27 December 2023: Articles 
Prolonged Anhepatic State as a Bridge to Retransplantation: A Challenging Case of a 35-Year-Old Male Liver Transplant Patient with a Temporary Portacaval Shunt
Management of emergency care
David Richer Araujo Coelho1ABEF*, Rogerio Oliveira da Luz1AE, Samanta Teixeira Basto2BE, Claudia Cristina Tavares de Sousa2E, Henry Pereira da Silva1E, Eduardo de Sousa Martins Fernandes2E, Anderson Brito-Azevedo2AEDOI: 10.12659/AJCR.941933
Am J Case Rep 2023; 24:e941933
Abstract
BACKGROUND: Liver transplantation is a life-saving intervention for patients with a diagnosis of acute liver failure or end-stage liver disease. Despite advances in surgical techniques and immunosuppressive therapies, primary nonfunction remains a concern, often necessitating retransplantation. In these scenarios, the anhepatic state, achieved through total hepatectomy with a temporary portacaval shunt, serves as a bridge to retransplantation. However, the challenge lies in the uncertain survival period and several potential complications associated with this procedure.
CASE REPORT: We present a case of a 35-year-old male patient with autoimmune hepatitis who underwent liver transplantation from a deceased donor. Seven days later, he experienced acute liver failure, leading to an urgent listing for retransplantation. To prevent the intense systemic inflammatory response, the patient underwent a total hepatectomy with a temporary portacaval shunt while awaiting another graft and endured a 57-h anhepatic state. On day 17 following retransplantation, he had cerebral death due to a hemorrhagic stroke.
CONCLUSIONS: This case underscores one of the most prolonged periods of anhepatic state as a bridge to retransplantation, highlighting the complexities associated with this technique. The challenges include sepsis, hypotension, coagulopathy, metabolic acidosis, renal failure, electrolyte disturbances, hypoglycemia, and hypothermia. Vigilant monitoring and careful management are crucial to improve patient outcomes. Further research is needed to optimize the duration of the anhepatic state and minimize complications for liver transplantation recipients.
Keywords: case reports, Intensive Care Units, Liver Transplantation, Hepatectomy, Portacaval Shunt, Surgical, Reoperation
Background
Liver transplantation (LT) offers a life-saving intervention for patients with acute liver failure or end-stage liver disease [1]. While surgical and immunosuppressive advancements have improved LT outcomes, LT remains a complex procedure with potential complications [2]. One of the most significant challenges is primary nonfunction, which can require total hepatectomy, but retransplantation (reLT) depends on organ availability [3]. A temporary portacaval shunt (TPCS), known as an anhepatic state, has been used as a bridge to retransplantation in those cases [4,5].
Since Ringe et al (1988) first performed a total hepatectomy with a TPCS to stabilize a patient with fulminant hepatic failure while awaiting reLT [6], there have been several reports in the literature of both successful and unsuccessful cases [7–34]. However, there is still no consensus regarding the maximum duration of the anhepatic state that can be safely tolerated, given potential complications such as sepsis, hypotension, coagulopathy, metabolic acidosis, renal failure, electrolyte disturbances, hypoglycemia, and hypothermia [6,7,12,14].
Considering the risks associated with the anhepatic state [6,7,12,14], monitoring clinical and laboratory parameters, including infection, hemodynamics, coagulation status, renal function, metabolic alterations, and body temperature, is imperative. Here, we report a case of a 35-year-old man with autoimmune hepatitis who underwent a 57-h anhepatic state with a TPCS as a bridge to retransplantation, one of the most prolonged periods reported. We describe the patient’s clinical presentation, diagnosis, and management strategies during this life-threatening period in the Intensive Care Unit (ICU).
Case Report
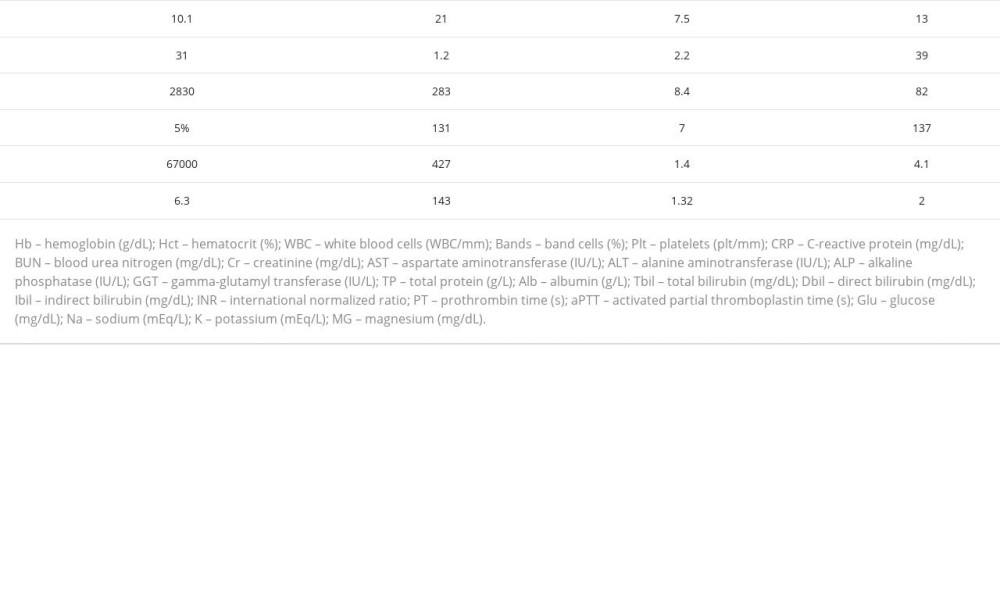
A 35-year-old man with a diagnosis of autoimmune hepatitis who had previously been managed with diuretic therapy for refractory ascites and experienced 2 episodes of upper gastrointestinal bleeding was admitted to the hospital for LT from a deceased donor. The patient had a Child-Turcotte-Pugh score of C and a Model for End-Stage Liver Disease (MELD) score of 38. Upon admission, laboratory findings indicated anemia, thrombocytopenia, elevated liver function tests, hypoalbuminemia, and increased total and direct bilirubin (Table 1). The donor was a 48-year-old woman with hypertension who died from a hemorrhagic stroke.
LT was performed using the conventional technique, with ligation of the splenic artery and a choledochal-choledochal anastomosis, without complications. The total ischemia time was 4 h and 29 min, cold ischemia time was 4 h and 1 m, warm ischemia time was 28 min, and the anhepatic phase was 44 min. During the surgery, 3000 mL of crystalloid, 100 mL of albumin, and 1 unit of packed red blood cells were administered. Surgical prophylaxis included ceftriaxone and fluconazole.
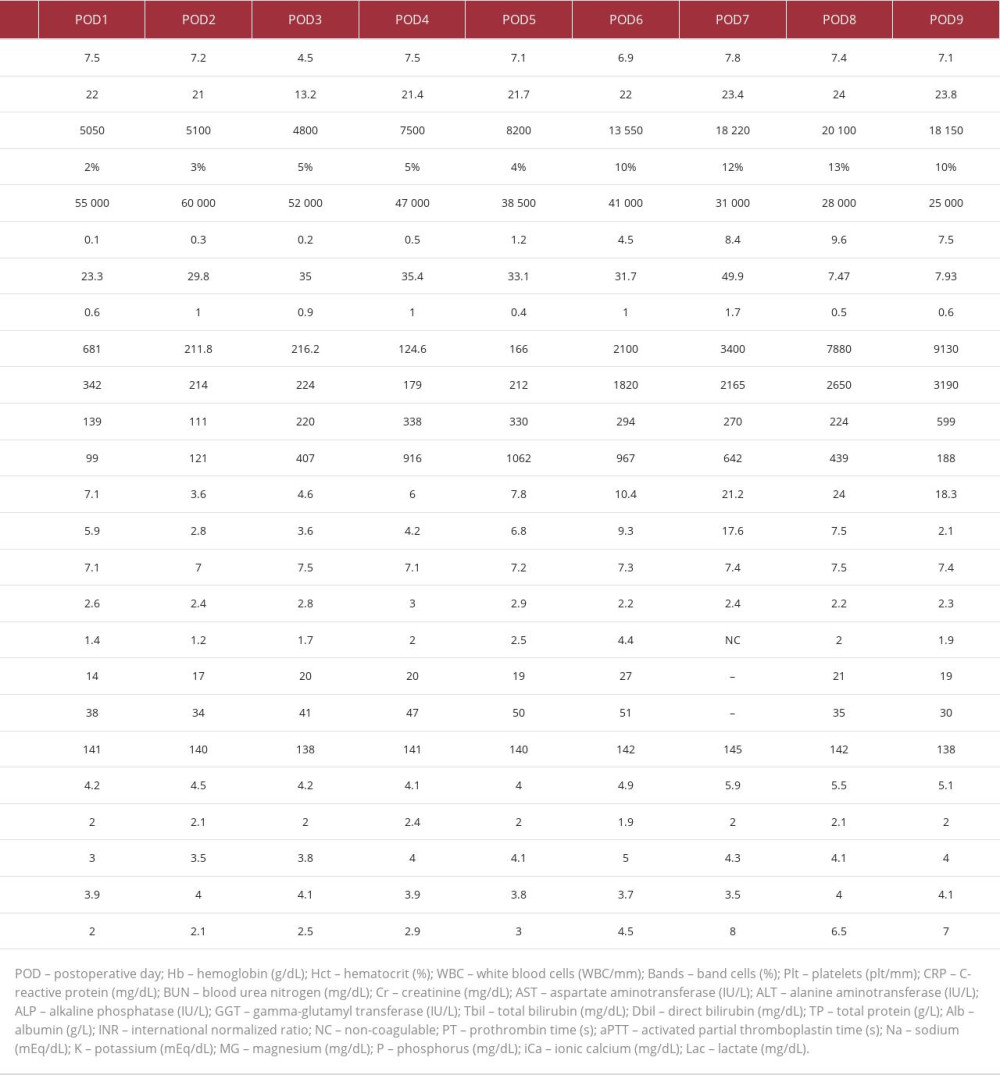
Upon admission to the ICU, the patient received low-dose vasopressor support and oxygen via a nasal catheter. He presented with mild metabolic acidosis and an elevated international normalized ratio (INR) of 1.4 (Table 2), for which vitamin K was administered for 3 days.
On postoperative day (POD) 3, he experienced dyspnea and desaturation. A chest X-ray revealed bilateral pleural effusion, and 600 mL of serous fluid was drained via thoracentesis. Following the drainage, there was an improvement in ventilation, but hemoglobin levels dropped from 7.2 to 4.5 g/dL, and 3 additional units of packed red blood cells were provided.
On POD6, despite adjustments to immunosuppressants, transaminase levels suddenly increased, associated with progressive and loss of liver function tests (aspartate aminotransferase [AST]: 166–2100 IU/L, alanine aminotransferase [ALT]: 212–1820 IU/L). A computed tomography (CT) scan of the abdomen showed hepatic patent vessels. There was also a significant worsening of inflammatory parameters (white blood cells [WBC]: 8200–13 550 WBC/mm3, band cells: 4–10%, C-reactive protein [CRP]: 1.2–4.5 mg/dL) with negative blood and preservation fluid cultures. Antibiotic therapy was switched to empirical piperacillin with tazobactam.
On POD7, renal replacement therapy (RRT) was initiated due to the deterioration of renal function (creatinine: 1–1.7 mg/dL, blood urea nitrogen [BUN]: 31.7–49.9 mg/dL), metabolic acidosis, and hyperkalemia. However, acute liver failure with elevated transaminases, a non-coagulable INR, thrombocytopenia (platelets: 31 000 plt/mm3), hypervolemia, and metabolic acidosis persisted. A seventh-day syndrome hypothesis was proposed, although a liver biopsy was not conducted.
On POD9, the patient experienced decreased consciousness and tonic-clonic seizures, requiring orotracheal intubation and dispensation of phenytoin. A cranial CT scan showed no abnormalities. Plasmapheresis was conducted, and he was listed for retransplantation.
On the same day, a hepatectomy was conducted due to acute liver failure, and a TPCS was performed. Upon readmission to the ICU, thromboelastographic abnormalities were observed, and transfusions of blood products were administered. The patient also required high doses of vasopressors, continuous venovenous hemofiltration dialysis (CVVHD) due to oliguria, correction of persistent metabolic acidosis and hypocalcemia, support with mechanical ventilation, administration of dextrose to prevent hypoglycemia, and maintenance of normothermia with warming blankets. Due to high drainage rates through the Blake drains, refractory shock, and unsuccessful correction of the blood abnormalities, an exploratory laparotomy was necessary to control bleeding from a site on the left abdominal wall.
After 57 h of the anhepatic phase with a TPCS, he underwent reLT from a deceased 57-year-old man with a history of social alcohol consumption and hypertension who died from a hemorrhagic stroke. After reLT, the patient showed a gradual improvement in coagulopathy. His dependence on vasopressors decreased, and mechanical ventilator settings were reduced. CVVHD was maintained, accompanied by regular administration of calcium gluconate, dextrose infusion, and warming blankets.
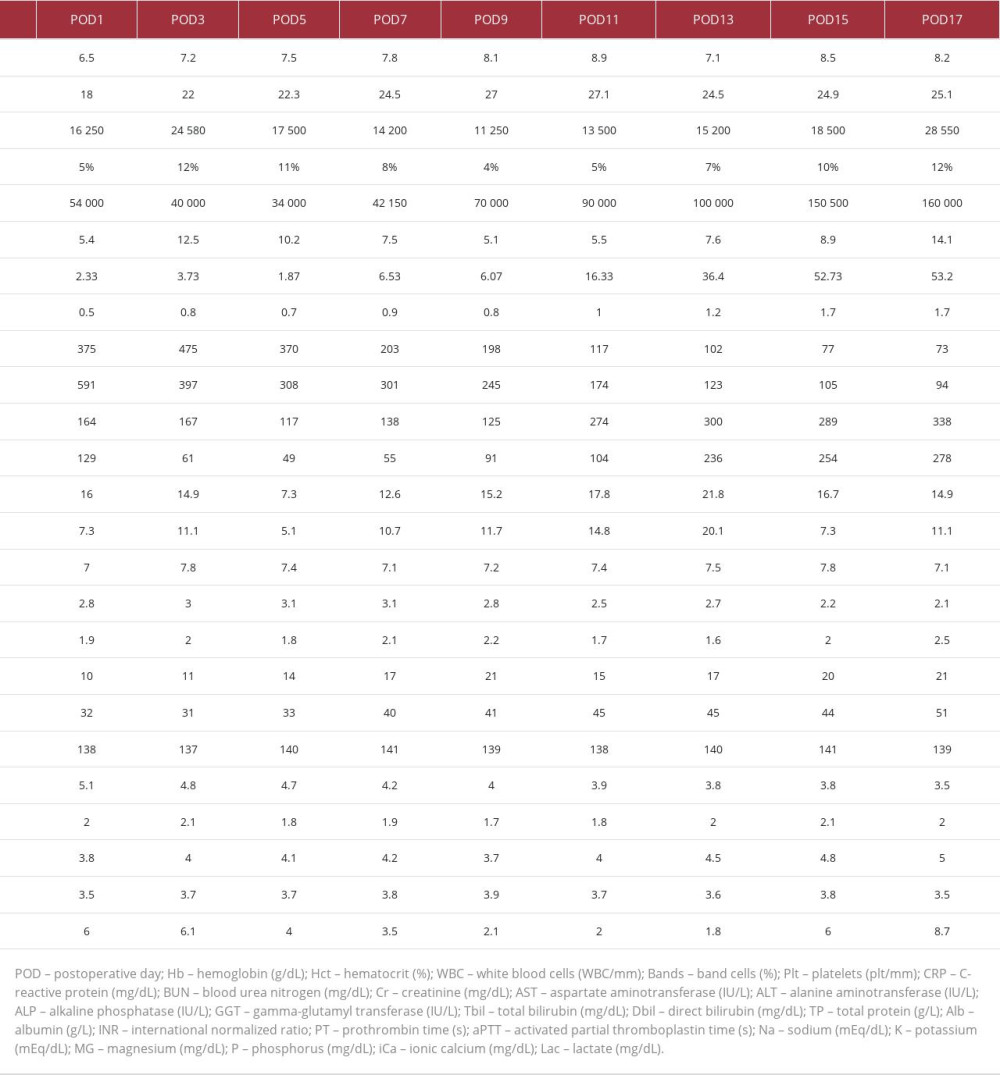
On POD3 after reLT, laboratory test results showed deterioration (WBC: 16 250–24 580 WBC/mm3, band cells: 5–12%, CRP: 5.4–12.5 mg/dL; Table 3), with positive blood cultures for
The patient continued to require RRT and exhibited decreasing transaminase levels but increasing bilirubin levels (AST: 370–102 IU/L, ALT: 308–123 IU/L, total bilirubin: 7.3–21.8 mg/dL, direct bilirubin: 5.1–20.1 mg/dL). There was subsequent clinical and laboratory worsening (WBC: 11 250–15 200 WBC/mm3, band cells: 4–7%, CRP: 5.1–7.6 mg/dL), which prompted the addition of amikacin to the treatment regimen. Following the resolution of thrombocytopenia, a combination of immuno-suppression and ganciclovir was reintroduced, but the patient continued to deteriorate.
Sedation was terminated on POD4 after reLT to perform a neurological assessment, but the patient remained unresponsive. An electroencephalogram (EEG) showed a depressed tracing without an epileptiform pattern. On POD17 after the reLT, his neurological condition did not improve, and there were no trunk reflexes. A cranial CT scan revealed bilateral acute ischemic brain injuries, mainly in the posterior circulation and cerebellar hemispheres, with hemorrhagic transformation, compression of the fourth ventricle, and small subfalcine herniation to the right. Neurosurgical intervention was not feasible, and a protocol for brain death was initiated. The EEG showed cerebral electrical silence, and the patient was declared deceased due to intracerebral hemorrhage.
Discussion
This case report describes the complexities and challenges faced during a prolonged 57-h anhepatic state using a TPCS as a bridge to reLT in a 35-year-old man with autoimmune hepatitis. Prior to the LT, the patient had decompensated cirrhosis with refractory ascites and 2 episodes of upper gastrointestinal bleeding, being categorized with a Child-Turcotte-Pugh score of C and a MELD score of 38 [35]. The procedure was successful, with no complications. However, on POD7, the patient presented with elevated transaminase levels, worsening inflammatory parameters, and deterioration of renal function with the initiation of RRT. These clinical and laboratory findings pointed toward a potential seventh-day syndrome [36], although a liver biopsy was not conducted to confirm the diagnosis.
Seventh-day syndrome is characterized by the sudden, unexpected failure of a normally functioning liver graft 1 week after LT [36]. While the underlying pathophysiology remains unclear, studies show marked apoptosis of hepatocytes, Fas receptor activation, and antibody-mediated rejection as mechanisms leading to the development of the syndrome [37–40]. Treatment options include the immediate start of desensitization, which can be achieved through plasma exchange, intravenous immunoglobulin, or anti-CD20 antibody [40,41].
Our patient presented with acute liver failure 7 days after the surgery without any other explainable etiology, which increases the likelihood of our hypothesis of seventh-day syndrome (as shown in Table 2) [35]. Our approach was to start the desensitization with plasmapheresis and list the patient for reLT. This approach prevents the life-threatening multiorgan failure and intense systemic inflammatory response that the necrotic graft can cause if not immediately removed [42,43]. Indeed, after the initiation of plasmapheresis, the patient had an improvement in hemodynamics and mechanical ventilator settings. However, he still experienced several complications during the 57-h anhepatic state, including hypotension, coagulopathy, metabolic acidosis, renal failure, persistent hypocalcemia, hypoglycemia, and hypothermia.
Our main strategies employed to manage such complications were as follows: (1) vasopressors, predominantly norepinephrine, to sustain a mean arterial blood pressure of 65 mm Hg; (2) administration of 2 packs of fresh frozen plasma every 8 h and 1 vial of vitamin K per day, targeting an INR lower than 2; (3) packed red blood cell units and platelet transfusions, when needed; (4) an exploratory laparotomy was necessary to control severe bleeding from the left abdominal wall; (5) RRT to address hypervolemia and metabolic acidosis; (6) consistent monitoring of serum calcium levels and administration of calcium gluconate to counteract hypocalcemia; (7) continuous dextrose infusion to ensure serum glucose levels remained above 100 mg/dL; (8) warming blankets for normothermia; and (9) regular laboratory tests and intensive monitoring in the ICU. Although unavailable at our facility, the molecular adsorbent recirculating system is another potential approach for patients with acute hepatic failure, which selectively removes albumin-bound toxins from the blood. Recent studies have indicated its effectiveness in anhepatic states [25,29,30].
We consider our case report unique because it was one of the most prolonged periods described in the literature. The anhepatic state has been used in various cases. The most prolonged period without sequelae was 99 h in a 7-month-old female patient [29]. We conducted a literature review of cases of anhepatic states as a bridge to retransplantation, with a total of 29 published articles. Further details of the characteristics of each study can be found in Table 4. In successful cases, the systemic inflammatory response attributed to primary nonfunction seemed to improve during the initial anhepatic state [9–13,21,25–28,32–34].
However, the anhepatic state can be unsuccessful due to several complications. Notably, sepsis emerges as a significant concern. Ringe et al (1993) reported that out of 19 patients undergoing an anhepatic state, 9 died from sepsis [16]. Their subsequent study in 1995 confirmed this concern, with most patients dying from disseminated infections [8]. Similarly, in the study by Domínguez-Fernández et al (2001), half of the patients who underwent transplantation following an anhepatic state died due to sepsis [17]. Sanabria Mateos et al (2016) reported a mean anhepatic state duration of 15.5 h among 6 patients, with all displaying systemic inflammatory response syndrome within the first postoperative week, and the incidence of sepsis was high at 50% [15]. Further reports of sepsis are detailed in Table 4 [7–34]. Despite our patient being on a tailored broad-spectrum antibiotic and antifungal regimen, sepsis was still a clinical challenge, as evidenced by deteriorating laboratory parameters (Table 2).
The absence of liver function in anhepatic states can lead to other complications, such as hypotension, coagulopathy, metabolic acidosis, renal failure, hypocalcemia, hypoglycemia, and hypothermia [6,7,12,14]. While the mechanisms underlying these complications are not fully understood, they may be explained in the context of the liver’s multifaceted roles in physiological homeostasis. For example, the liver’s importance as an immune organ might predispose anhepatic states to sepsis [44–46]. Hypotension is another frequent manifestation, likely due to the accumulation of vasoregulatory substances that the liver typically metabolizes, including nitric oxide and endothelin [47–49]. Coagulation disturbances, notably coagulopathy, are anticipated, given the liver’s central role in clotting pathways [50,51], a challenge underscored in our case and corroborated by others (Table 4). The liver’s involvement in lactate clearance and ammonia-to-urea conversion may elucidate the emergence of metabolic acidosis and renal failure [52,53]. Hemodynamic shifts in the anhepatic state might also contribute to renal tubular injury [54,55]. The frequent administration of citrated blood products in these patients to correct coagulopathy can exacerbate hypocalcemia, amplifying the risk of bleeding [26]. Hypoglycemia is another potential complication, as the liver serves as the primary glycogen storage site [56]. Lastly, anhepatic states tend to present with hypothermia, emphasizing the need for thermal interventions like warming blankets [10,14,22,31].
The anhepatic state can also have long-term complications. In our case, the patient underwent a 57-h prolonged anhepatic state but died 14 days after reLT due to cerebral hemorrhage. Although we managed coagulopathy with specific management strategies, the outcome was unfortunate. In other cases, there have been reported neurological deficits, such as neuropathy and dysarthria [12,18], chronic renal insufficiency [14,23], and infections [19,20,27,29–31]. Further research is needed to better elucidate the mechanisms underlying those long-term complications.
Conclusions
In conclusion, this case highlights one of the most prolonged periods of anhepatic state using a TPCS as a bridge to reLT. We emphasize the complexities and challenges associated with this technique, including sepsis, hypotension, coagulopathy, metabolic acidosis, renal failure, electrolyte disturbances, hypoglycemia, and hypothermia. Vigilant monitoring and intensive care are imperative to manage these complications and improve outcomes. Our patient had cerebral death from a hemorrhagic stroke, and documenting such cases is essential for enhancing our understanding and improving future patient care. Further research is needed to deepen our knowledge of anhepatic states with a TPCS, identify strategies to minimize complications, and refine protocols for LT recipients.
References:
1.. Dababneh Y, Mousa OY, Liver transplantation: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing
2.. Halliday N, Westbrook RH, Liver transplantation: Post-transplant management: Br J Hosp Med Lond Engl 2005, 2017; 78; 278-85
3.. Hartog H, Hann A, Perera MTPR, Primary nonfunction of the liver allograft: Transplantation, 2022; 106; 117-28
4.. Iesari S, Foguenne M, Lerut J, Total hepatectomy and modified temporary porto-caval shunt as a useful bridge to urgent retransplantation: Hepatobiliary Pancreat Dis Int, 2018; 17; 376-77
5.. Nacif LS, Zanini LY, Sartori VF, Intraoperative surgical portosystemic shunt in liver transplantation: Systematic review and meta-analysis: Ann Transplant, 2018; 23; 721-32
6.. Ringe B, Pichlmayr R, Lübbe N, Total hepatectomy as temporary approach to acute hepatic or primary graft failure: Transplant Proc, 1988; 20; 552-57
7.. Ferraz-Neto BH, Moraes-Junior JMA, Hidalgo R, Total hepatectomy and liver transplantation as a two-stage procedure for toxic liver: Case reports: Transplant Proc, 2008; 40; 814-16
8.. Ringe B, Pichlmayr R, Total hepatectomy and liver transplantation: A life-saving procedure in patients with severe hepatic trauma: Br J Surg, 1995; 82; 837-39
9.. Lurz E, Klucker E, Reiter K, One step at a time: A pediatric case of primary two staged liver transplantation in a child with ESLD: Transplantology, 2022; 3; 152-55
10.. Henderson A, Webb I, Lynch S, Total hepatectomy and liver transplantation as a two-stage procedure in fulminant hepatic failure: Med J Aust, 1994; 161; 318-19
11.. Heneghan HM, Nazirawan F, Dorcaratto D, Extreme heatstroke causing fulminant hepatic failure requiring liver transplantation: A case report: Transplant Proc, 2014; 46; 2430-32
12.. Hunter SK, Martin M, Benda JA, Liver transplant after massive spontaneous hepatic rupture in pregnancy complicated by preeclampsia: Obstet Gynecol, 1995; 85; 819-22
13.. Rozga J, Podesta L, LePage E, Control of cerebral oedema by total hepatectomy and extracorporeal liver support in fulminant hepatic failure: Lancet Lond Engl, 1993; 342; 898-99
14.. Lee SH, Yang SH, Kim GS, Two-stage liver transplantation in a surgically complicated liver failure patient after hepatic tumor resection –A case report: Korean J Anesthesiol, 2010; 59; 348-52
15.. Sanabria Mateos R, Hogan NM, Dorcaratto D, Total hepatectomy and liver transplantation as a two-stage procedure for fulminant hepatic failure: A safe procedure in exceptional circumstances: World J Hepatol, 2016; 8; 226-30
16.. Ringe B, Lübbe N, Kuse E, Total hepatectomy and liver transplantation as two-stage procedure: Ann Surg, 1993; 218; 3-9
17.. Domínguez Fernández E, Lange K, Lange R, Relevance of two-stage total hepatectomy and liver transplantation in acute liver failure and severe liver trauma: Transpl Int, 2001; 14; 184-90
18.. Montalti R, Busani S, Masetti M, Two-stage liver transplantation: An effective procedure in urgent conditions: Clin Transplant, 2010; 24; 122-26
19.. Bustamante M, Castroagudín JF, Gonzalez-Quintela A, Intensive care during prolonged anhepatic state after total hepatectomy and porto-caval shunt (two-stage procedure) in surgical complications of liver transplantation: Hepatogastroenterology, 2000; 47; 1343-46
20.. Oldhafer KJ, Bornscheuer A, Frühauf NR, Rescue hepatectomy for initial graft non-function after liver transplantation: Transplantation, 1999; 67; 1024-28
21.. Erhard J, Lange R, Niebel W, Acute liver necrosis in the HELLP syndrome: Successful outcome after orthotopic liver transplantation. A case report: Transpl Int, 1993; 6; 179-81
22.. Detry O, De Roover A, Delwaide J, Prolonged anhepatic state after early liver graft removal: Hepatogastroenterology, 2007; 54; 2109-12
23.. Guirl MJ, Weinstein JS, Goldstein RM, Two-stage total hepatectomy and liver transplantation for acute deterioration of chronic liver disease: A new bridge to transplantation: Liver Transplant, 2004; 10; 564-70
24.. So SK, Barteau JA, Perdrizet GA, Successful retransplantation after a 48-hour anhepatic state: Transplant Proc, 1993; 25; 1962-63
25.. Singh N, Washburn K, Schenk A, Rescue hepatectomy and anhepatic phase management after primary nonfunction in a liver transplant: Exp Clin Transplant, 2022; 20; 776-79
26.. Bertholf RL, Bertholf MF, Brown CM, Ionized calcium buffering in the transfused anhepatic patient: Ab initio calculations of calcium ion concentrations: Ann Clin Lab Sci, 1992; 22; 40-50
27.. Kodakat SK, Ginsburg R, Gopal PB, A case of post-reperfusion syndrome following surgery for liver trauma: Br J Anaesth, 2006; 96; 31-35
28.. Chiumello D, Gatti S, Caspani L, A blunt complex abdominal trauma: Total hepatectomy and liver transplantation: Intensive Care Med, 2002; 28; 89-91
29.. Laine E, Al Sabeah H, Tranäng M, Results of liver retransplantation after rescue hepatectomy: A single-center study: Ann Transplant, 2023; 28; e939557
30.. Cimeno A, Sultan S, Alvarez-Casas J, Transplant hepatectomy with portacaval shunt and MARS therapy for perioperative catastrophe: A series of four liver transplant cases: Transplant Direct, 2021; 7(3); e674
31.. Detry O, Roover AD, Delwaide J, 60 h of anhepatic state without neurologic deficit: Transpl Int, 2006; 19; 769-69
32.. Hammer GB, So SK, Al-Uzri A, Continuous venovenous hemofiltration with dialysis in combination with total hepatectomy and portocaval shunting. Bridge to liver transplantation: Transplantation, 1996; 62; 130-32
33.. Arora H, Thekkekandam J, Tesche L, Long-term survival after 67 hours of anhepatic state due to primary liver allograft nonfunction: Liver Transplant, 2010; 16; 1428-33
34.. Kim HB, Maller E, Redd D, Orthotopic liver transplantation for inflammatory myofibroblastic tumor of the liver hilum: J Pediatr Surg, 1996; 31; 840-42
35.. Tanaka T, Sugawara Y, Kokudo N, Liver transplantation and autoimmune hepatitis: Intractable Rare Dis Res, 2015; 4; 33-38
36.. Hwang S, Lee SG, Ahn CS, Reappraisal of seventh-day syndrome following living donor liver transplantation: Transplant Proc, 2006; 38; 2961-63
37.. Memon MA, Karademir S, Shen J, Seventh Day Syndrome – acute hepatocyte apoptosis associated with a unique syndrome of graft loss following liver transplantation: Liver, 2001; 21; 13-17
38.. Halle-Smith JM, Hall LA, Hann A, Seventh Day Syndrome revisited: Early recognition of the clinical syndrome and an evolving understanding of its etiology: Front Transplant, 2022; 2022; 913584
39.. Pereira M, Ferreira I, Gandara J, Seventh-day syndrome: Case report: Transplant Proc, 2015; 47; 1055-58
40.. Zhongwei Z, Lili C, Bo W, Newly defined clinical features and treatment experience of seventh day syndrome following living donor liver transplantation: Transplant Proc, 2012; 44; 494-99
41.. Matsuura T, Kohashi K, Kawano Y, Successful management to prevent early graft loss due to Seventh-day Syndrome after liver retransplantation: A case report and literature review: Pediatr Transplant, 2021; 25; e13907
42.. Choe W, Kwon S-W, Kim S-S, Effects of therapeutic plasma exchange on early allograft dysfunction after liver transplantation: J Clin Apheresis, 2017; 32; 147-53
43.. Taner CB, Bathala V, Nguyen JH, Primary nonfunction in liver transplantation: A single-center experience: Transplant Proc, 2008; 40; 3566-68
44.. Kubes P, Jenne C, Immune responses in the liver: Annu Rev Immunol, 2018; 36; 247-77
45.. Mikulak J, Bruni E, Oriolo F, Hepatic natural killer cells: Organ-specific sentinels of liver immune homeostasis and physiopathology: Front Immunol, 2019; 10; 946
46.. Yan J, Li S, Li S, The role of the liver in sepsis: Int Rev Immunol, 2014; 33; 498-510
47.. Pascoli MD, Sacerdoti D, Pontisso P, Molecular mechanisms leading to splanchnic vasodilation in liver cirrhosis: J Vasc Res, 2017; 54; 92-100
48.. Arkenau HT, Stichtenoth DO, Frölich JC, Elevated nitric oxide levels in patients with chronic liver disease and cirrhosis correlate with disease stage and parameters of hyperdynamic circulation: Z Gastroenterol, 2002; 40; 907-13
49.. Moore K, Endothelin and vascular function in liver disease: Gut, 2004; 53; 159-61
50.. Intagliata N, Davis J, Caldwell S, Coagulation pathways, hemostasis, and thrombosis in liver failure: Semin Respir Crit Care Med, 2018; 39; 598-608
51.. Hartmann M, Szalai C, Saner FH, Hemostasis in liver transplantation: Pathophysiology, monitoring, and treatment: World J Gastroenterol, 2016; 22; 1541-50
52.. Gladden LB, A lactatic perspective on metabolism: Med Sci Sports Exerc, 2008; 40; 477-85
53.. Barmore W, Azad F, Stone WL, Physiology, urea cycle: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing [cited 2023 Oct 29].
54.. Caragata R, Emerson S, Santema ML, Intraoperative hypotension and the risk of acute kidney injury following liver transplantation: Clin Transplant, 2023; 37; e15053
55.. Basile DP, Anderson MD, Sutton TA, Pathophysiology of acute kidney injury: Compr Physiol, 2012; 2; 1303-53
56.. Soon GST, Torbenson M, The liver and glycogen: In sickness and in health: Int J Mol Sci, 2023; 24; 6133
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250