09 January 2024: Articles 
Delayed Emergence from Total Intravenous Anesthesia Following Posterior Spinal Correction and Fusion for Scoliosis: A Case Report
Patient complains / malpractice, Congenital defects / diseases
Osamu Hisatomi1ABCDEF*, Tetsuhiro Fujiyoshi2ABCDEF, Sho Shinotsuka1ABCDEF, Hirokazu SaiwaiDOI: 10.12659/AJCR.941563
Am J Case Rep 2024; 25:e941563
Abstract
BACKGROUND: Postoperative acute liver failure, a complication following spine surgery, can cause delayed emergence from total intravenous anesthesia. Here, we report a case of acute severe postoperative liver failure following posterior spinal correction and fusion in a patient with congenital scoliosis.
CASE REPORT: A girl’s congenital scoliosis worsened, and posterior spinal correction and fusion was scheduled. General anesthesia was induced with sevoflurane, fentanyl, target-controlled-infusion with propofol, and rocuronium. General anesthesia was maintained using target-controlled-infusion with propofol and remifentanil. The operation was completed with no remarkable complications. The operative time was 516 min and the anesthesia time was 641 min in the prone position. Emergence from anesthesia was poor, and it took 68 min to remove the tracheal tube after discontinuation of the anesthetic agents. The patient was drowsy and was transferred to her room in a general ward without reporting any pain, nausea, or dyspnea. On postoperative day 1, the results of laboratory investigations were suggestive of acute liver failure; contrast-enhanced computed tomography revealed a poorly enhanced area in the umbilical portion of the left liver lobe portal vein, indicating ischemic liver damage. Although no additional treatment was administered for acute liver failure, the patient recovered over time, and laboratory values normalized. No other postoperative complications were observed, and the patient was discharged on postoperative day 21.
CONCLUSIONS: Delayed emergence from general anesthesia may be due to acute liver failure following posterior spinal correction and fusion. There are several possible causes of postoperative liver failure, including anesthetics, prone position, and spinal surgery.
Keywords: Postoperative Complications, Delayed Emergence from Anesthesia, Liver Failure, Acute, Spinal Fusion, Scoliosis, Prone Position
Background
Posterior spinal correction and fusion (PSCF) is a major spinal surgery and a common surgical treatment for scoliosis [1]. Although prone positioning is necessary for spinal surgery, it is associated with various complications, many of which are caused by increased pressure on anterior structures [2]. Major postoperative complications of spinal surgery in the prone position include neurological deficits, chronic pain, infection, and bleeding [1–3], while minor complications include intestinal ileus and superior mesenteric artery syndrome [2,4,5]. Several causes of liver failure after PSCF have been reported. Intraoperative hypotension due to increased intrathoracic pressure in the prone position reportedly causes postoperative ischemic liver failure. Liver compression by the 4-point support frame of the prone-positioning surgical bed has also been reported as a cause of postoperative liver failure. However, reports on postoperative liver failure following PSCF without intraoperative hypotension or a 4-point support frame are limited. Intraoperative liver failure can be related to metabolic dysfunction and prolonged effects of anesthesia and cause delayed emergence from general anesthesia, which indicates prolonged anesthetic effects. Here, we report a case of postoperative acute severe liver failure following PSCF in a patient with scoliosis and delayed emergence from general anesthesia that was caused by prolonged anesthetics effect.
Case Report
A 15-year-old girl (height: 150 cm; weight: 32 kg) had congenital scoliosis. She had been followed up ever since scoliosis was first at 8 years of age. She had no neurological symptoms due to scoliosis, and no other congenital abnormalities were found. However, her scoliosis worsened, and PSCF was scheduled. She had no other congenital abnormalities and neurological symptoms due to scoliosis, but experienced slight dyspnea on exertion. She presented with congenital scoliosis between the 3rd thoracic vertebra and 1st lumbar vertebra, and a Cobb angle of 49° between the 6th and 11th thoracic vertebrae on spine radiography (Figure 1A). Abnormal findings included a low vital capacity of 1.03 L, which equated to 38.4% of the standard vital capacity. Her physical status, according to the American Society of Anesthesiologists, was class 2.
General anesthesia was induced with sevoflurane, fentanyl 50 μg, propofol at an effective site concentration of 3.0 μg/mL, and rocuronium 20 mg. General anesthesia was maintained using propofol at an effective site concentration of 2.0 to 2.5 μg/mL and remifentanil at 0.2 to 0.4 μg/kg/min. In addition to standard vital signs monitoring, continuous artery blood pressure at the left radial artery and continuous bispectral index (BIS) were monitored. Intraoperative neurological monitoring was performed using sensory- and motor-evoked potentials. PSCF between the 3rd thoracic vertebra and the 1st lumbar vertebra was completed with no remarkable complications (Figure 1B). The operative time was 516 min and the anesthesia time was 641 min in the prone position. The total doses of anesthetic administered were 1431 mg of propofol and 150 μg of fentanyl. The estimated blood loss was 880 g and her urine output was 150 mL. Fluid intake included 3360 mL of crystalloids, 900 mL of preoperative autologous blood, and 250 mL of intraoperative autologous blood obtained from a blood salvage device. The auto-RBC was administered when an intraoperative arterial gas test indicated that the hemoglobin concentration (Hb) was 8.3 g/dL. At the end of the surgery, the final Hb was 8.7 g/dL. Intravenous patient-controlled analgesia (ivPCA) was initiated 100 min before the end of anesthesia with fentanyl at 11 μg/kg/day. Emergence from anesthesia was poor, and it took 68 min to remove the tracheal tube after discontinuation of the anesthetic agents. The patient was drowsy but could open her eyes when her name was called. Although her consciousness status was poor, her general condition was stable. Her spontaneous respiration was adequate, the respiratory rate was 16 breaths per minute, and the tracheal tube was removed. Although she was drowsy, the hand-grip test revealed no abnormal neurological dysfunction, and sensory and motor testing of her lower extremities revealed normal results after the extubation. She was transferred to her room in a general ward without any reports of pain, nausea, or dyspnea.
On postoperative day (POD) 1, her consciousness status was alert and her general condition was stable despite delayed emergence from general anesthesia. The results of laboratory investigations were suggestive of acute liver failure: aspartate transaminase (AST) was 3113 IU/L, alanine transaminase (ALT) was 2235 IU/L, prothrombin time (PT) was 18.8 s, PT-international normalized ratio (INR) was 1.62, and platelet count was 61 000/μL (Table 1). Contrast-enhanced computed tomography (CT) revealed a poorly enhanced area in the umbilical portion of the left liver lobe portal vein, indicating ischemic liver damage. However, blood flow was preserved in the hepatic and portal veins (Figure 2). AST and ALT levels decreased, and platelet counts increased on POD2 (Table 1). Although no additional treatment was administered for acute liver failure, the patient recovered over time, and laboratory values normalized on POD19. No other postoperative complications were observed, and the patient was discharged on POD21.
Discussion
Several possible causes for acute postoperative liver failure exist [6–8], including administering anesthetic agents. Propofol-induced syndrome (PRIS) is strongly associated with a propofol dose exceeding 4 mg/kg/h and propofol administration for 48 h or more [9]. Most studies have demonstrated that PRIS occurs during propofol sedation in the intensive care unit. Although the total dose of propofol in our case was comparable to the dose in these reports, the duration of propofol infusion was much shorter. One case report showed that sevoflurane, a volatile anesthetic, had hepatotoxic effects and caused acute liver failure in an 11-year-old boy. Although administration of inhaled anesthetics is a differential diagnosis for acute liver failure, in our case sevoflurane was administered only for slow induction and for a short duration [10].
In a systematic review by Kwee et al of the prone position during surgery and its complications, reports on spinal surgery dominated the cited literature, and variable complications following spinal surgery were presented [2]. Cardiovascular compromise and postoperative vision loss have been reported in many articles, and hepatic dysfunction and ischemic hepatitis caused by increased central venous pressure have also been reported during spine surgery in the prone position [2]. Several causes of postoperative organ damage have been previously reported. Compression of abdominal organs using a prone-positioning support system can cause postoperative organ damage [1,4,5]. Liver ischemia is less likely to occur because the liver receives a rich blood supply from the portal vein and hepatic artery. However, the prone position and prone-positioning support devices decrease the hepatic blood supply and cause liver congestion owing to increased central venous pressure [2]. The prone position also decreases cardiac output and induces intra-operative hypotension [1]. Satomoto et al showed that prone-positioning support devices compressed the liver, resulting in postoperative liver failure [11]. The prone-positioning surgical bed has a device with 4-point support frames that supports the anterior thorax. This device compresses the liver and increases intrathoracic pressure. Yuen et al investigated the differences in the prone positioning support of the surgical bed that affected intraoperative hypotension and postoperative liver failure [5], suggesting that some frames that exerted no pressure on the patient’s anterior chest wall maintained hemodynamic status and reduced liver compression. Most reports have shown that postoperative liver failure following prone position surgery is caused by severe intraoperative hypotension in the prone position and liver compression by the 4-point support frames used in prone positioning. In some reports, intraoperative severe hypotension caused ischemic liver damage [4,5]. In our patient, intraoperative hemodynamics were completely stable and severe hypotension never occurred. The total urine volume of 150 mL for 641 min of anesthesia time was smaller than the intake volume of crystalloid and blood infusion, but the small urine volume did not indicate hypovolemic status, because 0.5 mL/kg/h of urine output was maintained during the operation. Intraoperative hemodynamics were completely stable and we used a prone-positioning surgical bed – the Trios® Surgical Table System (Mizuho Corporation, Tokyo, Japan) – that applied less pressure on the chest. Thus, in our patient, the cause of acute postoperative liver failure following PSCF may not have been severe hypotension or liver compression caused by the surgical bed.
Liver damage can be caused by forced correction of spinal alignment deformities [12]. Hepatic blood circulation is restricted by the dislocation of vessels and organs due to spinal alignment modifications; it is also inhibited by vessel and organ dislocation in the prone position. One possible cause of postoperative liver failure is repetitive liver compression caused by using a pedicle probe to excavate the screw holes. The surgical procedure of pedicle screw insertion places pressure on the anterior chest wall. During the insertion of each screw, the intrathoracic pressure increases, and the liver is compressed between the spine and anterior chest wall. In our patient, many screws were inserted, and transient intraoperative liver ischemia and compression may have caused postoperative acute liver failure.
Intraoperative ischemic liver damage can result in metabolic dys-function and prolonged effects of anesthesia. In our patient, 68 min were required before the tracheal tube could be removed after cessation of propofol administration, and the intraoperative BIS ranged from 40 to 60. Although the effective site concentration of propofol TCI was much lower than the sleep concentration and the BIS was 70 at extubation, delayed emergence was noted. Such delayed emergence from general anesthesia most likely indicates prolonged anesthetic effects due to acute liver failure resulting from decreased intraoperative hepatic blood flow and metabolic activity. Other causes of delayed emergence should also be considered. The total dosage of intraoperative propofol and fentanyl due to the long anesthesia time might have prevented clear emergence by the residual anesthetics effect, although the estimated anesthetics concentration was low enough to achieve alert consciousness after general anesthesia. Fentanyl administered by ivPCA for postoperative pain control was one of the possible causes of the delayed emergence. However, the postoperative blood concentration of fentanyl was adequate; the calculated blood concentration of fentanyl was not as high as at extubation, and she was alert on POD1.
Conclusions
Patients with delayed emergence from general anesthesia should be evaluated for acute liver failure following PSCF. There are several possible causes of postoperative liver failure, including administering anesthetics agents, prone positioning, and spinal surgery.
Tables
Table 1.. Laboratory data.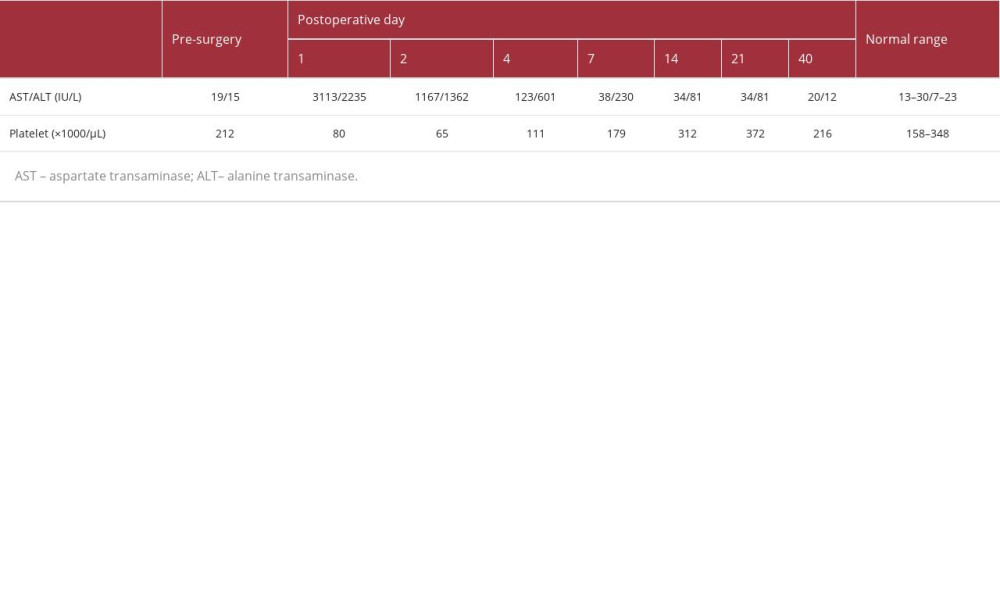
References:
1.. Keil LG, Himmelberg SM, Guissé NF, Nash AB, Fletcher ND, Stone JD, Complications following posterior spinal fusion for adolescent idiopathic scoliosis: A retrospective cohort study using the modified Clavien-Dindo-Sink system: Spine Deform, 2022; 10; 607-14
2.. Kwee MM, Ho Y-H, Rozen WM, The prone position during surgery and its complications: A systematic review and evidence-based guidelines: Int Surg, 2015; 100; 292-303
3.. Abcejo AS, Diaz Soto J, Castoro C, Profound obstructive hypotension from prone positioning documented by transesophageal echocardiography in a patient with scoliosis: A case report: A Case Rep, 2017; 9; 87-89
4.. Vasiliadis HS, Teuscher R, Kleinschmidt M, Temporary liver and stomach necrosis after lateral approach for interbody fusion and deformity correction of lumbar spine: Report of two cases and review of the literature: Eur Spine J, 2016; 25(Suppl. 1); 257-66
5.. Yuen VMY, Chow BFM, Irwin MG, Severe hypotension and hepatic dysfunction in a patient undergoing scoliosis surgery in the prone position.: Anaesth Intensive Care, 2005; 33; 393-99
6.. Rahbari NN, Garden OJ, Padbury R, Posthepatectomy liver failure: A definition and grading by the International Study Group of Liver Surgery (ISGLS): Surgery, 2011; 149; 713-24
7.. Sgro C, Clinard F, Ouazir K, Incidence of drug-induced hepatic injuries: A French population-based study: Hepatology, 2002; 36; 451-55
8.. Reuben A, Koch DG, Lee WM, Drug-induced acute liver failure: Results of a U.S. multicenter, prospective study: Hepatology, 2010; 52; 2065-76
9.. Vasile B, Rasulo F, Candiani A, Latronico N, The pathophysiology of propofol infusion syndrome: A simple name for a complex syndrome.: Intensive Care Med, 2003; 29; 1417-25
10.. Shriver MF, Zeer V, Alentado VJ, Mroz TE, Lumbar spine surgery positioning complications: A systematic review: Neurosurg Focus, 2015; 39; E16
11.. Bermúdez Barrezueta L, Benito Gutiérrez M, Acute liver failure after sevoflutane anesthesia in a pediatric patient: Rev Esp Anestesiol Reanin, 2019; 66; 474-77
12.. Satomoto M, Takagi Y, Igarashi H, Sato S, Hepatic infarction following prolonged prone position: Masui, 2006; 55; 1170-72
Figures
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








