15 December 2023: Articles 
Dermatofibrosarcoma Protuberans Occurring in an Adult Presenting with Chronic Lymphedema: A Case Study and Literature Review
Educational Purpose (only if useful for a systematic review or synthesis), Rare coexistence of disease or pathology
Clara Van Vyve1BCDEF*, Laurence Klein2AB, Ibrahim Kassem3BC, Jean LemaitreDOI: 10.12659/AJCR.941142
Am J Case Rep 2023; 24:e941142
Abstract
BACKGROUND: Dermatofibrosarcoma protuberans (DFSP) is a rare soft-tissue tumor typically located in the trunk. We report a unique case of DFSP in the right inguinal region of an adult presenting with chronic lymphedema. Only 1 case of DFSP and chronic lymphedema association has been previously reported in the literature. Since we could not provide adjuvant radiotherapy (RT), we conducted an extensive review of its application in similar cases, exploring various surgical treatments.
CASE REPORT: A 42-year-old Cameroonian man with unexplained chronic lymphedema presented with a tumor in the inguinal region of the affected limb. The patient underwent wide local excision (WLE) of the mass, including regional lymph node dissection. Pathological exam confirmed DFSP with a fibrosarcomatous component. Adjuvant RT was considered but not pursued due to the patient;s non-compliance.
CONCLUSIONS: This DFSP is reported for its rarity of site and the unique co-occurrence with chronic lymphedema. Considering both conditions are uncommon and the rarity of site of the DFSP, we assume that in this patient, chronic lymphedema was a contributing factor of occurrence of the DFSP. Remarkably, no prior reports have detailed an association between chronic lymphedema and DFSP onset. For that reason, we want to point out the value of better follow-up of chronic lymphedema and better knowledge of DFSP treatment options to improve patient healthcare and limit DFSP recurrence. In addition, we found adjuvant RT is an interesting treatment option that might be considered in all patients undergoing surgical excision, even in cases where negative surgical margins were achieved.
Keywords: Dermatofibrosarcoma, Non-Filarial Lymphedema, Radiotherapy Planning, Computer-Assisted
Background
DFSP is a rare slow-growing mesenchymal tumor affecting soft tissues and is mostly located in the trunk. According to Kreicher et al [1], only about 1% of DFSP are located on the genitals, about 20% are located on the lower limbs compared to 40% on the trunk. The tumor often presents as a skin-colored plaque or nodule on the skin. Around 90% are low-grade tumors, and the remaining 10% contains a fibrosarcomatous component (FSDFSP); they are “high-grade” tumors. The incidence of DFSP is estimated to 0.8 to 5 cases per 1 million people per year. DFSP is mostly encountered in young and middle-aged adults.
Elephantiasis is often due to lymph vessels blocked by filarial worms, but a lesser-known cause of chronic lymphedema is podoconiosis, a non-filarial elephantiasis. Podoconiosis is a multifactorial disease of which the inflammatory mechanisms and predisposing factors remain unclear. However, it is known that the disease is caused by an inflammatory reaction to red clay soil particles. In genetically susceptible individuals, the particles penetrate through the skin of the lower limbs. They are phagocytized by macrophages in the lymphatic system, causing inflammation, fibrosis, and occlusion of lymphatic vessels, eventually leading to chronic lymphedema [2].
Typical causes of DFSP remain unclear, although a suggested risk factor involves skin injury in the affected area [3]. Local immunodeficiency in the context of chronic lymphedema has been proposed as a factor that may facilitate the development of oncogenic processes [4], and this factor might influence cooccurrence of these rare disorders.
The association between DFSP and elephantiasis has only been described once in the literature in a case report by Singh et al [4], which described a 61-year-old woman with post-mastectomy lymphedema of the right upper limb. The patient presented with a 3-month history of a lump in the right breast and was diagnosed with an invasive carcinoma. The swelling appeared gradually after the patient underwent right modified radical mastectomy with right axillary clearance. A nodularity was noticed on the affected limb 5 years after treatment. A biopsy was done a year after the nodular lesion was first documented, and the pathological exam reported pigmented DFSP. P53 mutation was negative for both the primary breast malignancy and the DFSP. The authors suggested that it is possible that chronic lymphedema caused formation of the DFSP.
Here, we report a unique case of DFSP occurring in the inguinal region and affecting a limb presenting with chronic lymphedema. This article aims to highlight the significance of improving the follow-up for chronic lymphedema. We also want to encourage better understanding of DFSP treatment choices to improve patients’ healthcare and reduce the recurrence of DFSP.
Case Report
A 42-year-old Cameroonian man presented with a 3-year history of a mass in his right groin area. The patient also reported a 7-year history of elephantiasis in his right lower limb, which had never been treated or investigated (Figure 1). On examination, there was no sign of bacterial infection on the leg, and there was a lymphadenopathy in the right groin area.
The patient was treated for type II non-insulin-dependent diabetes, as well as high blood pressure and sleep apnea syndrome. The patient also had morbid obesity.
The serology test showed an absence of antibodies to filarial worms. Therefore, his elephantiasis was probably not due to a filarial cause. The primary origin of the chronic lymphedema was not further investigated, although the diagnosis of podoconiosis was not excluded. No additional treatment was administrated to the patient for his elephantiasis.
An ultrasound (US) showed a hypoechoic polylobulated mass of uncertain etiology on the inguinoscrotal region, well as several subcentimetric lymph nodes. The dimensions of the mass were 4.8 cm for the major axis and 2.9 cm for the minor axis.
The patient did not present for several months afterwards.
Five months after his US, an abdominal CT showed an exophytic mass of 9.2×1.1×7.7 cm and multiple swelled lymph nodes in the inguinal region. There was no sign of invasion of the vessels or the muscular structures.
We performed a wide local excision (WLE) and “en-bloc” re-section, removing the mass and the inguinal nodes. The surgical margins width was >1 cm. On analysis, no lymph node structure could be identified in view of numerous areas of necrosis, but these could explain the relative increase in mass compared to the CT scan. There was no invasion of the apo-neurosis macroscopically. After hemostasis and disinfection, 2 drains were inserted and there was no difficulty closing the incision. The scar healed well and the follow-up was uneventful.
The pathological exam (Figures 2, 3) of the mass was reported as DFSP with a fibrosarcomatous component of 18×11×6 cm. It was classified as pT4 R1. Tumoral cells were in frequent contact with resection edges. An immunohistochemistry test was reported positive for CD34, and we did not test factor XIIIa immunopositivity on the mass. Follow-up after 3 years remained uneventful.
It is worth noting that the patient had follow-up in another hospital after his surgery. We suggested a possible indication of first-line chemotherapy. However, the tumor board in Jules Bordet Oncological Institute opted for control MRI alone due to low risks of metastatic dissemination.
Discussion
An immunohistochemistry test was reported positive for CD34. CD34 is the most used antibody for the differential diagnosis between dermatofibroma (DF), a benign fibrohistiocytic tumor and DFSP, which has intermediate malignant potential [5,6]. Factor XIIIa is another marker of differential diagnosis between these tumors. Factor XIIIa immunopositivity was not tested in our case. An immunoprofile using antibodies to both CD34 and factor XIIIa is optimal for the distinction between DFs and DFSPs [5,7].
Articles have reported DFSP occurring in uncommon regions such as in the perianal region [8]. However, to the best of our knowledge, there is only 1 other case report of a dermatofibrosarcoma associated with chronic lymphedema. In that case, a woman with postmastectomy lymphedema presented with DFSP on the affected limb 5 years after the procedure [4]. Numerous similarities were found between this case and ours. Therefore, there is a possibility that the pathogenesis might also be similar, giving the rarity and uniqueness of cooccurrence of both disorders.
Local inflammation and immunity are managed by lymphatic vascularization. It was suggested that local immunodeficiency was associated with chronic lymphedema and thus could allow oncogenesis [4]. There is an alteration of local immune response caused by the collection of protein-rich interstitial fluid, which is also rich in growth factors [9]. It is also established that inflammation is correlated with the initiation and progression of cancer.
Thus, lymphedema could be a contributing factor for the development DFSP. However, these reports cannot be used to infer causation, and current scientific knowledge cannot explain how chronic lymphedema might constitute an essential part of the etiology of this tumor.
Concerning the current treatment options in DFSP, WLE and Mohs micrographic surgery (MMS) are standard therapies [10]. However, there is no consensus for WLE to establish standard safety margins. Multiple guidelines and research advocate using margins ranging from 1 to 5 cm [10,11,2]. We used a macroscopic margin width of >1 cm. Regarding MMS, if it is time consuming and difficult to perform on large masses, it is associated with maximal conservation of healthy tissue as well as a lower recurrence rate (1.5% for MMS compared to 8.8% for WLE [13]). It is therefore recommended for smaller wounds [13,14].
DFSP, and especially FS-DFSP, has a high recurrence rate, even after surgical excision. Data have shown the benefit of re-excision in patients who present with positive surgical margins, especially after R1 or marginal R0 resection [15]. However, in those patients, the proximity to critical anatomic structure may prevent re-excision. Adjuvant radiotherapy (RT) has been suggested to reduce the risk of local recurrence, particularly in those cases.
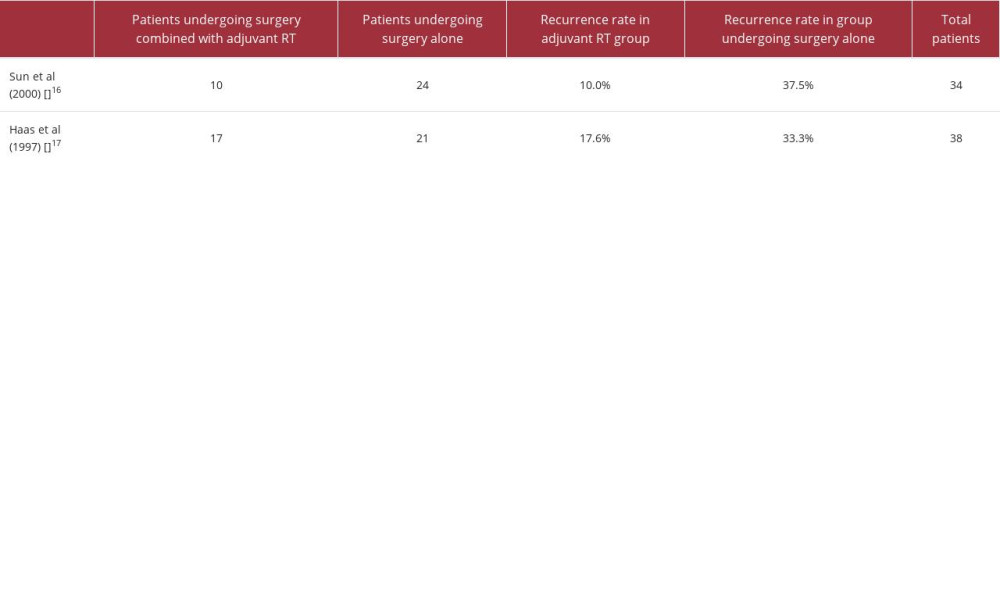
Two retrospective studies compared the recurrence rate in patients who received adjuvant RT vs patient who underwent surgery only [16,17]. Although the difference was not significant, the analysis showed that the recurrence rate was lower in surgery combined with adjuvant RT than surgery alone, as shown in Table 1, which shows a recurrence rate of 37.5% to 33.3% in the group undergoing surgery alone compared to 10% to 17.6% in the adjuvant RT group.
While multiple other studies reported very good control rates after adjuvant RT in cases with positive margins, a systematic review and meta-analysis of more recent findings by Chen et al [14] tried to establish more evidence-based information on the effectiveness of the technique. The paper reviewed 12 studies including 167 patients in total, all receiving adjuvant RT. The authors used surgical margin (positive/close or negative) as the variable of subgroup analysis. The recurrence rate was significantly higher in the subgroup with positive/close margins, showing the value of achieving negative margins. Although there was no recurrence in patients with negative margins, postoperative RT may still be recommended, especially because the risk of severe complications due to RT is considered low [13].
It is worth noting that the NCCN (National Comprehensive Cancer Network) guidelines suggest that close margins can be sufficient and therefore does not require re-excision if the patient undergoes postoperative RT [14]. In our case, the patient did not undergo postoperative RT after a decision was made by the tumor board in Jules Bordet Oncological Institute.
If results of RT as sole treatment remain unclear, it can be considered for unresectable lesions or if the resection would lead to unacceptable functional or cosmetic outcomes [7].
Another promising treatment for DFSP with significant response rates is a molecular targeted chemotherapy with imatinib mesylate, which is a protein tyrosine kinase inhibitor that has shown clinical activity against DFSP. In fact, imatinib mesylate targets tumors presenting a translocation between chromosomes 17 and 22 (t(17: 22)), which is what characterizes DFSP [10].
Conclusions
In conclusion, the etiopathogenesis of DFSP occurring in a chronic lymphedema territory needs more documentation to be fully understood. Factors that could link the 2 diseases include local immunodeficiency, induced by interstitial fluid rich in proteins and growth factors, and inflammation, which is known to be associated with the development and progression of cancer.
Only 1 case of DFSP and chronic lymphedema association were reported in the literature; therefore, we want to raise awareness of DFSP by reporting this case, showing how a territory of chronic lymphedema causes the formation of DFSP, and to encourage a better follow-up of patients with elephantiasis. However, adjuvant RT is an interesting treatment option that might be considered in all patients undergoing surgical excision, even in cases where negative surgical margins were achieved.
Figures
References:
1.. Kreicher K, Kurlander D, Gittleman H, Incidence and survival of primary dermatofibrosarcoma protuberans in the United States: Dermatol Surg, 2016; 42; S24-S31
2.. Wanji S, Deribe K, Minich J, Podoconiosis – from known to unknown: Obstacles to tackle: Acta Trop, 2021; 219; 105918
3.. Brooks J, Ramsey ML, Dermatofibrosarcoma protuberans. [Updated 2023 Apr 14]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK513305/
4.. Singh K, Backianathan S, Jennifer A, Dermatofibrosarcoma protuberans, lymphedema, and breast cancer: A rare association: Oncol J India, 2019; 3; 66-69
5.. Abenoza P, Lillemoe T, CD34 and Factor XIII a in the differential diagnosis of dermatofibroma and dermatofibrosarcoma protuberans: J Am Acad Dermatol, 1993; 15; 429-34
6.. Sadullahoglu C, Dere Y, Rezanko Atasever T, The role of CD34 and D2-40 in the differentiation of dermatofibroma and dermatofibrosarcoma protuberans: Turk Patoloji Derg, 2017; 33; 223-27
7.. Bichakjian C, Olencki T, Alam M, Dermatofibrosarcoma protuberans: Version 1.2014: J Natl Compr Canc Netw, 2014; 12; 863-68
8.. Shanmugam S, Bharath R, Dermatofibrosarcoma protuberans of perianal region: A rare case report: Int Surg J, 2022; 9(6); 1284-86
9.. Berebichez-Fridman R, Deutsch Y, Stewart-Treves syndrome: A case report and review of the literature: Case Rep Oncol, 2016; 9; 205-11
10.. Miller S, Alam M, Andersen J, Dermatofibrosarcoma protuberans: Clinical practice guidelines in oncology: J Natl Compr Canc Netw, 2012; 10; 312-18
11.. Ugurel S, Kortmann RD, Mohr P, Short German guidelines: Dermatofibrosarcoma protuberans: J Dtsch Dermatol Ges, 2008; 6; S17-S18
12.. Wiesmueller F, Agaimy A, Perrakis A, Dermatofibrosarcoma protuberans: Surgical management of a challenging mesenchymal tumor: World J Surg Oncol, 2019; 17; 90
13.. Lemm D, Mügge L, Mentzel T, Höffken K, Current treatment options in dermatofibrosarcoma protuberans: J Cancer Res Clin Oncol, 2009; 135; 653-65
14.. Chen YT, Tu WT, Lee WR, Huang YC, The efficacy of adjuvant radiotherapy in dermatofibrosarcoma protuberans: A systemic review and meta-analysis: J Eur Acad Dermatol Venereol, 2016; 30; 1107-14
15.. Harati K, Lange K, Goertz O, A single-institutional review of 68 patients with dermatofibrosarcoma protuberans: Wide re-excision after inadequate previous surgery results in a high rate of local control: World J Surg Onc, 2017; 15; 5
16.. Sun LM, Wang CJ, Huang CC, Dermatofibrosarcoma protuberans: Treatment results of 35 cases: Radiother Oncol, 2000; 57; 175-81
17.. Haas R, Keus R, Loftus B, The role of radiotherapy in the local management of dermatofibrosarcoma protuberans: Eur J Cancer, 1997; 33; 1055-60
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250