11 October 2023: Articles 
Septic Arthritis of Cervical Spine Facet Joints: A Case Report and Review of Imaging
Rare disease
Hironori KitajimaDOI: 10.12659/AJCR.941578
Am J Case Rep 2023; 24:e941578
Abstract
BACKGROUND: Septic arthritis of the facet joint (SAFJ) has been considered a rare type of spinal infection. However, because of the aging of the population, the increase in compromised hosts, and the increase in MRI use in recent years, the number of reports has been increasing. We report the clinical progress of a rare case of septic arthritis of the cervical facet joint (SACFJ) with some imaging considerations, and we compare our findings with existing reports of SACFJ.
CASE REPORT: A 73-year-old Japanese woman presented with fever, paralytic symptoms, and paresthesia of the upper limbs. Here, we report a case of SACFJ in which MRI findings allowed early diagnosis, and a favorable course was obtained by conservative treatment with antibiotics. Although MRI performed 93 days after the initiation of treatment showed a slight residual signal change in the facet joints, no symptoms had recurred by the sixth month after hospital discharge.
CONCLUSIONS: If a patient develops neurological symptoms such as paralysis with fever and increased inflammatory response, the physician must consider the possibility of pyogenic spondylitis, including SACFJ, and order an MRI. Epidural abscess is almost inevitable in SACFJ, and surgical treatment, including abscess drainage, is required if spinal cord or paralytic symptoms progress. For patients with SACFJ, as well as pyogenic spondylitis, MRI may not be useful in determining treatment efficacy.
Keywords: Epidural Abscess, Magnetic Resonance Imaging, Pyogenic arthritis, Pyoderma gangrenosum, and Acne, Female, Humans, Aged, Zygapophyseal Joint, Arthritis, Infectious, Lumbar Vertebrae, Spondylitis, Cervical Vertebrae
Background
Septic arthritis of the facet joint (SAFJ) historically accounted for about 4% of all pyogenic spinal infections and has been considered a rare condition [1]. However, with the aging of the population, the increase in compromised hosts, and the increase in use of MRI in recent years, there have been an increasing number of reports of SAFJ, which now make up about 20% of pyogenic spinal infections [2]. However, SAFJ is generally not well known and is difficult to diagnose. SAFJ can be associated with severe sepsis and residual neuropathy; early diagnosis and appropriate treatment are essential [2,3].
Of these SAFJ infections, 86% to 97% are located in the lumbar region [2,3]. To the best of our knowledge, there have been only 15 reported cases of septic arthritis of the cervical facet joint (SACFJ) [4–16]. Here, we report a case of SACFJ that was diagnosed early by MRI, in which a favorable clinical course was achieved by conservative treatment with antibiotics. In addition, we evaluated SAFJ over time by CT and MRI.
Case Report
A 73-year-old Japanese woman’s chief concerns were numbness on the right forearm (ulnar side) and upper arm (extension side), and difficulty in moving the right finger. Her medical history was unremarkable. She did not smoke or drink. The patient had a fever of 37.5°C, hyposensitivity in the right C7 and C8 regions, muscular weakness in triceps brachii MMT4/5, wrist flexion MMT4/5, wrist extension MMT4/5, finger extension MMT2/5,and finger flexion MMT4/5 (Figure 1, Table 1). Laboratory tests showed WBC count 9600/µL, CRP count 7.58 mg/d, and elevated inflammatory markers. Simple X-ray and CT of the cervical spine showed only deformation in the cervical spine, but MRI of the cervical spine revealed a high signal change in the right facet joint and paraspinal muscle of C7/Th1 in the sagittal section of the STIR image. In the same horizontal section, epidural mass lesions were observed extending from the C6/7 and C7/Th1 intervertebral foramen to the spinal canal (Figure 2). Based on the above, the patient was diagnosed with C7/Th1 right SACFJ and cervical epidural abscess. Treatment with Cephem antibiotics was initiated in accordance with the treatment of pyogenic spondylitis. In this case, cefotiam 3 g/day, which is effective against gram-positive cocci and, to some extent, gram-negative rods, was used for initial intravenous antibiotic treatment. The dose of antimicrobials was adjusted according to renal function. Methicillin-sensitive
Discussion
For our patient, we performed CT and MRI over time for SACFJ and monitored progress. Reportedly, SALFJ-related bone destruction takes about one month to appear on simple X-rays, and bone destruction and epidural abscess take about 2 weeks to appear on CT [17,18], but signal change in soft tissues can be detected as early as 2 days after onset by MRI [19,20]. We found it difficult to make a diagnosis from clinical symptoms, laboratory tests, simple X-ray, and CT, but were able to reach a rapid diagnosis with the addition of MRI. We thus consider MRI useful for diagnosing early-stage SACFJ. However, on day 30 and day 93 after initiation of treatment, although symptoms and blood data had been normalized, the MRI signal change at the facet joint remained (Figures 3, 4). Residual MRI enhancement has also been reported even after normalization of laboratory tests and symptoms in pyogenic spondylitis, suggesting that MRI may be less useful for determining the effects of treatment [21]. MRI may not also be useful in determining treatment efficacy in SACFJ. In contrast, bone erosions and joint destruction that were not visible on CT at admission were confirmed by CT on the 10th day. The cervical spine CT on the 41st day showed no progression of bone destruction. Fusion of the facet joint was confirmed by CT on day 191, with no sign of cervical spine instability (Figure 5). We found that if sufficient quenching of the infection is achieved, destruction of the facet joints will also result in bony fusion.
We summarized the 15 cases of SACFJ that we found documented in the literature (Table 2) [4–16]. Most patients were male, and the average age was 61.2 years. Most of the infections were unilateral, with no notable skewing to either the right or left side. These results were similar to those reported for septic arthritis of the lumbar facet joint (SALFJ) [18]. The most common site of onset was at C1/C2, with 6 cases. Symptoms were similar to those for pyogenic spondylitis, including neck pain, fever, and neurological symptoms, with fever and unilateral neck pain particularly common at the start of SAFJ [5]. Similar to pyogenic spondylitis, the pathogenesis of SAFJ includes direct infiltration from surrounding reservoirs of infection [7] and hematogenous [5] and iatrogenic causes [7]. In about 30% of patients, SACFJ was associated with underlying diseases such as diabetes or cirrhosis. Similar to the reports for SALFJ, the most common causative organism was
Treatment included surgical treatment, but conservative treatment with antibiotics was selected in 7/15 cases (46%) reported for the cervical spine. Conservative treatment used antibiotics for more than 6 weeks, and most patients improved without dysfunction. In most reports, antimicrobials are selected to target MSSA and MRSA. Also, initially, they are more often empirically treated. In any case, using susceptible and appropriate antimicrobials is considered essential. However, epidural abscess of SACFJ accounted for up to 13 of the 15 cases (86%), and if spinal cord symptoms or paralytic symptoms progressed after conservative treatment, drainage techniques include surgical treatment were to be considered. Since the spinal canal of the cervical spine is narrower than that of the lumbar spine, symptoms related to the cervical spine tend to become more severe with neurological symptoms related to an epidural abscess [7]. In addition to draining the abscess, common surgical treatments are fusion surgery, including the Brooks procedure14, the Harms technique [7], and occipitocervical fusion [6] for C1/ C2, and laminectomy [3,10,13,16] for other parts of the spine.
Conclusions
SACFJ is associated with a high risk of septic shock, residual severe neurological symptoms, and cervical spine instability, so early diagnosis by MRI and treatment with antibiotic therapy are important. Epidural abscesses are extremely common with SACFJ, and surgical treatment, including drainage, is required if there is a progression of paralysis or other spinal cord symptoms. Our patient showed no signs of progression of paralysis or other spinal cord symptoms, and a good outcome was achieved through conservative treatment with antibiotics. For SACFJ, as well as pyogenic spondylitis, MRI may not be useful in determining treatment efficacy.
Figures
References:
1.. Halpin D, Gibson R, Septic arthritis of a lumbar facet joint: J Bone Joint Surg Br, 1987; 69-B(3); 457-59
2.. Narváez J, Nolla JM, Narváez JA, Spontaneous pyogenic facet joint infection: Semin Arthritis Rheum, 2006; 35(5); 272-83
3.. Muffoletto AJ, Ketonen LM, Mader JT, Hematogenous pyogenic facet joint infection: Spine (Phila Pa 1976), 2001; 26(14); 1570-76
4.. Tomoda Y, Kihara Y, Kozuma R, Tanaka K, Septic arthritis of the cervical facets: Unusual cause of neck pain: J Gen Fam Med, 2018; 19(4); 143-44
5.. Sethi S, Vithayathil MK, Cervical facet joint septic arthritis: A real pain in the neck: BMJ Case Rep, 2017; 2017; 28775081
6.. Kuyumcu G, Simpfendorfer CS, Babic M, Septic arthritis of an atlantoaxial facet joint with normal inflammatory markers: Case report and literature review: World Neurosurg, 2017; 98; 870.e11-870.e15
7.. Compes P, Rakotozanany P, Dufour H, Fuentes S, Spontaneous atlantoaxial pyogenic arthritis surgically managed: Eur Spine J, 2015; 24(Suppl. 4); S461-64
8.. Jones JL, Ernst AA, Unusual cause of neck pain: Septic arthritis of a cervical facet: Am J Emerg Med, 2012; 30(9); 2094.e1-4
9.. Stecher JM, El-Khoury GY, Hitchon PW, Cervical facet joint septic arthritis: A case report: Iowa Orthop J, 2010; 30; 182-87
10.. Michel-Batôt C, Dintinger H, Blum A, A particular form of septic arthritis: Septic arthritis of facet joint: Joint Bone Spine, 2008; 75(1); 78-83
11.. Sasaki K, Nabeshima Y, Ozaki A, Septic arthritis of the atlantoaxial joint: J Spinal Disord Tech, 2006; 19(8); 612-15
12.. Halla JT, Bliznak J, Hardin JG, Finn S, Septic arthritis of the C1–C2 lateral facet joint and torticollis: Pseudo-Grisel’s syndrome: Arthritis Rheum, 1991; 34(1); 84-88
13.. Kaye ID, Protopsaltis TS, Cervical facet joint infection and associated epidural abscess with streptococcus intermedius from a dental infection origin a case report and review: Bull Hosp Jt Dis, 2013; 74(3); 237-43
14.. Kobayashi T, Miyakoshi N, Abe E, Acute neck pain caused by septic arthritis of the lateral atlantoaxial joint with subluxation: A case report: J Med Case Rep, 2015; 9; 171
15.. Muffolerro AJ, Nader R, Westmark RM, Hematogenous pyogenic facet joint infection of the subaxial cervical spine. A report of two cases and review of the literature: J Neurosurg, 2001; 95(1 Suppl.); 135-38
16.. Takatori R, Fujiwara Y, Narita W, Septic Arthritis of a Cervical Facet Joint Leading to Tetraplegia: A Case Report and Review of the Literature: Journal of Spine Research, 2015; 6; 927-31
17.. Yoon J, Efendy J, Redmond MJ, Septic arthritis of the lumbar facet joint. Case and literature review: J Clin Neurosci, 2020; 71; 299-303
18.. Pilleul F, Garcia J, Septic arthritis of the spine facet joint: Early positive diagnosis on magnetic resonance imaging. Review of two cases: Joint Bone Spine, 2000; 67(3); 234-37
19.. Fujiwara A, Tamai K, Yamato M, Septic arthritis of a lumbar facet joint: Report of a case with early MRI findings: J Spinal Disord, 1998; 11(5); 452-53
20.. Doita M, Nishida K, Miyamoto H, Septic arthritis of bilateral lumbar facet joints: Report of a case with MRI findings in the early stage: Spine (Phila Pa 1976), 2003; 28(10); E198-202
21.. Kowalski TJ, Layton KF, Berbari EF, Follow-up MR imaging in patients with pyogenic spine infections: Lack of correlation with clinical features: Am J Neuroradiol [Internet], 2007; 28(4); 693-99
Figures
Tables
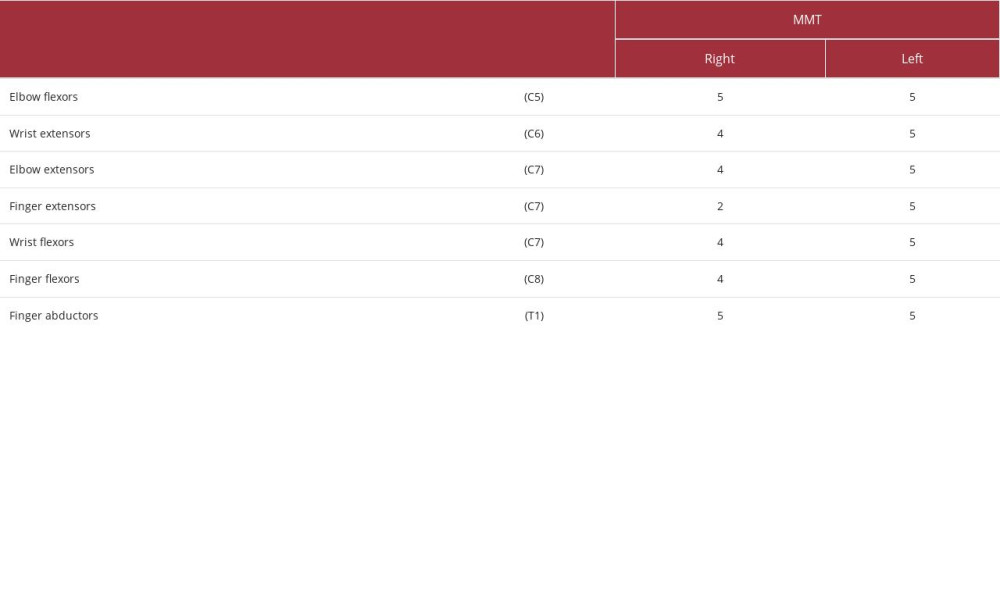 Table 1.. The patient’s neurologic fallout using myotomes. Evaluation by MMT (Manual Muscle Test).
Table 1.. The patient’s neurologic fallout using myotomes. Evaluation by MMT (Manual Muscle Test).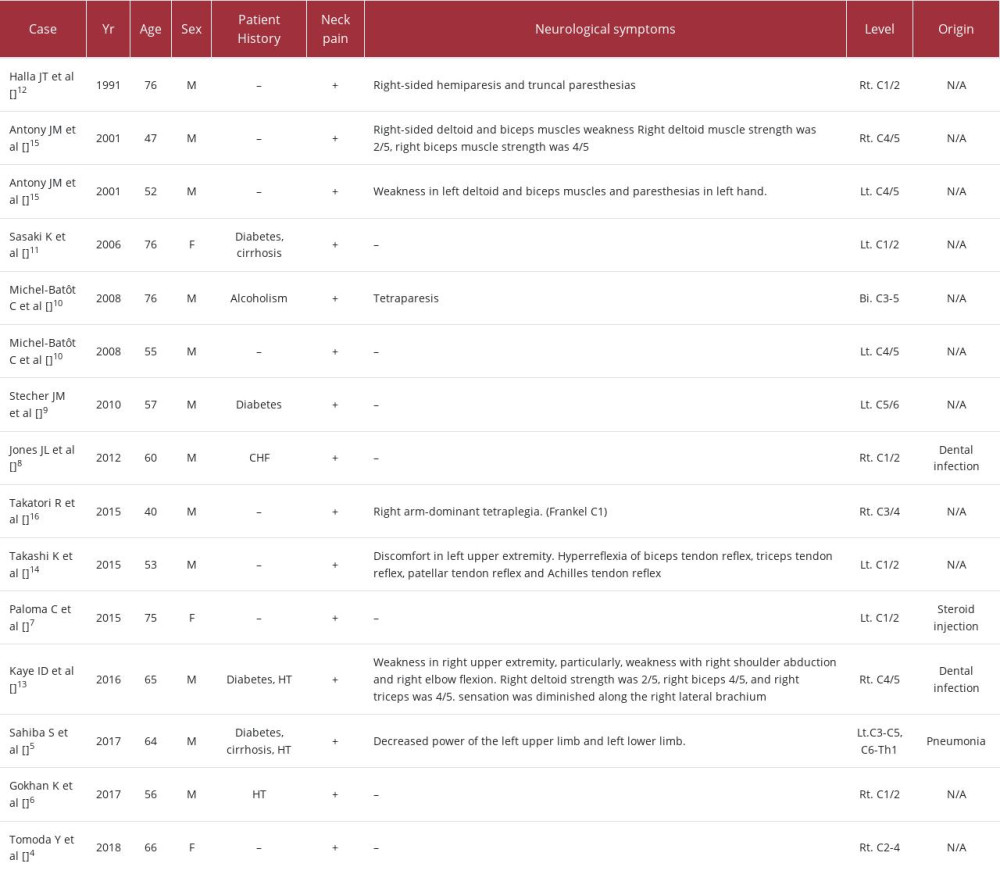 Table 2.. The 15 cases of septic arthritis of the cervical facet joint.
Table 2.. The 15 cases of septic arthritis of the cervical facet joint. .
. 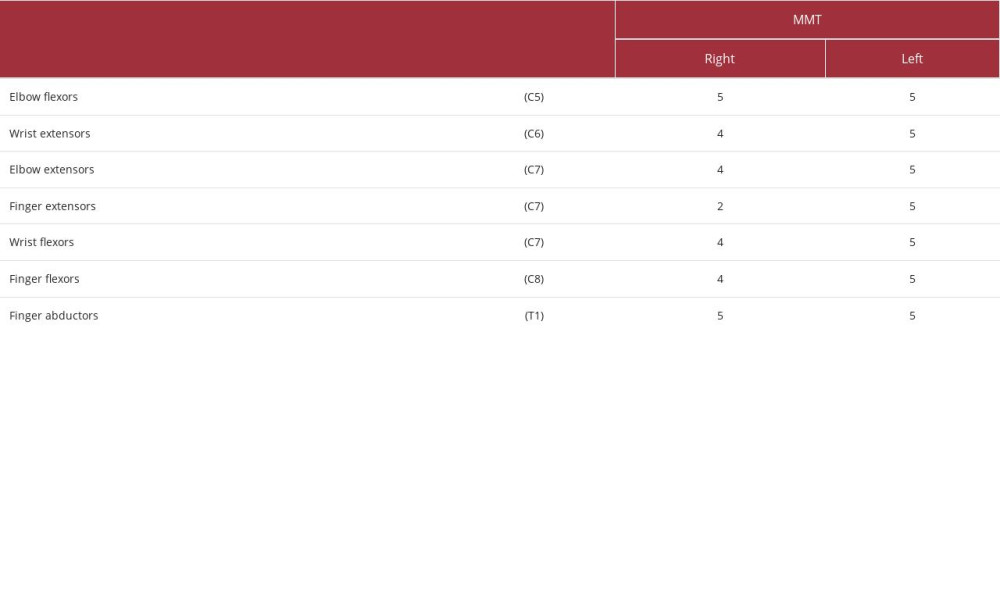 Table 1.. The patient’s neurologic fallout using myotomes. Evaluation by MMT (Manual Muscle Test).
Table 1.. The patient’s neurologic fallout using myotomes. Evaluation by MMT (Manual Muscle Test).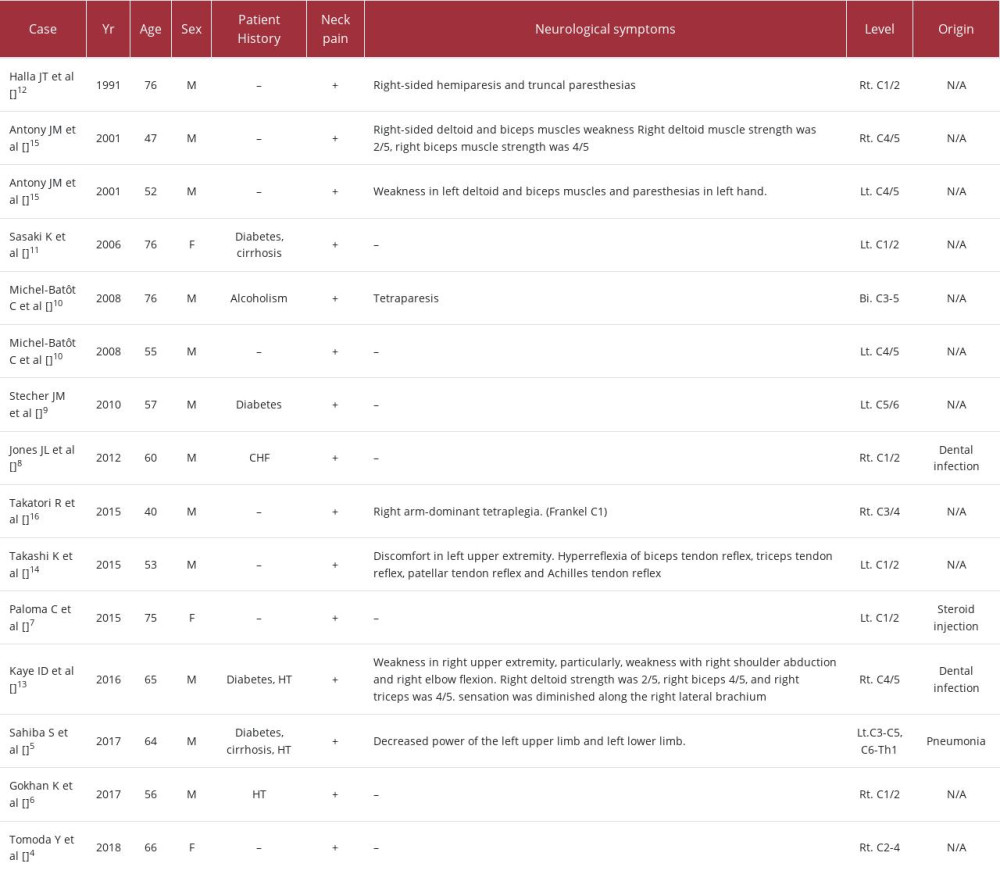 Table 2.. The 15 cases of septic arthritis of the cervical facet joint.
Table 2.. The 15 cases of septic arthritis of the cervical facet joint. .
. In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








