found. Additively, small fragments of locoregional, lipomatous-altered, glandular tissue were removed. The histomorphological assessment of the preauricularly resected tissue fragment revealed resident glandular tissue adjacent to an encapsulated tumorous lesion (Figure 4). This specimen showed a multiform cellular pattern with both epithelial and mesenchymal differentiation of tumor cells; the tissue fraction contained predominantly densely packed myoepithelial cells adjacent to a myxoid stromal component. All the tumor cells showed no signs of dysplasia and no increased mitotic rate and no necrosis. There was no capsular rupture and no perineural infiltration. The intraparotideal tissue of the left side was a lymph node with reactive changes (not shown). Further molecular testing of both lesions to exclude mimickers was not performed. The pathology examination revealed the ipsilateral and simultaneous presence of a WT as well as a PA; therefore, the patient was diagnosed with ipsilateral, synchronous multiple parotid tumors with different histological characteristics. At the time of publication, the patient had neither clinical symptoms nor signs of recurrence. As a regular follow-up, a clinical and ultrasonographical examination once a year was recommended.
Discussion
PA and WT are common tumors of the parotid gland. Their synchronous and ipsilateral occurrence is a rare phenomenon in which clinical examination and various imaging techniques can be misleading. Our case report reflects the importance of a timely and accurate diagnosis with histopathology that can ultimately rule out the presence of malignant transformation.
The simultaneous detection of a PA and a WT was described in 1974 for the first time [18]. Table 1 gives a literature overview of published cases and clinical information on unilateral synchronous PA and WT of the parotid gland within the last 30 years (1993–2023). Table 2 summarizes statistical surveys in which the explicit combination of PA and WT is depicted. Overall, the literature provides different information on the localization and frequency of multiple salivary gland tumors in general. Depending on the cohort, a preferred occurrence of multiple parotid tumors has been reported both ipsilaterally (67%, Ethunandan et al analyzed 650 tumors of 606 patients of 617 parotidectomies removed with oncological indication in Chichester, United Kingdom), as well as bilaterally (58%, Yu et al screened 2055 patients with parotid tumors and determined 69 multiple primary tumors of the parotid gland at the University School of Stomatology, Peking, China). In either case the vast majority of multiple neoplasms of the parotid gland are identical in histology, namely WT [11,13]. However, simultaneous occurrence of multiple parotid tumors of different entities is rare and clinical experience on this subject is largely based on single case reports [7–10,18]. In such cases the tumors are, considering their high prevalence, ordinarily a combination of WT and PA [11,13,18].
Although clinical diagnosis by imaging methods such as MRI and ultrasound is usually successful in locating and assessing the malignant potential of singular/bilateral lesions of the parotid glands, the difficulty of correct preoperative radiological assessment of multiple ipsilateral parotid tumors is well known [7,19]. A definitive diagnosis is usually made only during histological tissue examination, as in the present case [7,11]. It should be emphasized that even a correct preoperative determination of a single tumor entity by means of fine-needle aspiration cytology (FNAC) can be misleading in patients with multiple tumors with different histology, as the second intact tumor entity in situ cannot be taken into account by the pathologist [7,8]. In our case, non-invasive imaging (MRI) but no FNAC or other histological confirmation was performed prior to surgery, because even in benign tumors of the salivary glands, the masses including their capsule should be completely removed to avoid recurrences. Despite the advantage of early histological confirmation of a malignant finding, carryover of single tumor cells could occur due to the FNAC procedure. Furthermore, even with a benign FNAC finding, malignancy cannot be ruled out with absolute certainty due to the small sample size. Therefore, the further procedure of surgical resection would not necessarily change depending on the result of the FNAC. Finally, previous sampling could cause scarring, which potentially complicates subsequent surgery [20,21]. In 2018, Heine et al reported 2 cases of synchronous unilateral PA and WT. Instead of using FNAC, they employed elastography (Virtual Touch Imaging Quantification, VTIQ) as an additional diagnostic tool. In this way, the physical stiffness, which can be used as a potential marker for malignancy, was successfully assessed and interpreted prior to surgery [22].
In the course of multiple parotid tumors, a possible combination of a benign neoplasm with a malignant lesion, in most of the cases a Warthin tumor and mucoepidermoid carcinoma, should be considered [22,23]. Ochal-Choinska et al provided a comprehensive literature overview of known cases of simultaneous, unilateral parotid gland tumors of benign and malignant histology [24]. Whether multiple parotid tumors are more frequently associated with 2 benign entities (Ethunandan et al) or with a combination of a benign tumor entity and a malignant tumor entity (Seifert et al, Yu et al, Zeebregts et al, Schilling et al) has not yet been clearly established [11,13,14,16,25].
In the constellation of multiple parotid tumors, each case remains an individual course until the final histopathological diagnosis postoperatively. Thus, 3 synchronously occurring tumor entities with individual malignancy potential, namely a PA, a WT and a salivary duct carcinoma, have already been described within the parotid gland and successfully treated by surgery and postoperative radiotherapy [26]. In our case of a WT and a PA, the therapeutic approach of choice was a complete surgical tumor resection. This is the first-line therapy in singular WTs/Pas and is also the treatment of choice in ipsi-lateral multiple parotid tumors with benign histology [5,8,18].
Conclusions
Our case report shows the rare phenomenon of synchronous occurrence of different tumor entities in the parotid gland. Our report further supports that the combination of PA and WT is the most common association. Since radiological imaging techniques and fine-needle aspiration do not allow for distinct diagnosis of underlying biological entities in these patients, a timely and accurate histomorphological analysis of all separate tumor specimens is important to determine treatment options and to exclude malignant transformation.
Figures
Tables
Table 1.. An overview of published cases of unilateral synchronous PA & WT of the parotid gland and their clinical details within the last 30 years (1993–2023). Other combinations of multiple parotid tumors with different histology were not considered.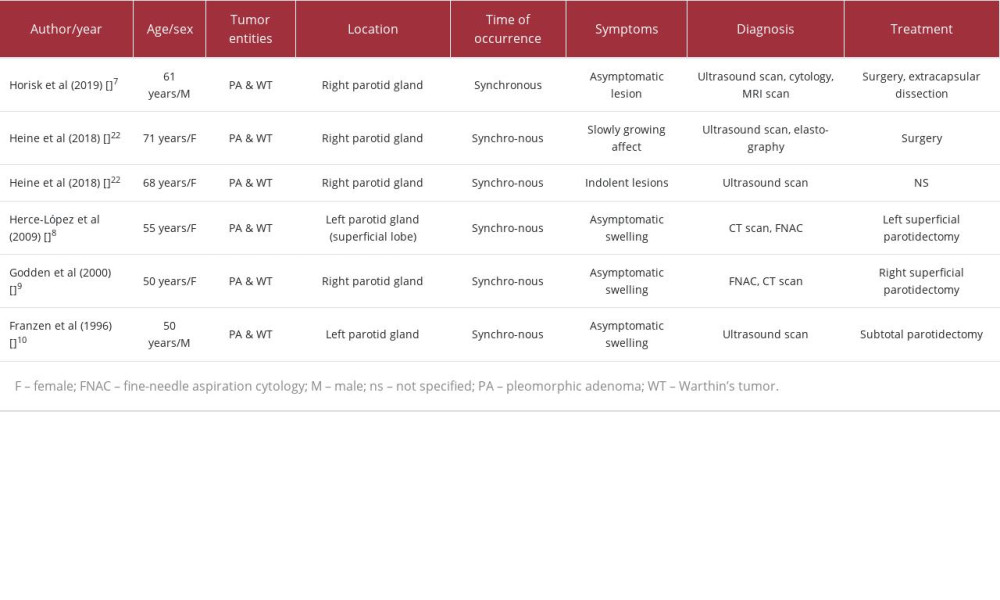 Table 2.. Recent statistical surveys in which the incidence of unilateral tumors of the parotid gland is referenced and the explicit combination of pleomorphic adenoma and Warthin tumor is documented.
Table 2.. Recent statistical surveys in which the incidence of unilateral tumors of the parotid gland is referenced and the explicit combination of pleomorphic adenoma and Warthin tumor is documented.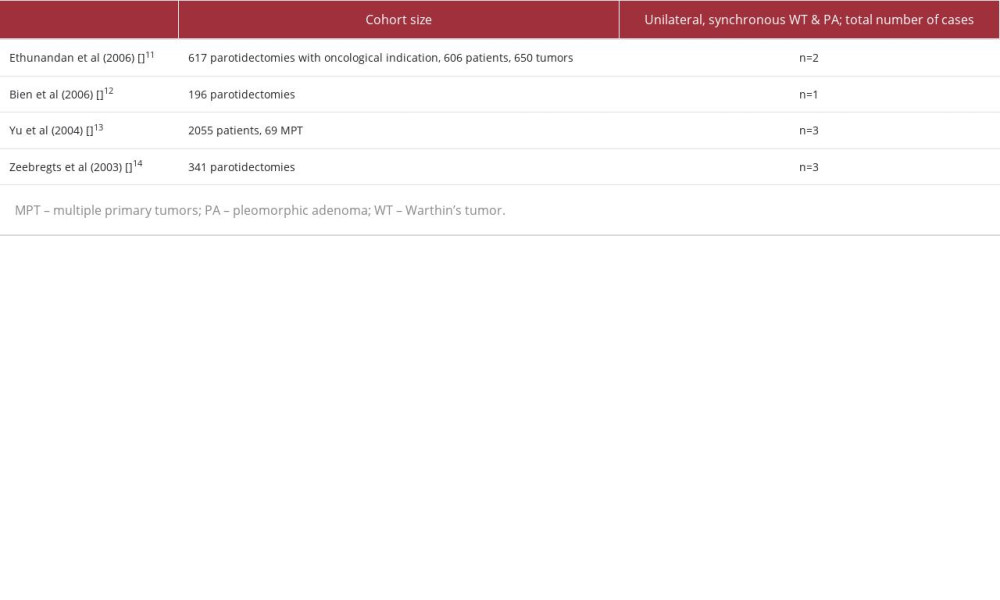
References:
1.. Speight P, Barrett A, Salivary gland tumours: Oral Dis, 2002; 8(5); 229-40
2.. Warthin AS, Papillary cyst adenoma lymphomatosum: A rare teratoid of the parotid region: J Cancer Res, 1929; 13(2); 116-25
3.. : Head and neck tumours, 2022, Lyon, International Agency for Research on Cancer
4.. Bradley PJ, McGurk M, Incidence of salivary gland neoplasms in a defined UK population: Br J Oral Maxillofac Surg, 2013; 51(5); 399-403
5.. El-Naggar AK, Chan JKC, Grandis JR: WHO Classification of Head and Neck Tumours, 2017, Lyon, International Agency for Research on Cancer
6.. Bokhari M, Greene J, Pleomorphic adenoma. [Updated 2022 Jul 4]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK430829/
7.. Horisk N, Stephenson E, Sayers C, Reid J, Incidental finding of synchronous pleomorphic salivary adenoma and Warthin’s tumour within a parotid gland: BMJ Case Rep, 2019; 12(4); e228675
8.. Herce-López J, Salazar-Fernández CI, Mayorga-Jiménez F, Synchronous unilateral parotid neoplasms. A case report: Med Oral Patol Oral Cir Bucal, 2009; 14(2); E90-92
9.. Godden DR, Akinmoladan VI, Warren A, Synchronous occurrence of 2 histo-logically distinct parotid neoplasms: J Oral Maxillofac Surg, 2000; 58(6); 680-81
10.. Franzen A, Koegel K, [Synchronous double tumors of the parotid gland]: Laryngorhinootologie, 1996; 75(7); 437-40 [in German]
11.. Ethunandan M, Pratt CA, Morrison A, Multiple synchronous and meta-chronous neoplasms of the parotid gland: The Chichester experience: Br J Oral Maxillofac Surg, 2006; 44(5); 397-401
12.. Bień S, Kamiński B, Kopczyński J, Sygut J, The synchroneous tumors of different histopathology in the parotid glands: Otolaryngol Pol, 2006; 60; 703-8
13.. Yu GY, Ma DQ, Zhang Y, Multiple primary tumours of the parotid gland: Int J Oral Maxillofac Surg, 2004; 33(6); 531-34
14.. Zeebregts CJ, Mastboom WJB, Noort G van, Det RJ van, Synchronous tumours of the unilateral parotid gland: Rare or undetected?: J Craniomaxillofac Surg, 2003; 31(1); 62-66
15.. Kajo K, Othman BK, Kajová Macháleková K, Sclerosing Warthin-like mucoepidermoid carcinoma of the salivary gland: Oral Oncol, 2022; 134; 106090
16.. Seifert G, Donath K, Multiple tumours of the salivary glands – terminology and nomenclature: Eur J Cancer B Oral Oncol, 1996; 32(1); 3-7
17.. Kim SY, Borner U, Lee JH, Magnetic resonance imaging of parotid gland tumors: A pictorial essay: BMC Med Imaging, 2022; 22(1); 191
18.. Astacio J, Papillary cystadenoma lymphomatosum associated with pleomorphic adenoma of the parotid gland: First case report: Oral Surg Oral Med Oral Pathol, 1974; 38(1); 91-95
19.. Kaleem A, Patel N, Alzahrani S, Concurrent presence of secretory carcinoma and Warthin’s tumor in ipsilateral parotid gland: Oral Oncol, 2020; 109; 104691
20.. Ramírez-Pérez F, González-García R, Hernández-Vila C, Is fine-needle aspiration a reliable tool in the diagnosis of malignant salivary gland tumors?: J Craniomaxillofac Surg, 2017; 45(7); 1074-77
21.. Shkedy Y, Alkan U, Mizrachi A, Fine-needle aspiration cytology for parotid lesions, can we avoid surgery?: Clin Otolaryngol, 2018; 43(2); 632-37
22.. Heine D, Zenk J, Psychogios G, Two case reports of synchronous unilateral pleomorphic adenoma and cystadenolymphoma of the parotid gland with literature review: J Ultrason, 2018; 18(75); 369-73
23.. Curry JL, Petruzzelli GJ, McClatchey KD, Lingen MW, Synchronous benign and malignant salivary gland tumors in ipsilateral glands: A report of two cases and a review of literature: Head Neck, 2002; 24(3); 301-6
24.. Ochal-Choińska A, Bruzgielewicz A, Osuch-Wójcikiewicz E, Synchronous multiple unilateral parotid gland tumors of benign and malignant histo-logical types: Case report and literature review: Braz J Otorhinolaryngol, 2019; 85(3); 388-92
25.. Schilling JA, Block BL, Speigel JC, Synchronous unilateral parotid neoplasms of different histologic types: Head Neck, 1989; 11(2); 179-83
26.. Tanaka S, Tabuchi K, Oikawa K, Synchronous unilateral parotid gland neoplasms of three different histological types: Auris Nasus Larynx, 2007; 34(2); 263-66
Figures
Tables
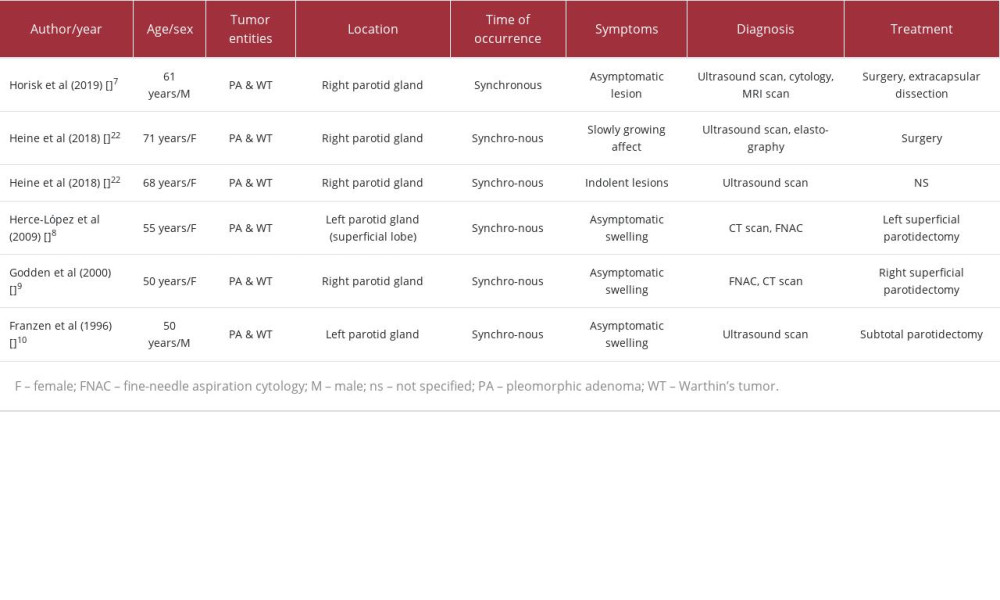 Table 1.. An overview of published cases of unilateral synchronous PA & WT of the parotid gland and their clinical details within the last 30 years (1993–2023). Other combinations of multiple parotid tumors with different histology were not considered.
Table 1.. An overview of published cases of unilateral synchronous PA & WT of the parotid gland and their clinical details within the last 30 years (1993–2023). Other combinations of multiple parotid tumors with different histology were not considered.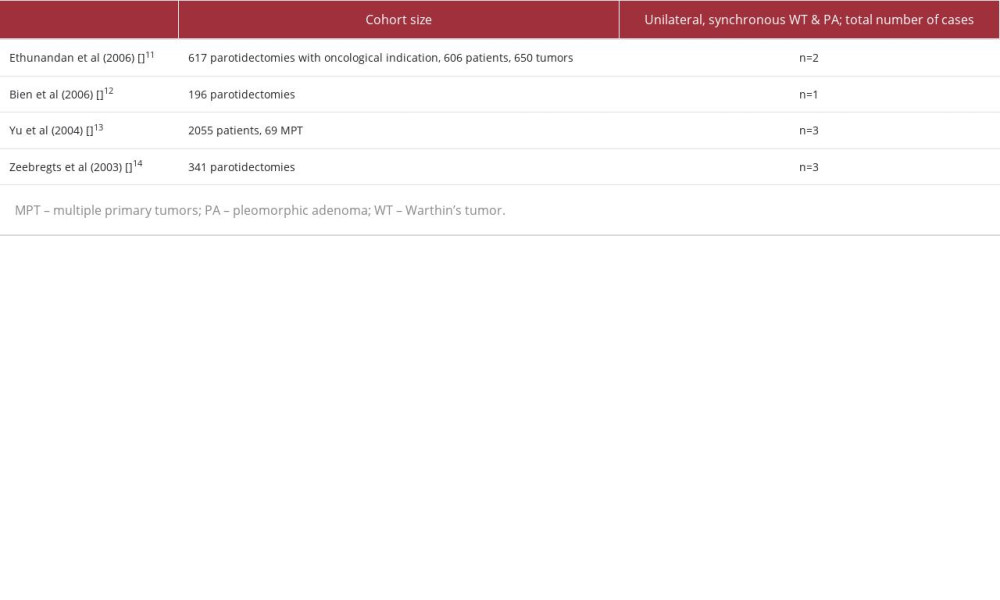 Table 2.. Recent statistical surveys in which the incidence of unilateral tumors of the parotid gland is referenced and the explicit combination of pleomorphic adenoma and Warthin tumor is documented.
Table 2.. Recent statistical surveys in which the incidence of unilateral tumors of the parotid gland is referenced and the explicit combination of pleomorphic adenoma and Warthin tumor is documented.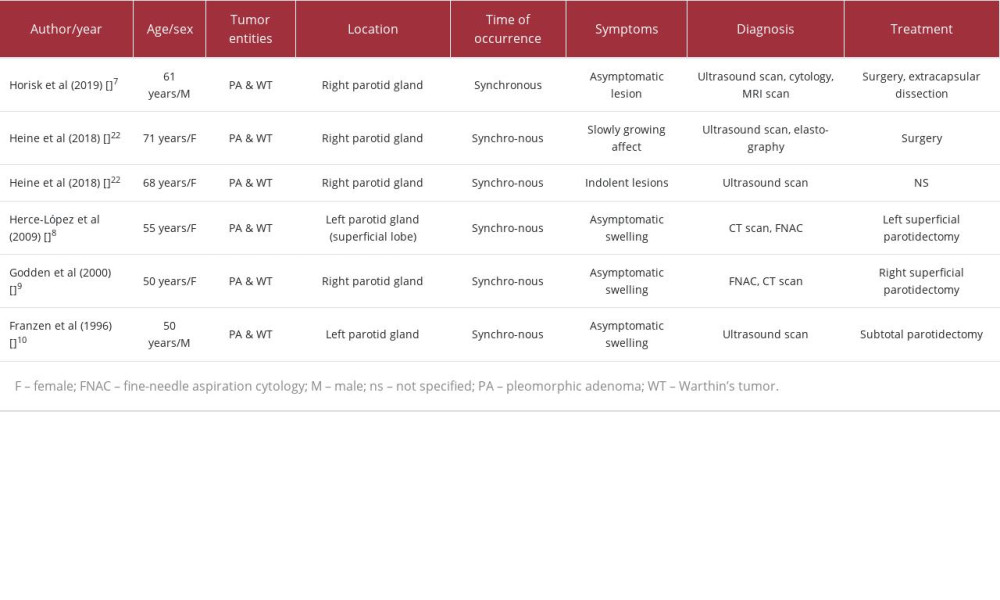 Table 1.. An overview of published cases of unilateral synchronous PA & WT of the parotid gland and their clinical details within the last 30 years (1993–2023). Other combinations of multiple parotid tumors with different histology were not considered.
Table 1.. An overview of published cases of unilateral synchronous PA & WT of the parotid gland and their clinical details within the last 30 years (1993–2023). Other combinations of multiple parotid tumors with different histology were not considered.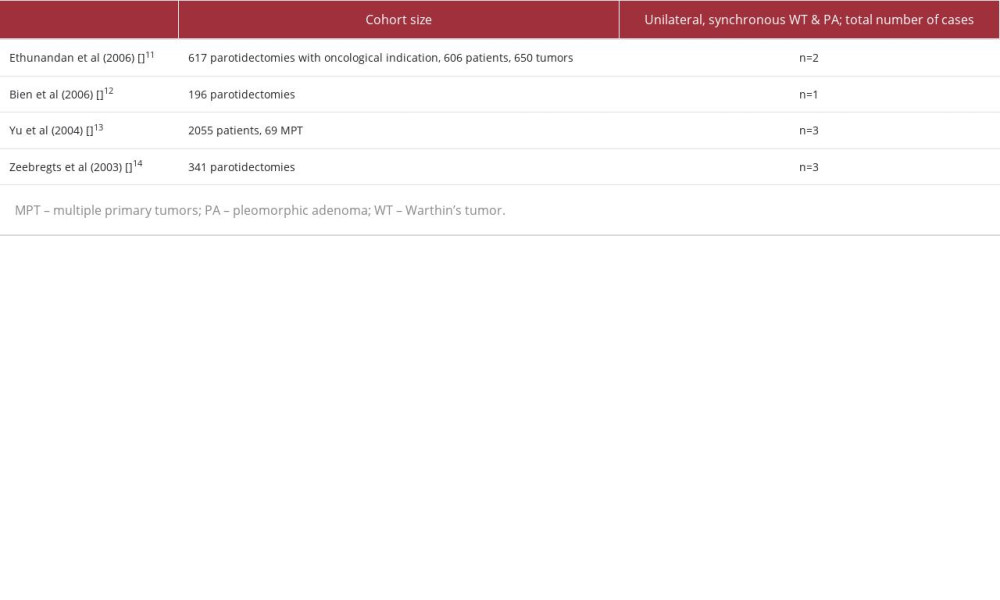 Table 2.. Recent statistical surveys in which the incidence of unilateral tumors of the parotid gland is referenced and the explicit combination of pleomorphic adenoma and Warthin tumor is documented.
Table 2.. Recent statistical surveys in which the incidence of unilateral tumors of the parotid gland is referenced and the explicit combination of pleomorphic adenoma and Warthin tumor is documented. In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








