30 October 2023: Articles 
Use of a 2-Piece Small Diameter Implant in the Esthetic Zone in a Site of Chronic Residual Periapical Lesion: A Case Report with 1-Year Follow-Up and Histopathological Examination
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Patient complains / malpractice
Shahad B. AlsharifDOI: 10.12659/AJCR.941877
Am J Case Rep 2023; 24:e941877
Abstract
BACKGROUND: Replacing missing teeth in the anterior region of the jaw can be challenging due to the limited available interdental space. Improper selection or inadequate placement of a dental implant in this situation can affect the adjacent anatomical structures negatively. What if, in addition, a residual intraosseous chronic inflammatory lesion was present? The objective of this case report is to demonstrate the step-by-step surgical procedures of replacing a maxillary lateral incisor in a patient with a residual lesion with a satisfactory outcome.
CASE REPORT: A 63-year-old female patient with an extracted maxillary lateral incisor presented for implant placement. Radiographically, a residual periapical lesion with mild atrophy of the alveolar bone and fairly low density with sparse trabeculation was noted. Owing to the limited restorative space, a Straumann Bone Level Tapered Implant Ø2.9 mm (Small Cross-Fit connection, Roxolid, SLActive) was placed. Histopathological evaluation revealed a definitive diagnosis of periapical granuloma. After 1 year, the clinical examination revealed a successful outcome, and the patient was satisfied with the result.
CONCLUSIONS: This case report shows a successful clinical and radiographical outcome after 1 year of a 2-piece small diameter dental implant, the Straumann Bone Level Tapered Implant, diameter 2.9 mm, replacing a missing maxillary lateral incisor after enucleating the lesion with histopathological examination.
Keywords: case reports, Dental Implants, Pathology, Oral, Periapical Diseases, Treatment Outcome, Dentistry
Background
Compromised non-restorable teeth associated with periapical infection are usually indicated for extraction [1]. Historically, in the early studies, it was proposed that placing dental implants into these chronically infected sites is challenging due to the presence of microorganisms and proinflammatory mediators, which might affect the osseointegration process and lead to implant failure [2–7] or retrograde peri-implantitis [7,8]. It was hypothesized that the presence of periodontal and endodontic infection would be a predictive marker for dental implant infection and subsequently possible failure [8,9]. However, later animal experiments and clinical studies showed that, provided proper debridement and complete removal of the contaminated tissue in the infected site was performed prior to implant placement, successful osseointegration was achieved with comparable outcomes [10–15]. However, the extraction of non-restorable compromised teeth associated with periapical lesions does not necessarily eliminate the infection if proper socket curettage was not performed. This could result in residual lesions.
Placing dental implants to replace missing teeth of limited interdental space is quite challenging. In these situations, the selection of 1-piece mini-implants is mostly chosen. Recently, the Straumann Bone Level Tapered Implant ⌀2.9 mm, Small Cross-Fit connection (Straumann, Basel, Switzerland), was launched. It is indicated to replace teeth of esthetic concern with limited interdental space, mainly maxillary lateral incisors and mandibular incisors, according to the manufacturer’s claim. The advantage of this implant compared with that of the mini-implant is that it is a 2-piece dental implant, which makes it similar in characteristics to standard implants. However, studies reporting the outcome of this 2-piece small diameter implant are lacking. Therefore, the objective of this case report is to present the step-by-step surgical procedure for obtaining a favorable result of a dental implant placed in a chronically infected site with a residual lesion to replace a maxillary lateral incisor with limited interdental space using the Straumann Bone Level Tapered Implant ⌀2.9 mm. This report includes histological examination of the peri-radicular infected tissue, in addition to a 1-year follow-up with a successful outcome.
Case Report
CASE PRESENTATION:
A 63-year-old female patient presented to our dental clinic with a chief concern of “I would like to replace my missing front tooth with an implant.” A review of her medical history revealed high cholesterolemia and anxiety disorder. She was taking pravastatin 20 mg once daily, duloxetine 60 mg once daily, clonazepam 1 mg 3 times daily as needed, vitamin D 1500 mg daily, and fish oil 2000 mg daily. She was allergic to penicillin. No smoking habit was reported. Her dental history revealed multiple restorations (teeth #13, 15, 16, 22, 24, 31, 32, 33, 34, 37, 46), extractions (teeth #12, 14, 35, 36, 45, 47), removable partial denture (replacing teeth #35, 36), and previously placed implants (teeth #14, 45). She claimed to brush twice daily and flossing once daily. Extra-oral and intra-oral examinations revealed no pathology or abnormalities.
Upon clinical examination, the maxillary right lateral incisor, tooth # 12, was extracted 6 months ago (Figure 1). History of the extracted tooth disclosed multiple recurrent periapical abscesses with excursive pain and swelling extending extra-orally and involving the eyelid, with blurred vision, that did not heal despite the past dental treatment, which included incision, drainage, and a course of antibiotic, followed by root canal treatment. Subsequently, the patient’s general dentist decided to extract the tooth, and the patient was referred to our periodontal clinic for implant surgery. The periapical radiograph showed a round radiolucent intraosseous lesion with a well-defined radiopaque border occupying the area of the extracted tooth #12, approximately 1.8 cm in diameter (Figure 1). Cone-beam computed tomography was taken for further assessment (iCAT scanner, Imaging Sciences International, Hatfield, PA, USA). The obtained image was assessed using OnDemand 3D Imaging Software (Cybermed, Seoul, South Korea). The radiology report indicated mild atrophy of the edentulous alveolar bone in the region of tooth #12, with adequate alveolar bone height and width for implant placement. However, the overall density of the maxillary bone was fairly low, and the bony trabeculation was sparse to be considered during implant planning and placement surgery. Accordingly, implant placement surgery was planned and, based on the limited available restorative space, the Straumann Bone Level Tapered Implant ⌀2.9 mm (Small Cross-Fit connection, Roxolid, SLActive) was chosen for placement. Subsequently, the surgical guide was fabricated.
SURGICAL PROCEDURE:
The patient was pre-medicated with the antibiotic erythromycin 500 mg orally twice a day for a course of 10 days, which was started the day before the surgical procedure. Surgery was performed under local anesthesia using lidocaine hydrochloride 2% with 1: 100.000 epinephrine (2% Xylocaine Dental, Novocol Pharmaceutical of Canada, Inc., Ontario, Canada). The procedure started with a crestal incision over the edentulous area of tooth #12 with a sulcular incision over the adjacent teeth, distal of tooth #11 and mesial of tooth #13. A distal vertical releasing incision was made at the mesial line angle of tooth #13. A full-thickness mucoperiosteal flap was elevated. Bony fenestration was detected at the buccal plate of the alveolar bone (Figure 2). A trephine bur was used at the fenestration area to create access to the intraosseous lesion (Figure 3). After the access was created through the alveolar bone, the tissue lining the lesion was removed, placed in formalin, and sent to the oral pathology laboratory for histopathology assessment. The bony housing of the lesion was debrided with a bone curette and irrigated with sterile water to ensure complete removal of the soft tissue lining. After complete debridement, a tooth-supported surgical guide was placed after confirming the restorative position in periapical radiograph (Figure 4), and the implant bed was prepared following the manufacture’s guidelines. The Straumann Basic Surgical Cassette was used to create the osteotomy, first by using the needle drill (diameter 1.6 mm), followed by the pilot drill (diameter 2.2 mm) to a depth of 6 mm. An alignment pin was placed in the osteotomy to confirm implant axis orientation; then, the drilling continued to the desired final depth. As the bone density was soft, no profile drilling or bone tapping was needed. After the implant bed was completely prepared, a position indicator was used to confirm the implant’s positioning and angulation (Figure 5).
Next, the bony housing of the intraosseous lesion was filled with 0.5 cc of allograft 50/50 cortico-cancellous particulate bone (AlloOss; ACE Surgical Supply Co., Inc., MA, USA); then, the Straumann Bone Level Tapered Implant (small CrossFit, Roxolid, SLActive) with a diameter of 2.9 mm and length of 10 mm was placed with an insertion torque of 25 Ncm, followed by a healing abutment (3.5 mm). The buccal plate was augmented with further particulate bone graft covered by a resorbable collagen membrane of 15×20 mm (ConForm; ACE Surgical) (Figure 6). The mucoperiosteal flap was repositioned and sutured using 4-0 Cytoplast PTFE suture (Osteogenics Lubbock, TX, USA), with a simple interrupted technique. Lastly, a peri-apical radiograph was taken (Figure 7). A summary checklist of the step-by-step surgical procedures is presented in Table 1. Chlorhexidine gluconate 0.12% mouthwash twice daily for 10 days was prescribed. Sutures were removed after 1 week. Healing progressed well and was uneventful. An Essix retainer was delivered to replace the missing incisor temporarily during the osseointegration period for esthetic purposes (Figure 8). After 4 months, osseointegration was achieved and the patient was referred to her restorative dentist for the restorative treatment.
HISTOPATHOLOGICAL EVALUATION:
After staining the obtained tissue with hematoxylin and eosin, it was examined under a light microscope (Nikon Eclipse Ci microscope; Nikon Instruments Inc., Nikon, Japan) at ×10 and ×100 magnification. The microscopic examination revealed dense fibrous connective tissue with patchy chronic inflammatory infiltrate, blood capillaries, and interspersed fibroblasts. Numerous cholesterol clefts had associated multi-nucleated giant cells, extravasated red blood cells, and reactive bone spicules (Figure 9), leading to a definitive diagnosis of periapical granuloma.
FOLLOW-UP:
After 1 year, the patient presented for follow-up. Clinical examination revealed a successful outcome, based on the criteria of Misch et al [16]. The dental implant was producing no pain, as reported by the patient, and periodontal probing around the dental implant ranged from 2 to 4 mm. There was no bleeding on probing, no exudate, no mobility detected, and no thread exposure noticed, and the radiographic examination showed <2 mm of radiographic bone loss (Figure 10). Bone loss was assessed by measuring the distance between the neck of the implant fixture to the first bone to implant contact. The patient was satisfied and pleased with the outcome.
Discussion
Replacing missing teeth with limited mesiodistal bone width is always challenging. This is usually the case when replacing maxillary lateral incisors and mandibular incisors. Placing standard diameter dental implants in these cases can negatively affect the surrounding structures, which includes destruction of the interproximal bone and the periodontal ligament of the adjacent tooth [17], increased chance for thread exposure [18], and crestal bone loss of the implant and the adjacent natural teeth [19–22]. Thus, a minimum distance of 1.5 mm between the implant and the adjacent tooth was found to be necessary to avoid these negative consequences and maintain a stable functional and esthetic result [23]. Narrow-diameter implants and mini-implants have been introduced as an alternative treatment to standard implants for patients with limited mesiodistal bone width. Dental implants of diameter 3 to 3.4 mm are considered narrow-diameter implants [24], while mini-implants are 1-piece implants with a diameter of <3 mm [25,26].
Several studies reported that the narrower the implants’ diameter, the lower the survival outcome [27–30]. Additionally, mechanical studies showed that the narrower the diameter, the higher the risk of fracture with torsional loads [31]. Moreover, the fracture of mini-implants during insertion can occur even with a small amount of insertion torque [32]. However, other studies reported long-term outcomes that are similar to those of standard-diameter implants [33,34]. Despite these similar outcomes, the main drawback of mini-implants is that they are 1-piece implants. The flexibility of 2-piece narrow implants, which permits various prosthetic designs, has been reported to be successful [35–37]. However, all narrow-diameter implants assessed in these studies were of a diameter ³3 mm. Some cases have very limited mesiodistal width, which might require implants narrower than 3 mm. The present case used a 2.9-mm 2-piece Straumann implant, which is used for narrow interdental spaces in the anterior region, most specifically, for maxillary lateral incisors and mandibular incisors.
The present case shows the 1-year clinical and radiographical follow-up of a 2-piece small diameter implant, the Straumann Bone Level Tapered Implant ⌀2.9 mm, which replaced a missing maxillary lateral incisor, associated with chronic infection. Despite the presence of the residual infection within the alveolar bone, there was no biological impairment in the bone during the healing phase, with successful 1-year outcome. This could be attributed to the rigorous debridement of the infectious lesion before placing the dental implant, which was stressed in the literature [10–15]. However, a recent animal experimental study that histologically investigated the effect of periapical lesion debridement before implant placement concluded that complete removal of the granulation tissue is not essential to achieve successful osseointegration of the implants [38]. However, the interpretation of this result should be done with caution, as it was an animal study performed on dogs. Moreover, a systematic review stated that the nature of the infection that caused the alveolar bone lesion might affect the outcome of the implant placed in the area, and the authors pointed out the deficiency of reliable data in this concern [39].
In the present case, the histopathological diagnosis for the residual alveolar lesion was periapical granuloma, which is one of the most common periapical lesions [40,41]. Periapical granuloma can be defined as chronic inflammation at the apex of a necrotic tooth consisting of granulation tissue and chronic inflammatory cells infiltrate. Radiographically, it usually appears as periapical radiolucency with well- or ill-defined margins and might be associated with radiopaque borders, which was consistent with the present case. Treatment of periapical granuloma is based on the restorability of the associated tooth, either non-surgical root canal treatment or extraction, with follow-up examinations to monitor the healing of the lesion. However, if during follow-up the lesion failed to heal, assessment of the endodontic treatment is suggested to evaluate possible causes to be corrected with non-surgical retreatment, apicectomy, or even extraction, while if the tooth was originally extracted owing to restorability reasons, surgical intervention might be needed to enucleate the lesion and submit the retrieved tissue for histopathological examination for definitive diagnosis [42–44]. This was the situation in this case report, as the lesion failed to resolve or show signs of healing even after 6 months of the extraction; thus, surgical intervention was planned accordingly.
Follow-up and continued assessment of edentulous sites that are planned for future implants placement is encouraged. In addition, long-term maintenance of an implant-supported pros-thesis is critical for continued success [45]. A dental implant maintenance program is suggested to include oral microbiota assessment, as peri-implant microbiota was found to be different than periodontal microbiota [46]. Studies have found that some compounds, such as probiotics and chitosan, can modify the microbiota of dental implants, and thus, possibly the clinical and microbiological parameters [46,47]. Future research and clinical trials for these compounds are suggested to investigate their effect and applicability as adjuncts in long-term dental implant health.
There are treatment options to replace maxillary missing lateral incisors other than implant placement; these includes canine substitution utilizing orthodontic forces followed by a restorative procedure to mimic the lateral incisor shape [48], tooth-supported restoration [49], and removable partial dentures [50]. In the present case, after clinical examination and treatment options were discussed with the patient, dental implant placement was chosen. Despite the reported successful 1-year result, longer follow-up time is needed to determine the long-term outcome of the Straumann Bone Level Tapered Implant ⌀2.9 mm (Small Cross-Fit connection, Roxolid, SLActive) in sites with a residual intraosseous lesion.
Conclusions
This case report showed the 1-year successful outcome of a small diameter 2-piece dental implant, the Straumann Bone Level Tapered Implant ⌀2.9 mm. A narrow-diameter 2-piece implant was a reliable treatment option in this case of limited inter-dental space in the anterior region and site with chronic infection, as the supporting gingival tissue and marginal bone were stable, with no signs of peri-implant disease. However, further studies with a larger number of implants and longer follow-up time are needed to evaluate the long-term outcomes, as data are lacking.
Figures
References:
1.. Fu L, Du L, Qi J, Immediate implant placement in posterior sockets with periapical infection and bone defects: Three case reports: J Oral Implantol, 2022; 48; 500-6
2.. Alsaadi G, Quirynen M, Komarek A, van Steenberghe D, Impact of local and systemic factors on the incidence of oral implant failures, up to abutment connection: J Clin Periodontol, 2007; 34; 610-17
3.. Becker W, Becker BE, Guided tissue regeneration for implants placed into extraction sockets and for implant dehiscences. Surgical techniques and case reports: Int J Periodontics Restorative Dent, 1990; 10; 376-91
4.. Barzilay I, Immediate implants. Their current status: Int J Prosthodont, 1993; 6; 169-75
5.. Rosenquist B, Grenthe B, Immediate placement of implants into extraction sockets: Implant survival: Int J Oral Maxillofac Implants, 1996; 11; 205-9
6.. Schwartz-Arad D, Chausu G, The ways and wherefores of immediate placement of implants into fresh extraction sites: A literature review: J Periodontol, 1997; 68; 915-23
7.. Quirynen M, Vogels R, Alsaadi G, Predisposing conditions for retrograde peri-implantitis, and treatment suggestions: Clin Oral Implants Res, 2005; 16; 599-608
8.. Ayangco L, Sheridan PJ, Development and treatment of retrograde periimplantitis involving a site with a history of failed endodontic and apicoectomy procedures: A series of reports: Int J Oral Maxillofac Implants, 2001; 16; 412-17
9.. Polizzi G, Grunder U, Goené R, Immediate and delayed implant placement into extraction sockets: A 5-year report: Clin Implant Dent Relat Res, 2000; 2; 93-99
10.. Fugazzotto P, A retrospective analysis of immediately placed implants in 418 sites exhibiting periapical pathology: Results and clinical considerations: Int J Oral Maxillofac Implants, 2012; 27; 194-202
11.. Fugazzotto PA, A retrospective analysis of implants immediately placed in sites with and without periapical pathology in sixty-four patients: J Periodontol, 2012; 83; 182-86
12.. Marconcini S, Barone A, Gelpi F, Immediate implant placement in infected sites: a case series: J Periodontol, 2013; 84; 196-202
13.. Jung RE, Zaugg B, Philipp AO, A prospective, controlled clinical trial evaluating the clinical radiological and aesthetic outcome after 5 years of immediately placed implants in sockets exhibiting periapical pathology: Clin Oral Implants Res, 2013; 24; 839-46
14.. Zuffetti F, Capelli M, Galli F, Post-extraction implant placement into infected versus non-infected sites: A multicenter retrospective clinical study: Clin Implant Dent Relat Res, 2017; 19; 833-40
15.. Chrcanovic BR, Martins MD, Wennerberg A, Immediate placement of implants into infected sites: A systematic review: Clin Implant Dent Relat Res, 2015; 17; e1-e16
16.. Misch CE, Perel ML, Wang HL, Implant success, survival, and failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference: Implant Dent, 2008; 17; 5-15
17.. Cardaropoli G, Lekholm U, Wennström JL, Tissue alterations at implant-supported single-tooth replacements: A 1-year prospective clinical study: Clin Oral Implants Res, 2006; 17; 165-71
18.. Romeo E, Lops D, Amorfini L, Chiapasco M, Clinical and radiographic evaluation of small-diameter (3.3-mm) implants followed for 1–7 years: A longitudinal study: Clin Oral Implants Res, 2006; 17; 139-48
19.. Tarnow DP, Cho SC, Wallace SS, The effect of inter-implant distance on the height of inter-implant bone crest: J Periodontol, 2000; 71; 546-49
20.. Tarnow DP, Magner AW, Fletcher P, The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla: J Periodontol, 1992; 63; 995-96
21.. Choquet V, Hermans M, Adriaenssens P, Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region: J Periodontol, 2001; 72; 1364-71
22.. Gastaldo JF, Cury PR, Sendyk WR, Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla: J Periodontol, 2004; 75; 1242-46
23.. Grunder U, Gracis S, Capelli M, Influence of the 3-D bone-to-implant relationship on esthetics: Int J Periodontics Restorative Dent, 2005; 25; 113-19
24.. Quek CE, Tan KB, Nicholls JI, Load fatigue performance of a single-tooth implant abutment system: Effect of diameter: Int J Oral Maxillofac Implants, 2006; 21; 929-36
25.. Shatkin TE, Shatkin S, Oppenheimer BD, Oppenheimer AJ, Mini dental implants for long-term fixed and removable prosthetics: A retrospective analysis of 2514 implants placed over a five-year period: Compend Contin Educ Dent, 2007; 28; 92-99
26.. Bulard RA, Vance JB, Multi-clinic evaluation using mini-dental implants for long-term denture stabilization: A preliminary biometric evaluation: Compend Contin Educ Dent, 2005; 26; 892-97
27.. Albrektsson T, Gottlow J, Meirelles L, Survival of NobelDirect implants: An analysis of 550 consecutively placed implants at 18 different clinical centers: Clin Implant Dent Relat Res, 2007; 9; 65-70
28.. Ortega-Oller I, Suárez F, Galindo-Moreno P, A meta-analysis based on prospective clinical trials: J Periodontol, 2014; 85; 569-80
29.. Renouard F, Nisand D, Impact of implant length and diameter on survival rates: Clin Oral Implants Res, 2006; 17; 35-51
30.. Winkler S, Morris HF, Ochi S, Implant survival to 36 months as related to length and diameter: Ann Periodontol, 2000; 5; 22-31
31.. Sfondrini MF, Gandini P, Alcozer R, Failure load and stress analysis of orthodontic miniscrews with different transmucosal collar diameter: J Mech Behav Biomed Mater, 2018; 87; 132-37
32.. Sreenivasagan S, Subramanian AK, Nivethigaa B, Assessment of insertion torque of mini-implant and its correlation with primary stability and pain levels in orthodontic patients: J Contemp Dent Pract, 2021; 22; 84-88
33.. Cordaro L, Torsello F, Mirisola Di Torresanto V, Rossini C, Retrospective evaluation of mandibular incisor replacement with narrow neck implants: Clin Oral Implants Res, 2006; 17; 730-35
34.. Degidi M, Piattelli A, Carinci F, Clinical outcome of narrow diameter implants: A retrospective study of 510 implants: J Periodontol, 2008; 79; 49-54
35.. Galindo-Moreno P, Nilsson P, King P, Clinical and radiographic evaluation of early loaded narrow diameter implants – 1-year follow-up: Clin Oral Implants Res, 2012; 23; 609-16
36.. Lee JS, Kim HM, Kim CS, Long-term retrospective study of narrow implants for fixed dental prostheses: Clin Oral Implants Res, 2013; 24; 847-52
37.. Maiorana C, King P, Quaas S, Clinical and radiographic evaluation of early loaded narrow-diameter implants: 3 years follow-up: Clin Oral Implants Res, 2015; 26; 77-82
38.. Rea M, Bengazi F, Velez JU, Implants placed into alveoli with periapical lesions: An experimental study in dogs: Oral Maxillofac Surg, 2021; 25; 351-57
39.. Waasdorp JA, Evian CI, Mandracchia M, Immediate placement of implants into infected sites: A systematic review of the literature: J Periodontol, 2010; 81; 801-8
40.. Peters E, Lau M, Histopathologic examination to confirm diagnosis of peri-apical lesions: A review: J Can Dent Assoc, 2003; 69; 598-600
41.. Gbolahan O, Fatusi O, Owotade F, Clinicopathology of soft tissue lesions associated with extracted teeth: J Oral Maxillofac Surg, 2008; 66; 2284-89
42.. Regezi JA, Sciubba JJ: Oral pathology: Clinical pathologic correlations, 1999, Philadelphia (NY), W. B Saunders Company
43.. Flucke U, Thompson LD: Head and neck pathology, 2019, Philadelphia, Elsevier
44.. Neville BW, Damm DD, Allen CM, Chi AC: Color atlas of oral and maxillofacial diseases, 2018, Philadelphia, Elsevier Inc
45.. Hatzimanolakis P, Tsourounakis I, Kelekis-Cholakis A, Dental implant maintenance for the Oral Healthcare Team: Compend Contin Educ Dent, 2019; 40; 424-29 ; quiz 430
46.. Butera A, Pascadopoli M, Pellegrini M, Oral microbiota in patients with peri-implant disease: A narrative review: Applied Sciences, 2022; 12; 3250
47.. Divakar DD, Jastaniyah NT, Altamimi HG, Enhanced antimicrobial activity of naturally derived bioactive molecule chitosan conjugated silver nanoparticle against dental implant pathogens: Int J Biol Macromol, 2018; 108; 790-97
48.. Kokich VO, Kinzer GA, Managing congenitally missing lateral incisors. Part I: Canine substitution: J Esthet Restor Dent, 2005; 17; 5-10
49.. Kinzer GA, Kokich VO, Managing congenitally missing lateral incisors. Part II: Tooth-supported restorations: J Esthet Restor Dent, 2005; 17; 76-84
50.. Friel T, Waia S, Removable partial dentures for older adults: Prim Dent J, 2020; 9; 34-39
Figures
Tables
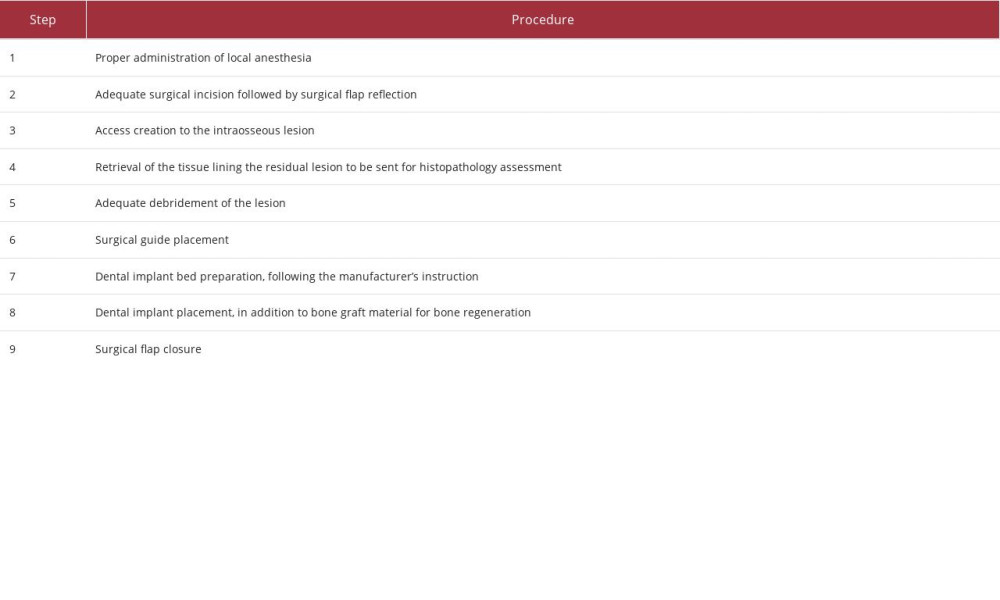 Table 1.. Summary checklist of the step-by-step surgical procedures performed to replace a maxillary lateral incisor associated with limited interdental space and a residual intraosseous lesion.
Table 1.. Summary checklist of the step-by-step surgical procedures performed to replace a maxillary lateral incisor associated with limited interdental space and a residual intraosseous lesion.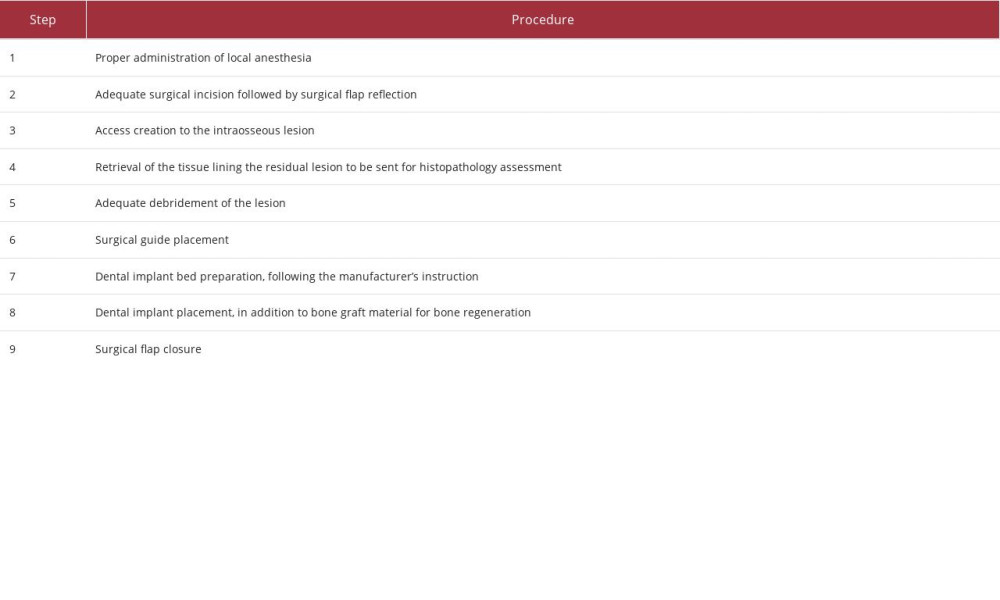 Table 1.. Summary checklist of the step-by-step surgical procedures performed to replace a maxillary lateral incisor associated with limited interdental space and a residual intraosseous lesion.
Table 1.. Summary checklist of the step-by-step surgical procedures performed to replace a maxillary lateral incisor associated with limited interdental space and a residual intraosseous lesion. In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








