01 November 2023: Articles 
Fulminant Lymphocytic Myocarditis Successfully Managed with Intra-Aortic Balloon Pump and Extracorporeal Membrane Oxygenation:A Case Report
Unusual or unexpected effect of treatment, Rare disease
Suélisson da Silva Araujo1ABEF, Izadora Raduan Brigo1ABEF, Leopoldo Fernando Moura Campos Angerami1ABEF, Pedro Henrique Ferro de Brito1ABEF, Rogério Bicudo Ramos Filho1ABEF, Taiane Maria Silva Terra1ABEF, Thais Baptista Teixeira1ABEF, Arthur Cicupira Rodrigues de Assis1ABF, Paulo Rogério Soares1ABEF, Thiago Luis ScudelerDOI: 10.12659/AJCR.941422
Am J Case Rep 2023; 24:e941422
Abstract
BACKGROUND: Lymphocytic myocarditis (LM) is a rare inflammatory disease of the heart. The clinical presentation of LM varies from mild flu-like symptoms to fulminant myocarditis with cardiogenic shock. Fulminant myocarditis has a poor prognosis and the usual treatment is inotropes with or without ventricular assist devices such as intra-aortic balloon pump (IABP) and venoarterial extracorporeal membrane oxygenation (V-A ECMO). We report the case of fulminant LM with severe cardiogenic shock that was successfully treated with concomitant use of IABP and V-A ECMO.
CASE REPORT: A 32-year-old woman with no medical history presented to the Emergency Department (ED) with chest pain with irradiation to the left upper limb, worse when supine. The electrocardiogram (ECG) on admission showed sinus rhythm with nonspecific ST-T repolarization abnormalities, and laboratory results showed elevated ultrasensitive troponin and C-reactive protein. Transthoracic echocardiography (TTE) showed left ventricular ejection fraction (LVEF) of 25% and diffuse hypokinesis. On the next day, she developed cardiogenic shock requiring vasoactive drugs, IABP, and V-A ECMO. Pulse therapy with methylprednisolone was started. Endomyocardial biopsy (EMB) revealed acute LM, and intravenous human immunoglobulin was administered. The patient evolved with progressive clinical improvement, being discharged 56 days after admission, with an improvement in the LVEF to 55%.
CONCLUSIONS: Fulminant LM is a rare and potentially fatal condition that requires immediate intervention. The combination of IABP and V-A ECMO among patients with LM-cardiogenic shock may provide survival benefits.
Keywords: Extracorporeal Membrane Oxygenation, Intra-Aortic Balloon Pumping, myocarditis
Background
Fulminant LM is a serious and potentially fatal condition involving acute inflammation of the heart muscle. This condition is characterized by rapid deterioration of heart function and can lead to heart failure and sudden death. Although fulminant LM is relatively rare, it can occur in any age group and is often challenging to diagnose. However, the incidence and prevalence of fulminant LM is not well characterized. Viral infection is likely the most common cause of lymphocytic myocarditis and is found in 30% to 40% of cases [1]. Importantly, no specific therapies for fulminant LM exist. Most of these patients require inotropic support and, in some cases, IABP. In refractory cases, V-A ECMO may be considered. Unfortunately, it is difficult to predict which patients will achieve sustained myocardial recovery after removal of the ventricular assist device [2]. The role of immunosuppressive therapy in the treatment of fulminant myocarditis remains unclear. Previous trials have failed to demonstrate a beneficial effect of immunosuppression [3–5]. We report the case of a young patient with fulminant LM and cardiogenic shock successfully treated with mechanical circulatory support (IABP plus V-A ECMO).
Case Report
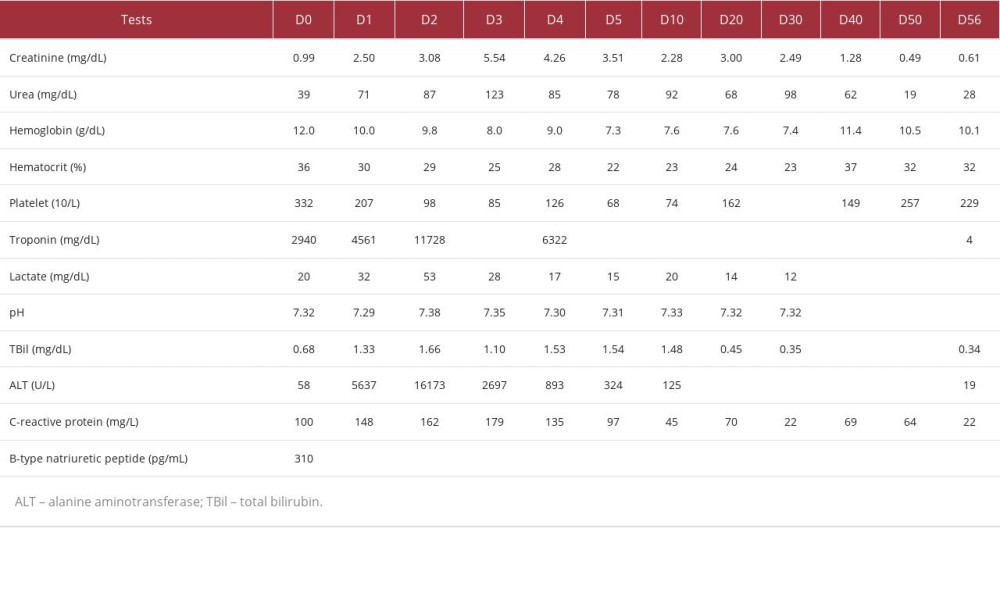
A 32-year-old woman with no significant past medical history was admitted to the ED with chest pain with irradiation to the left upper limb, worse in the supine position. She presented with a heart rate of 89 beats per minute, blood pressure of 110/60 mmHg, and body temperature of 36.3°C. Her respiratory rate was 14 breaths per minute with 96% peripheral oxygen saturation without supplementary oxygen. At that time, her physical exam results were unremarkable. She reported flu-like symptoms 7 days before admission to the ED, with an episode of fever measured at 39.0°C. The ECG on admission showed sinus rhythm with nonspecific ST-T repolarization abnormalities (Figure 1). Laboratory results were notable for ultrasensitive troponin of 2940 mg/dL, C-reactive protein of 100 mg/L, and B-type natriuretic peptide of 310 pg/mL (Table 1). A viral panel for influenza A and B, respiratory syncytial virus, and SARSCoV-2 was negative. The presumptive diagnosis of myocarditis was made based on the results of biological and cardiac tests, and colchicine and aspirin were started. On the next day, she developed respiratory failure, and hemodynamic instability, requiring intubation. Noradrenaline 0.20 mcg/Kg/min and dobutamine 12.0 mcg/kg/min were started. A chest X-ray showed bilateral pulmonary congestion. Left heart catheterization revealed non-obstructive coronary artery disease. Transthoracic echocardiography (TTE) showed LVEF of 25%, diffuse hypokinesis, inter-ventricular septal dyssynchrony, and moderate right ventricular dysfunction (Figure 2). She was given high-dose pulse steroids early. One gram per day of IV methylprednisolone was given in the first 3 days, followed by tapering doses of prednisone, 60 mg once a day for 2 days, 40 mg once a day for 2 days, 20 mg once a day for 2 days, and then 10 mg once a day for 2 days.
As the patient maintained signs of low cardiac output despite high doses of vasoactive drugs, an IABP was inserted. Then, the patient presented ventricular tachycardia with pulse, without reversal with synchronized electrical cardioversion. At that time, amiodarone and lidocaine were started to control the ventricular arrhythmia. She remained dependent on vasopressor, inotropic support, and IABP, with a rising lactate and V-A ECMO was started. Urgent EMB was performed to confirm the clinical diagnosis of fulminant myocarditis and to determine the underlying etiology. Endomyocardial histology demonstrated features consistent with myocarditis with predominantly lymphocytic infiltrates (Figure 3). Intravenous human immunoglobulin 30 g per day for 5 days was then indicated. On the third day of admission, continuous renal replacement therapy was initiated for acute kidney injury. On the 10th day of admission, noradrenaline was withdrawn. On the 11th day of admission, a new TTE was performed, showing a LVEF of 45% and moderate right ventricular dysfunction. V-A ECMO was successfully explanted after 11 days of support. Dobutamine was weaned off by day 14 of admission. TTE performed on day 15 revealed an LVEF of 55% and mild RV dysfunction. IABP was withdrawn.
After recovery of hemodynamics, the patient was started on heart failure treatment, including carvedilol and angiotensin-converting enzyme inhibitor. TTE done before discharge showed normal left ventricle cavity size and LVEF of 55%. She was discharged in stable condition 56 days after admission.
Discussion
LM is the most common form of myocarditis and is associated with viral/post-viral infection, autoimmune/connective tissue disease, or may be idiopathic [6]. Fulminant myocarditis is a syndrome characterized by the need for inotropic or mechanical circulatory support to maintain end-organ perfusion until transplantation or recovery [1]. The initial clinical presentation of fulminant myocarditis is nonspecific, ranging from flu-like symptoms to cardiogenic shock and potentially fatal arrhythmias [7] and it is associated with a mortality rate greater than 50% [8].
The role of immunosuppressive therapy is well-established for treating giant cell myocarditis, eosinophilic myocarditis, cardiac sarcoidosis, and acute myocarditis associated with systemic autoimmune diseases [9]. Although the role of immunosuppressive therapies for patients with acute LM remains controversial [10], intravenous corticosteroid was indicated, initially and intravenous immunoglobulin, later, after confirmation of LM, due to the severity of the disease presentation.
The role of EMB to guide management has not been evaluated in large clinical trials. In our patient, EMB was performed due to clinically suspected myocarditis and the presence of cardiogenic shock. Other indications for EMB in the context of acute myocarditis are: ventricular arrhythmias or Mobitz type II second-degree or higher atrioventricular (AV) block, particularly when symptom onset is recent, with mild or no left ventricular dilatation; peripheral eosinophilia or an associated systemic inflammatory disorder; persistent or recurrent release of necrosis markers, particularly when an autoimmune condition is likely or ventricular arrhythmias and high-degree AV block are present; or cardiac dysfunction in a patient receiving immune checkpoint inhibitor therapy [11].
The patient’s EMB showed LM, with negative viral genome research results. A multicenter study showed that only 38% of patients with myocarditis were able to find the viral genome in their EMB samples [12].
Cardiovascular magnetic resonance (CMR) is a non-invasive test capable of providing diagnostic and prognostic information in patients with clinically suspected myocarditis. There are 3 sequences that are classically used for the diagnosis of myocarditis: early global enhancement, myocardial edema (T2), and late gadolinium enhancement (LGE). These techniques allow visualization of tissue features typically found in inflammation, such as edema, hyperemia, capillary leak, necrosis, and fibrosis. However, due to the patient’s severe hemodynamic instability, CMR was not performed [13].
For patients with fulminant myocarditis with poor drug treatment effect, it is recommended to use temporary mechanical circulatory support (MCS) [14]. Due to our patient’s poor response to vasoactive drugs, we immediately inserted IABP, which can provide sufficient hemodynamic support and prompt end-organ function recovery in patients with cardiogenic shock [15]. Ogunbayo et al showed that the use of IABP in patients with acute myocarditis complicated by cardiogenic shock can reduce mortality [16].
As IABP did not sufficiently improve the patient’s hemodynamic condition, V-A ECMO was considered. Pozzi et al showed that use of V-A ECMO is associated with an overall survival to hospital discharge rate of 55–78% in patients with fulminant and acute myocarditis developing cardiogenic shock [17]. However, several studies comparing V-A ECMO plus IABP versus V-A ECMO alone in patients with cardiogenic shock have shown conflicting results [18,19], with the most robust evidence for patients with cardiogenic shock and acute myocardial infarction [20,21].
This present case suggests that the combined use of IABP and V-A ECMO in patients with fulminant LM can reduce the incidence of potentially lethal arrhythmias, improve hemodynamic status, and reduce mortality in patients with a similar profile.
Conclusions
In patients with acute LM complicated by cardiogenic shock, the combination of IABP and V-A ECMO may provide survival benefits.
Figures
References:
1.. Kociol RD, Cooper LT, Fang JC, Recognition and Initial Management of Fulminant Myocarditis: A Scientific Statement From the American Heart Association: Circulation, 2020; 141(6); e69-e92
2.. Houel R, Vermes E, Tixier DB, Myocardial recovery after mechanical support for acute myocarditis: Is sustained recovery predictable?: Ann Thorac Surg, 1999; 68; 2177-80
3.. Wojnicz R, Nowalany-Kozielska E, Wojclechowska C, Randomized, placebo-controlled study for immunosuppressive treatment of inflammatory dilated cardiomyopathy: two-year followup results: Circulation, 2001; 104; 39-45
4.. Gullestad L, Aass H, Fjeld JG, Immunomodulating therapy with intravenous immunoglobulin in patients with chronic heart failure: Circulation, 2001; 103; 220-25
5.. McNamara DM, Holubkov R, Starling RC, Controlled trial of intravenous immune globulin in recent-onset dilated cardiomyopathy: Circulation, 2001; 103; 2254-59
6.. Ganji M, Ruiz-Morales J, Ibrahim S, Acute lymphocytic myocarditis: J Geriatr Cardiol, 2018; 15(7); 517-18
7.. Feldman AM, McNamara D, Myocarditis: New Engl J Med, 2000; 343; 1388-98
8.. Ammirati E, Cipriani M, Lilliu M, Survival and left ventricular function changes in fulminant versus non fulminant acute myocarditis: Circulation, 2017; 136(6); 529-45
9.. Ammirati E, Frigerio M, Adler ED, Management of acute myocarditis and chronic inflammatory cardiomyopathy: An expert consensus document: Circ Heart Fail, 2020; 13(11); e007405
10.. Ammirati E, Bizzi E, Veronese G, Immunomodulating therapies in acute myocarditis and recurrent/acute pericarditis: Front Med (Lausanne), 2022; 9; 838564
11.. Basso C, Myocarditis: N Engl J Med, 2022; 387(16); 1488-500
12.. Bowles NE, Ni J, Kearney DL, Detection of viruses in myocardial tissues by polymerase chain reaction. Evidence of adenovirus as a common cause of myocarditis in children and adults: J Am Coll Cardiol, 2003; 42; 466-72
13.. Polte CL, Bobbio E, Bollano E, Cardiovascular magnetic resonance in myocarditis: Diagnostics, 2022; 12(2); 399
14.. Asaumi Y, Yasuda S, Morii I, Favorable clinical outcome in patients with cardiogenic shock due to fulminant myocarditis supported by percutaneous extracorporeal membrane oxygenation: Eur Heart J, 2005; 26; 2185-92
15.. Baldetti L, Pagnesi M, Gramegna M, Intra-aortic balloon pumping in acute decompensated heart failure with hypoperfusion: From pathophysiology to clinical practice: Circ Heart Fail, 2021; 14(11); e008527
16.. Ogunbayo G, Olorunfemi O, Elbadawi A, Outcomes of intra-aortic balloon pump use in myocarditis complicated by cardiogenic shock: J Am Coll Cardiol, 2017; 69(11 Suppl.); 860
17.. Pozzi M, Banfi C, Grinberg D, Veno-arterial extracorporeal membrane oxygenation for cardiogenic shock due to myocarditis in adult patients: J Thorac Dis, 2016; 8(7); E495-502
18.. Vallabhajosyula S, O’Horo JC, Antharam P, Concomitant intra-aortic balloon pump use in cardiogenic shock requiring veno-arterial extracorpo-real membrane oxygenation: Circ Cardiovasc Interv, 2018; 11(9); e006930
19.. Zeng P, Yang C, Chen J, Comparison of the efficacy of ECMO with or without IABP in patients with cardiogenic shock: A meta-analysis: Front Cardiovasc Med, 2022; 9; 917610
20.. Van den Brink FS, Zivelonghi C, Vossenberg TN, VA-ECMO With IABP is associated with better outcome than VA-ECMO alone in the treatment of cardiogenic shock in ST-elevation myocardial infarction: J Invasive Cardiol, 2021; 33(5); E387-E92
21.. Nishi T, Ishii M, Tsujita K, Outcomes of venoarterial extracorporeal membrane oxygenation plus intra-aortic balloon pumping for treatment of acute myocardial infarction complicated by cardiogenic shock: J Am Heart Assoc, 2022; 11(7); e023713
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250