30 November 2023: Articles 
Polybacterial Iliopsoas Muscle Abscess as an Indication for Early Diagnosis of Crohn’s Disease
Unusual clinical course, Challenging differential diagnosis, Educational Purpose (only if useful for a systematic review or synthesis)
Shun Yamashita12ABDEF*, Masahiko Nakamura1ABDF, Takashi Akutagawa3DEF, Orisa Nakashima1ACDF, Masaki TagoDOI: 10.12659/AJCR.941399
Am J Case Rep 2023; 24:e941399
Abstract
BACKGROUND: Crohn disease (CD) is a chronic, relapsing inflammatory bowel disease characterized by penetrations or fistulae in the gastrointestinal tract and abscesses in the surrounding tissues. Diagnosis of CD is difficult with an iliopsoas muscle abscess (IMA) as an initial presentation.
CASE REPORT: A 22-year-old Japanese man had right hip pain 17 days prior to admission. Because of worsening pain, he was admitted to our hospital. Physical examination revealed limitation of his right hip motion and a positive right psoas sign. Abdominal contrast-enhanced computed tomography (CT) revealed a large right IMA. Continuous drainage, which revealed polymicrobial pus, with intravenous administration of antibiotics dramatically decreased the size of the IMA. The drainage tube was removed on hospitalization day 9 because barium enema and contrast radiography of the abscess through the drainage tube showed no fistula. However, on day 19 of hospitalization, the IMA was redetected by abdominal CT. Continuous abscess drainage was resumed, and the third contrast radiograph of the abscess revealed contrast medium flow into the small intestine. Colonoscopy detected stenoses and circumferential ulceration of the terminal ileum. Histopathological examination of the ileum biopsy showed histocyte aggregation with lymphocyte or plasmacyte infiltration of the lamina propria, compatible with a CD diagnosis. Laparoscopic ileocecal resection was performed on day 64 of hospitalization.
CONCLUSIONS: Penetration of the intestinal tract caused by CD should be suspected in a patient with a polymicrobial IMA. It is essential to identify the fistula and subsequently perform surgical resection of the affected intestinal area.
Keywords: Crohn Disease, Digestive System Surgical Procedures, Fistula
Background
Crohn disease (CD) is a chronic, relapsing inflammatory bowel disease [1,2]. It is caused by interactions between genetic and environmental factors [1,3]. Among the genetic factors, it has been shown that NOD2 homozygosity can increase the risk of developing CD by 20- to 40-fold [4]. Environmental factors include smoking, oral contraceptive use, lifestyle and hygiene, vaccinations, surgeries, exposure to drugs, including nonsteroidal anti-inflammatory drugs or antibiotics, and exposure to gastrointestinal pathogens [1,3]. In many countries, the risk of developing CD is higher in women than in men by 20% to 30% [3], and 80% of patients with CD are diagnosed before 40 years of age [6,7]. In Japan, CD often develops in the late teens to early 30s, with a 2.4-fold higher incidence in men than in women and with annual incidence of 55.6 per 100 000 persons [8,9]. CD causes various manifestations, including systemic signs, such as fever, malaise, or weight loss; gastrointestinal signs, such as diarrhea or abdominal pain; and extra-gastrointestinal signs, such as anemia, aphthous stomatitis, erythema nodosum, uveitis, scleritis, or venous thromboembolism [1,2,10]. The Montreal classification system categorizes the phenotypes of CD by the age of onset, the affected location within the intestinal tract, and disease behavior [11]. The gastrointestinal symptoms and signs of CD depend on the affected location in the gastrointestinal tract [1]. Patients with ileal-type and ileocolonic-type CD can present with fistulae in the gastrointestinal tract and abscesses in surrounding tissues, and those with colonic-type CD can present with fistulae in the rectum or perirectal abscesses [1]. Patients with CD can already have advanced conditions, such as intestinal perforations or fistulae or nearby intra-abdominal abscesses, at the initial medical visit because of the insidious progression of the disease [1,12]. In fact, 46% of patients with CD reportedly developed at least one fistula, most of which were perianal fistulae, before or at the time of diagnosis [13]. Surgical re-section of the affected area in the gastrointestinal tract along with antibiotic treatment is required to treat patients with CD complicated with abscesses caused by intestinal penetration or fistulae [2], but preoperative diagnosis of CD associated with iliopsoas muscle abscess (IMA) as an initial presentation can be difficult [14].
We report the case of a patient with CD who developed a right IMA from a fistula in the small intestine before showing typical systemic, gastrointestinal, or extra-gastrointestinal manifestations of CD. Repeated contrast radiography of the abscess through the drainage tube and barium enema made it possible to detect the fistula, which was missed by the initial and second rounds of contrast radiography, initial round of abdominal contrast-enhanced computed tomography (CT), and barium enema. Detection of the fistula led to the diagnosis of CD, resulting in subsequent surgical resection of the affected site in the intestinal tract to prevent the recurrence of the abscess.
Case Report
Two months before hospital admission, a previously healthy 22-year-old man had presented with abdominal pain and vomiting for 2 days. His symptoms spontaneously improved, and he was able to eat as usual. However, 17 days before admission, he experienced pain and limitation of the motion in his right hip, which gradually worsened. He visited his primary physician 9 days before admission, and non-steroidal anti-inflammatory drugs were prescribed. However, since his general condition and hip pain worsened, he was eventually admitted to our hospital.
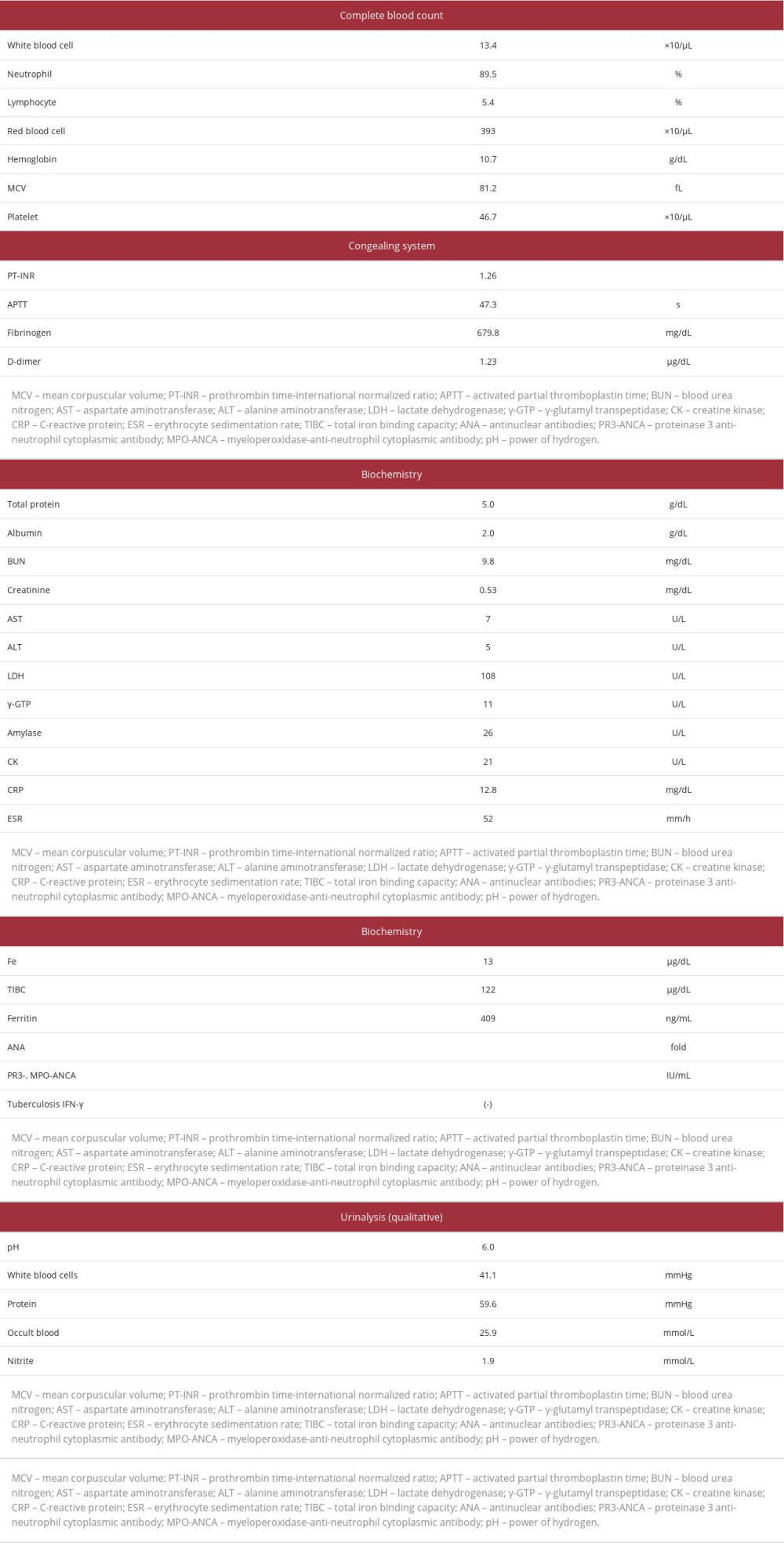
On admission, he was alert, with a body temperature of 38.0°C, pulse rate of 84 beats/min, blood pressure of 86/50 mmHg, respiratory rate of 22 breaths/min, and oxygen saturation of 97% on room air. Physical examination revealed only limitation of the motion of his right hip and a positive psoas sign, without petechial hemorrhage of the palpebral conjunctiva, caries, cardiac murmur, Osler nodes, Janeway lesions, abdominal tenderness, tenderness of the costovertebral angle upon percussion, or edema of the lower limbs. His laboratory findings on admission are presented in Table 1. He had a white blood cell count of 13 400 cells/µL (neutrophil percentage, 89.5%), serum hemoglobin concentration of 10.7 g/dL (mean corpuscular volume, 81.2 fL), serum total protein concentration of 5.0 g/dL, serum albumin concentration of 2.0 g/dL, serum C-reactive protein concentration of 12.8 mg/dL, and erythrocyte sedimentation rate of 52 mm/h. In addition, his serum iron concentration was 12 µg/dL, with a serum total iron binding capacity of 122 µg/dL and serum ferritin level of 409 ng/mL, compatible with the presence of chronic inflammation. There were no signs of liver or kidney dysfunction, with normal serum lactate dehydrogenase and creatine kinase concentrations. Serological tests for syphilis, HIV antibodies, antinuclear antibodies, and antineutrophil cytoplasmic antibodies were all negative, as was the interferon gamma release assay for tuberculosis. Echocardiography showed no valvular diseases or vegetations. Abdominal CT with contrast enhancement showed a large, low-density, ring-enhancing area in the right iliopsoas muscle containing air density areas, suggesting a right gas-forming IMA, without low-density areas indicative of infarction in the liver, kidneys, or spleen (Figure 1A, 1B). In addition, enlargement of the appendix and thickening of the sigmoid colon wall were revealed without mural enhancement of other parts of the intestinal tract or other findings characteristic of CD, including a fat halo sign or comb sign. The IMA sample obtained by CT-guided drainage was a stool-like pus with the odor of feces, and subsequent culture revealed the presence of
With continuous drainage of the IMA and intravascular administration of cefotiam, metronidazole, and caspofungin acetate, the patient’s fever and right hip pain gradually improved, concurrent with decreases in his white blood cell count and serum C-reactive protein concentration. In addition, abdominal CT with contrast enhancement on hospitalization day 9 revealed a marked decrease in the size of the right IMA. An intestinal penetration was highly suspected because of the polymicrobial pus culture, which included enterobacteria; therefore, barium enema and contrast radiography of the abscess through the drainage tube using a diluted barium sulfate was performed without applying excessive pressure during the procedure.
However, no communication was observed between the intestinal tract and the IMA. Subsequently, the drainage tube for the right IMA was removed on day 9. On the same day, intravenous antibiotics and an antifungal agent were changed to oral administration, with the resumption of oral food intake. However, on day 19 of admission, his right hip pain recurred, and abdominal CT with contrast enhancement showed relapse of the IMA (Figure 1C, 1D). Abdominal ultrasonography revealed no apparent intestinal fistula, and the second round of contrast radiography of the abscess through the drainage tube failed to show leakage of the contrast medium into the intestinal tract. Colonoscopy was performed, which revealed a stenosis and a circumferential ulcer in the terminal ileum (Figure 2). Histopathological examination of the ileum biopsy samples revealed histocyte aggregation, with infiltration of lymphocytes and plasmacytes in the lamina propria (Figure 3). The third round of contrast radiography of the abscess through the drainage tube, which was performed on day 30, finally demonstrated the flow of contrast medium into the small intestine (Figure 4). The second barium enema on the day 35 revealed multiple stenoses, with leakage of the contrast medium outside the bowel in the ileocecal region (Figure 5). The intestinal stenoses and histological findings were suggestive of CD in this patient, leading to the diagnosis of secondary IMA caused by CD.
Subsequently, laparoscopic ileocecal resection was performed on day 64 of admission. Hematoxylin and eosin staining of the resected ileocecum showed transmural infiltration of inflammatory cells, with significant fibrosis. In addition, the formation of an abscess containing multinucleated giant cells was identified in the mucosal layer. Based on these findings, we confirmed that the present case was consistent with CD (Figure 6). Drainage of the IMA and intravenous administration of antibiotics and antifungal agents were performed for an appropriate period. Consequently, the patient was discharged on day 78, without recurrence of the IMA. Oral administration of mesalamine was started on an outpatient basis.
Discussion
CD is a chronic, relapsing inflammatory bowel disease that often affects patients in their late teens to early 40s with a variety of systemic, gastrointestinal, and extra-gastrointestinal symptoms [1,2,7–11]. Intestinal penetrations, fistulae, or abscesses can be the first manifestations of CD because of its often insidious progression [1,12]. Among abscesses caused by CD, IMAs are relatively rare (occurring in 0.4% to 4.3% of patients) with nonspecific manifestations [14], making it difficult to diagnose CD as the underlying cause of IMAs [15,16]. However, identification of the causative bacteria of an IMA can help identify the mechanism of development as either primary or secondary. Primary IMAs are caused by hematogenous dissemination of bacteria, mainly gram-positive cocci, whereas secondary IMAs are caused by invasion of the causative bacteria from adjacent organs [17]. The most common cause of secondary IMA is intestinal penetration caused by CD, and the causative agents are usually polymicrobial, including enterobacteria (such as gram-negative rods), anaerobes, or fungi [17]. The patient in the present case developed an IMA with scarce systemic or gastrointestinal manifestations of CD upon IMA diagnosis. Our experience suggests that, when seeing a young patient with polymicrobial IMA at the peak age of CD onset, it is essential to suspect intestinal penetrations due to CD, even without typical symptoms, signs, or past history of CD.
Several cases of CD with atypical presentations have been reported: a case with poor systemic and gastrointestinal signs for CD other than fever [18], cases with lesions located in only the large intestine [19,20], and cases with atypical or rare extra-gastrointestinal signs of CD [21–25]. When lesions are located in only the large intestine, it can be difficult to distinguish CD from ulcerative colitis [19]. The clinical manifestations of a CD case localized to the appendix are similar to those of acute appendicitis, and a diagnosis of CD is possible only by histopathological examinations [20]. The reported atypical or rare extra-gastrointestinal signs of CD are as follows: complication of superior mesenteric vein obstruction and protein-losing enteropathy [21]; thrombosis in the portal vein and splenic vein, with diffuse abdominal lymphadenopathy requiring differentiation from malignant lymphoma [22]; acute intermittent porphyria [23]; and presacral abscess [24,25]. The present case was an atypical case of CD because of the lack of systemic and gastrointestinal signs other than fever. In addition, the patient had an IMA that made it difficult to identify the site of penetration of the intestinal tract, which made the diagnosis of CD extremely elusive.
The most useful and reliable tool to make a diagnosis of CD is colonoscopy with biopsy [2]. However, performing colonos-copy risks disseminating intestinal bacteria into the abdominal cavity if there is an intestinal penetration or perforation.
Furthermore, small intestinal CD cannot be diagnosed by colonoscopy. Although capsule endoscopy is useful for the diagnosis of small intestinal CD, capsule retention in the gastrointestinal tract could occur in cases featuring a gastrointestinal stenotic lesion [9]. Therefore, it is necessary to evaluate the condition of the gastrointestinal system, especially for the presence of penetrations, perforations, fistulae, or stenoses, before performing gastrointestinal endoscopy [2,26]. Although barium enema examination and contrast radiography of the abscess through the drainage tube are traditional evaluation methods for the conditions mentioned above, they have relatively low sensitivity and specificity [17]. Currently, magnetic resonance enterography is available in some settings as a useful alternative modality to evaluate mucosal lesions of the gastrointestinal tract with a sensitivity ≥80% and specificity ≥90%, and to detect abscesses or fistulae with a sensitivity ≥90% and specificity ≥95% [27]. It was difficult for us to identify communication between the IMA and intestinal tract, although penetration of the intestinal tract due to CD was initially suspected on the basis of the polymicrobial culture results of the pus from the IMA, which included enterobacteria. We regrettably failed to perform magnetic resonance enterography because of the negative findings of the first round of contrast radiography of the abscess through the drainage tube and barium enema, which led to removal of the IMA drainage tube. As a result, the patient’s IMA recurred after a short period. In a patient with a polymicrobial IMA, it is essential to investigate the presence of penetrations or fistulae in the gastrointestinal tract by repeated contrast radiography of the abscess through the drainage tube or barium enema, or to utilize high-performance modalities such as magnetic resonance enterography [27].
Patients with CD can usually achieve remission and maintenance of the disease using corticosteroids, immunosuppressive agents, or biological agents. Other treatment modalities, such as surgical treatments or administration of antibiotics, are required for patients who are intractable to standard medical treatments or those with intestinal fistulae or abscesses [1,2]. Percutaneous abscess drainage is among the useful surgical treatments for patients with a penetrating type of CD who develop fistulae or abscesses [14]. In addition, it is necessary to completely resect an intestinal fistula after percutaneous drainage to avoid recurrence of the abscess [28,29]. Our patient did not have an IMA recurrence after complete surgical resection of the intestinal fistula following percutaneous drainage.
Conclusions
When seeing a young patient with a polymicrobial IMA that features enterobacteria, physicians should suspect the presence of penetrations or fistulae of the small intestine or colon caused by CD, even without typical manifestations of CD such as abdominal pain or diarrhea. Since it can be difficult to identify the location of penetrations, it is essential to repeat radiographic examinations to facilitate surgical resection of the affected area of the intestinal tract.
Figures
References:
1.. Veauthier B, Hornecker JR, Crohn’s disease: Diagnosis and management: Am Fam Physician, 2018; 98(11); 661-69
2.. Baumgart DC, Sandborn WJ, Crohn’s disease: Lancet, 2012; 380(9853); 1590-605 [Erratum in: Lancet. 2013;381(9862):204]
3.. Singh N, Bernstein CN, Environmental risk factors for inflammatory bowel disease: United European Gastroenterol J, 2022; 10(10); 1047-53
4.. Ananthakrishnan AN, Epidemiology and risk factors for IBD: Nat Rev Gastroenterol Hepatol, 2015; 12(4); 205-17
5.. Langholz E, Current trends in inflammatory bowel disease: The natural history: Therap Adv Gastroenterol, 2010; 3(2); 77-86
6.. Freeman HJ, Natural history and long-term clinical course of Crohn’s disease: World J Gastroenterol, 2014; 20(1); 31-36
7.. Freeman HJ, Application of the Vienna Classification for Crohn’s disease to a single clinician database of 877 patients: Can J Gastroenterol, 2001; 15(2); 89-93
8.. Murakami Y, Nishiwaki Y, Oba MS, Estimated prevalence of ulcerative colitis and Crohn’s disease in Japan in 2014: An analysis of a nationwide survey: J Gastroenterol, 2019; 54(12); 1070-77 [Erratum in: J Gastroenterol. 2019;55(1):131]
9.. Nakase H, Uchino M, Shinzaki S, Evidence-based clinical practice guidelines for inflammatory bowel disease 2020: J Gastroenterol, 2021; 56(6); 489-526
10.. Lichtenstein GR, Loftus EV, Isaacs KL, ACG Clinical Guideline: Management of Crohn’s disease in adults: Am J Gastroenterol, 2018; 113(4); 481-517 [Erratum in: Am J Gastroenterol. 2018;113(7):1101]
11.. Satsangi J, Silverberg MS, Vermeire S, Colombel JF, The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications: Gut, 2006; 55(6); 749-53
12.. Freeman HJ, Long-term clinical behavior of jejunoileal involvement in Crohn’s disease: Can J Gastroenterol, 2005; 19(9); 575-78
13.. Schwartz DA, Loftus EV, Tremaine WJ, The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota: Gastroenterology, 2002; 122(4); 875-80
14.. Ogihara M, Masaki T, Watanabe T, Psoas abscess complicating Crohn’s disease: Report of a case: Surg Today, 2000; 30(8); 759-63
15.. Gao D, Medina MG, Alameer E, Nitz J, Tsoraides S, A case report on delayed diagnosis of perforated Crohn’s disease with recurrent intra-psoas abscess requiring omental patch: Int J Surg Case Rep, 2019; 65; 325-28
16.. Amato L, Valeri M, Emini P, Retroperitoneal and iliopsoas abscess as Crohn’s disease onset mimicking a common lumbosciatic pain: Ann Ital Chir, 2022; 11; S2239253 X22037458
17.. Mallick IH, Thoufeeq MH, Rajendran TP, Iliopsoas abscesses: Postgrad Med J, 2004; 80(946); 459-62
18.. Kęsicka A, Burandt J, Główczewski A, Krogulska A, Fever as the only first sign of Crohn’s disease-difficulties in diagnosis during the COVID-19 pandemic: Children (Basel), 2022; 9(12); 1791
19.. Ali MZ, Tariq MU, Abid MH, A case report and literature review of rectosigmoid Crohn’s disease: A diagnostic pitfall ultimately leading to spontaneous colonic perforation: Cureus, 2023; 15(3); e36941
20.. Gnanaselvam P, Weerakoon DN, Wijayasuriya WAM, Isolated Crohn’s disease of the appendix presenting as acute appendicitis in a 60-year-old South Asian female: A case report, review of literature, and follow-up recommendations: Case Rep Surg, 2019; 201; 5285417
21.. Ito S, Higashiyama M, Horiuchi K, Atypical clinical presentation of Crohn’s disease with superior mesenteric vein obstruction and protein-losing enteropathy: Intern Med, 2019; 58(3); 369-74
22.. Raza A, Chan V, Cheema MA, Atypical clinical presentation of Crohn’s disease as diffuse abdominal lymphadenopathy and venous thrombosis: A difficult to diagnose case: Cureus, 2019; 11(9); e5805
23.. Mitre C, Mercea V, Copaciu IM, Acute intermittent porphyria – an unexpected association in a patient with newly diagnosed Crohn’s disease: J Gastrointestin Liver Dis, 2019; 28(4); 509-12
24.. Wang J, Ng M, Kochar K, Large presacral abscess in a patient with Crohn’s disease: J Surg Case Rep, 2019; 2019(11); rjz297
25.. Jwa HJ, Song HJ, Jun H, Gluteal and presacral abscess due to Crohn’s disease with multiple fistulas: Korean J Gastroenterol, 2022; 80(6); 267-72
26.. Panés J, Rimola J, Perianal fistulizing Crohn’s disease: Pathogenesis, diagnosis and therapy: Nat Rev Gastroenterol Hepatol, 2017; 14(11); 652-64
27.. Church PC, Turner D, Feldman BM, Systematic review with meta-analysis: Magnetic resonance enterography signs for the detection of inflammation and intestinal damage in Crohn’s disease: Aliment Pharmacol Ther, 2015; 41(2); 153-66
28.. Funayama Y, Sasaki I, Naito H, Psoas abscess complicating Crohn’s disease: Report of two cases: Surg Today, 1996; 26(5); 345-48
29.. Ribeiro MB, Greenstein AJ, Yamazaki Y, Aufses AH, Intra-abdominal abscess in regional enteritis: Ann Surg, 1991; 213(1); 32-36
Figures
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250