24 October 2023: Articles 
Episodic Cocaine Use as a Cause of Venous Thromboembolism and Acute Liver Injury
Unknown etiology
Khyati H. Patel1ABCDEF*, Kyle C. Thomas1ABCDE, Stephen K. Stacey2ABCDEDOI: 10.12659/AJCR.941360
Am J Case Rep 2023; 24:e941360
Abstract
BACKGROUND: Pulmonary embolism secondary to deep vein thrombosis (DVT) with cor pulmonale is commonly associated with risk factors including surgery, cancer, and prolonged immobility. Cocaine is known to cause vasoconstriction and has a prothrombotic effect. Prolonged and heavy use of cocaine can also cause inflammation and liver damage. However, data on its potential role in causing pulmonary embolism and direct hepatotoxicity in cases of episodic use are scarce.
CASE REPORT: A 34-year-old man with no significant medical history except for episodic cocaine use presented in respiratory distress. Workup revealed submassive pulmonary embolism with pulmonary infarctions complicated by pneumonia, hypoxemic respiratory failure, and anemia. He was treated with anticoagulation and intensive care. On day 5 of hospitalization, the patient had an acute hepatic injury. His alanine aminotransferase level peaked at over 2000 IU/L on day 7, until finally tapering. Liver failure was found to be secondary to cocaine use. Liver enzyme levels improved with supportive care. He was discharged with apixaban and continued liver enzyme monitoring.
CONCLUSIONS: When investigating the cause of venous thromboembolism and transaminitis, evaluating cocaine use via patient history or laboratory analysis of cocaine and its metabolites should be considered. Cocaine is known to cause vasoconstriction and has a prothrombotic effect, although data on its potential role in causing pulmonary embolism and direct hepatotoxicity in cases of episodic use are scarce. Further investigation, such as cohort studies, could help strengthen our understanding of the relationship between cocaine use, acute hepatic injury, and pulmonary embolism.
Keywords: Chemical and Drug Induced Liver Injury, Cocaine, venous thromboembolism, Male, Humans, Adult, Pulmonary Embolism, Anticoagulants
Background
Pulmonary embolism secondary to deep vein thrombosis (DVT) is commonly caused by risk factors responsible for any of Virchow’s triad elements – hypercoagulability, venous stasis, and vessel wall injury. Well-known risk factors include surgery, cancer, trauma, pregnancy, prolonged immobilization, and inherited or acquired coagulation disorders. In addition, there are other comorbidities, such as diabetes, hypertriglyceridemia, and hypertension, which increase the risk for DVT/pulmonary embolism. We present the case of a patient who had none of these risk factors or associated comorbidities. His only known medical problem was episodic cocaine use.
Cocaine, a stimulant, can be administered through intranasal (snorting), intravenous, and inhalational routes. Depending on the route of administration, it can cause various pulmonary complications, including pulmonary edema, pulmonary hemorrhage, asthma, hypersensitivity lung disease, and aortic dissection [1–4]. Cocaine also causes liver damage by direct toxic effects on hepatocytes and impairing its antioxidant system by depleting glutathione [5]. Recent studies indicate it can have primary prothrombotic effects [6,7]. Cocaine is known to cause myocardial infarction-arterial thrombosis, but data on its role in causing DVT/pulmonary embolism-venous thrombosis are limited.
Case Report
A 34-year-old man presented to the Emergency Department with 1 month of progressively worsening shortness of breath that had become severe in the past 2 days. The patient reported a history of COVID-like symptoms approximately a month ago, but his SARS-CoV-2 nasal antigen assay was negative. Family and past medical history were noncontributory. He denied illicit drug use.
On examination, he was alert and oriented to time, place, and person and in acute respiratory distress. Physical examination revealed pallor. The cardiac and pulmonary examinations were normal. Vitals signs were temperature: 36.9°C; heart rate: 115 beats/min; respiratory rate: 24/min; blood pressure: 155/101 mmHg; and O2 Saturation: 97% on room air. His laboratory test results were significant for hemoglobin of 5.6 mg/ dL and elevated D-dimer level of 1445 ng/mL. A computed tomography (CT) angiogram of the chest revealed acute pulmonary embolism with significant clot burden bilaterally and right upper and lower lobe infiltrates, concerning for pneumonia (Figures 1, 2). A CT of the abdomen and pelvis with intravenous contrast revealed acute DVT in the left external iliac vein and common femoral vein, with acute thrombus in the right renal vein (Figure 3). He was treated with a heparin drip, ceftriaxone, and azithromycin for community-acquired pneumonia and 2 units of packed red blood cells.
He was transferred from the critical access Emergency Department to our Intensive Care Unit (ICU). In the ICU, an echocardiogram showed a severely enlarged right ventricular chamber size, moderately reduced systolic function, and estimated right ventricular systolic pressure of 68 mmHg (right atrial pressure of 15 mmHg).
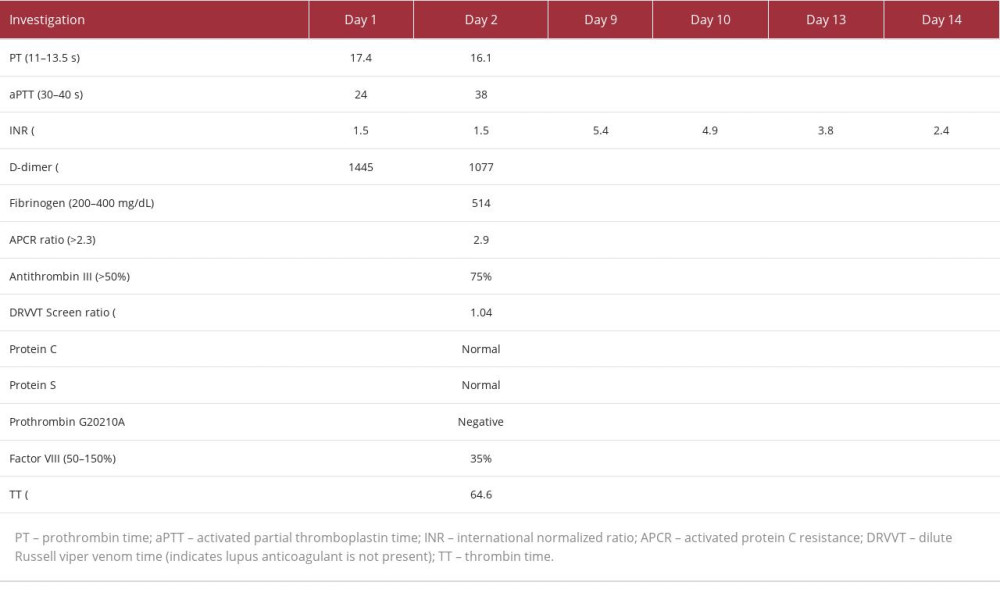
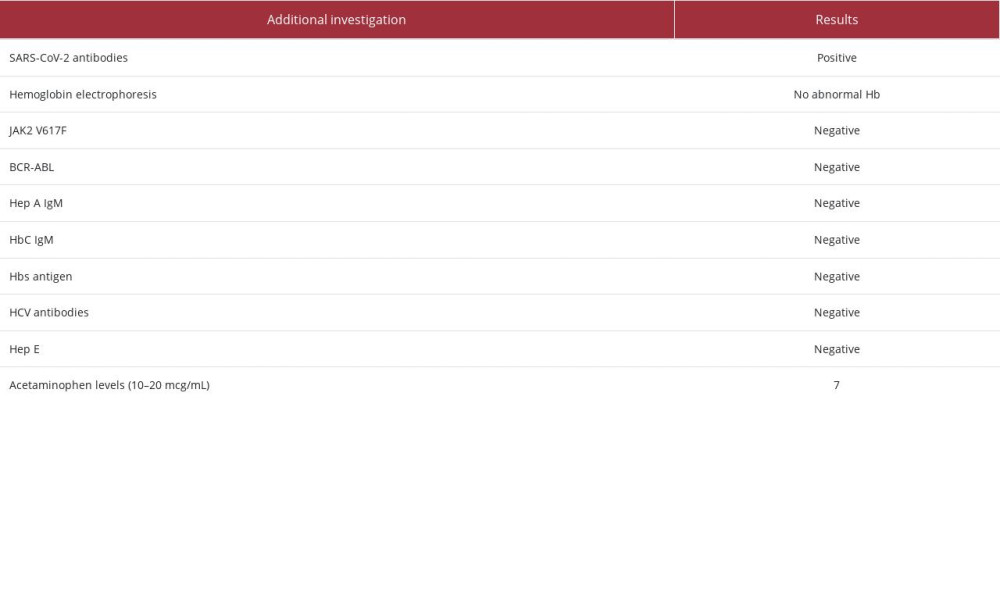
His care was transitioned to the hospitalist team on day 3, who further investigated the cause of his thromboembolism. A coagulation disorder was initially suspected, but his coagulation panel was negative (Table 1). This was further complicated on day 5 by rising liver enzyme levels (Figure 4). Although this trend of liver enzymes is most commonly seen with ischemic hepatitis, his presentation was inconsistent with this diagnosis. He had no hypotensive episodes, jugular venous distension, right upper quadrant tenderness, or elevations in lactate dehydrogenase. Results of magnetic resonance cholangiopancreatography were also normal. Additionally, his liver ultrasound and magnetic resonance imaging were unremarkable for any signs of congestive hepatopathy. Tests for viral hepatitis, autoimmune liver diseases, and acetaminophen toxicity were negative (Table 2).
On day 8, the patient admitted that he had a habit of snorting cocaine once every 1 to 2 weeks when his parents were not present, most recently 5 days before admission. Although a rare cause, the probable diagnosis of venous thromboembolism secondary to cocaine use was made. He was also diagnosed with non-acetaminophen drug-induced liver injury. The patient’s condition was stabilized, and he was discharged on oral apixaban 5 mg for 3 to 6 months and oxygen. His complete blood count and liver function tests were monitored until normal. He was advised against further cocaine use.
Discussion
This patient’s case demonstrates venous thromboembolism in a young adult whose only known risk factor was cocaine use. Although there was an initial concern for a clotting disorder, he had no family history of clotting disorders and his coagulation panel was negative. The case was further complicated by severe hepatic injury. The observed enzyme trend can be seen in multiple conditions, including ischemic liver injury, acetaminophen toxicity, viral hepatitis, autoimmune diseases, and drug-induced liver injury. The patient was initially felt to have an ischemic liver injury, although the typical findings of elevated jugular venous pressure, right upper quadrant tenderness, and elevated lactate dehydrogenase levels were absent. After ruling out other causes and after the patient’s eventual admission of cocaine usage 5 days before his admission, non-acetaminophen drug-induced liver damage, a rare cause for transaminitis, was suspected. He snorted cocaine once every 1 to 2 weeks, obtaining it from different dealers each time.
Cocaine can be prepared using adulterants such as local anesthetics (lidocaine, benzocaine), sugars (mannitol, lactose, sucrose), stimulants (caffeine, ephedrine), toxins (quinine, strychnine), calcium, aspirin, plaster, levamisole, phenacetin, acetaminophen, and hydroxyzine, and inert compounds such as inositol, talc, cornstarch, silica, and flour [8]. In addition, intranasal and inhalation routes can particularly affect the pulmonary artery vasculature by causing intense vasospasm, pulmonary artery hypertension, and possibly even pulmonary infarction [1].
A systematic review of the prothrombotic effects of cocaine details its role in activating the coagulation process by increasing plasminogen activator inhibitor, von Willebrand factor (VWF), hemoglobin, hematocrit, red cell count, and fibrinogen [6]. Even the long-lived metabolites of cocaine, benzoylecgonine and cocaethylene [7], are highly potent VWF secretagogues [7,9]. Less is known about cocaine’s effects on venous endothelial cells, although other cases of cocaine-induced pulmonary embolism exist [6,7]. It has been found that adulterants like levami-sole, which is present in 69% of cocaine samples, are known to cause pulmonary damage, including pulmonary fibrosis [10–12].
Cocaine-induced hepatotoxicity is thought to be mainly due to N oxidative metabolites of cocaine and depletion of intra-cellular and mitochondrial glutathione, which impairs the liver’s antioxidant system [5]. This could underlie the effectiveness of N acetylcysteine in non-acetaminophen drug-induced liver injury [13–15].
Two cases have been reported in the literature in which patients with a history of substance use disorder were diagnosed with acute fulminant liver failure through urine drug screening early in the investigation that revealed cocaine use as the cause [13,14]. Philips et al discussed a patient in a case report akin to ours in which the patient’s self-reported drug use was discovered late, and cocaine was the ultimate cause of drug-induced liver injury [15]. Thus, relying on self-reported data can lead to limitations, such as missing the window period for detecting drugs on screening tests due to delayed patient reporting.
To date, there have been 2 reported cases of cocaine-induced pulmonary embolism. In both cases, patients had pre-existing risk factors, such as a family history of clotting disorders [16], coronary artery disease, type 2 diabetes, hypertension, and hypertriglyceridemia, in addition to using cocaine [16,17]. However, Shah et al published a case report about a young female patient who had no prior medical history but cocaine use and was diagnosed with cocaine-induced diffuse alveolar hemorrhage and in situ lung thrombosis [18].
According to the presented case reports, there exist substantive indications that the use of cocaine can potentially result in pulmonary embolism and acute liver damage. Hence, when investigating the cause of venous thromboembolism and transaminitis, consideration should be given to evaluating cocaine use via urine drug screening or plasma levels. Other potential tests include serum levels of the long-lived metabolites benzoylecgonine and cocaethylene. When obtaining a drug use history, it can help to have an open-minded and nonjudgmental discussion – especially without family members present – as this could give an early insight into ongoing medical issues.
Limitations
The rarity of this pathophysiology was a significant limitation in this case. This was a diagnosis of exclusion, following the disclosure of drug use by the patient. In addition, the reluctance of the patient to discuss drug use habits, particularly in the presence of his parents, resulted in delayed detection of drug use by self-reported data, rendering urine and blood drug screens ineffective. It is important to note that using different drug dealers can potentially expose the patient to different formulations of cocaine mixed with various adulterants. Furthermore, this information was not discovered until later; hence it was not feasible to check for adulterants in the blood or urine and determine the appropriate tests to use. It is therefore essential to approach the subject with sensitivity and create a safe and non-judgmental atmosphere to encourage patients to openly discuss their drug use history and revisit the conversation at every annual health maintenance visit. Finally, idiopathic cases in young healthy adults should trigger consideration of toxicology screening.
Conclusions
Cocaine can be considered a potential risk factor when investigating the cause of DVT/pulmonary embolism. Previous case reports have discussed the effect of cocaine-induced arterial thrombosis, but there is scarce data on cocaine-induced venous thrombosis. Also, whether cocaine adulterants play a role in inducing thrombosis has not been elucidated. Hence, these can be prospective research areas. Further investigation, such as cohort studies, could help strengthen our understanding of the relationship between cocaine use, acute hepatic injury, and pulmonary embolism.
Figures
References:
1.. de Almeida RR, de Souza LS, Mançano AD, High-resolution computed tomographic findings of cocaine-induced pulmonary disease: A state of the art review: Lung, 2014; 192(2); 225-33
2.. Meisels IS, Loke J, The pulmonary effects of free-base cocaine: A review: Cleve Clin J Med, 1993; 60(4); 325-29
3.. Mohamed MA, Abraham R, Maraqa TI, Elian S, Cocaine-induced type-A aortic dissection extending to the common iliac arteries: Cureus, 2018; 10(1); e2059
4.. Terra Filho M, Yen CC, Santos Ude P, Muñoz DR, Pulmonary alterations in cocaine users: Sao Paulo Med J, 2004; 122(1); 26-31
5.. Graziani M, Antonilli L, Togna AR, Cardiovascular and hepatic toxicity of cocaine: Potential beneficial effects of modulators of oxidative stress: Oxid Med Cell Longev, 2016; 2016; 8408479
6.. Wright NM, Martin M, Goff T, Cocaine and thrombosis: A narrative systematic review of clinical and in-vivo studies: Subst Abuse Treat Prev Policy, 2007; 2; 27
7.. Hobbs WE, Moore EE, Penkala RA, Cocaine and specific cocaine metabolites induce von Willebrand factor release from endothelial cells in a tissue-specific manner: Arterioscler Thromb Vasc Biol, 2013; 33(6); 1230-37
8.. Karila L, Petit A, Lowenstein W, Reynaud M, Diagnosis and consequences of cocaine addiction: Curr Med Chem, 2012; 19(33); 5612-18
9.. Roque Bravo R, Faria AC, Brito-da-Costa AM, Cocaine: An updated overview on chemistry, detection, biokinetics, and pharmacotoxicological aspects including abuse pattern: Toxins (Basel), 2022; 14(4); 278
10.. Salabei JK, Khan S, Khan A, ANCA-associated intrahepatic duct injury associated with levamisole-adulterated cocaine: Case Reports Hepatol, 2020; 2020; 8867183
11.. Fan T, Macaraeg J, Haddad TM, A case report on suspected levami-sole-induced pseudovasculitis: WMJ, 2017; 116(1); 37-9
12.. , Agranulocytosis associated with cocaine use – four States, March 2008-November 2009: MMWR Morb Mortal Wkly Rep, 2009; 58(49); 1381-85
13.. Dolkar T, Hamad AM, Han MM, Cocaine and opioid-induced acute liver injury: A rare case report: Cureus, 2022; 14(3); e23630
14.. Ansari M, Arshed S, Islam M, Sen S, Yousif A, A case of reversible drug-induced liver failure: Clin Case Rep, 2017; 5(7); 1181-83
15.. Philips CA, Chooracken MJ, Mahadevan P, Augustine P, S(n)orting out the problem: Fever of unknown origin and unexplained abnormal transaminases in a young male: Cureus, 2017; 9(8); e1543
16.. Sharma T, Kumar M, Rizkallah A, Cocaine-induced thrombosis: Review of predisposing factors, potential mechanisms, and clinical consequences with a striking case report: Cureus, 2019; 11(5); e4700
17.. Griffin D, Cha S, Cocaine: a provoking risk factor in venous thromboembolism: Cureus, 2019; 11(12); e6520
18.. Shah R, Patel A, Mousa O, Manocha D, Crack lung: Cocaine-induced lung injury: QJM, 2015; 108(9); 749
Figures
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250