19 February 2024: Articles 
A 56-Year-Old Woman Presenting 19 Years After Pubic Bone Fracture with a Surgical Screw Foreign Body in the Bladder
Challenging differential diagnosis, Unusual or unexpected effect of treatment, Rare disease, Educational Purpose (only if useful for a systematic review or synthesis)
Michael N. ChrysikosDOI: 10.12659/AJCR.942059
Am J Case Rep 2024; 25:e942059
Abstract
BACKGROUND: Non-calculus foreign bodies in the bladder are rare and are usually introduced via the urethra. Reports of the migration of metallic foreign bodies from previous surgery are uncommon and mainly associated with surgical screws used for the internal fixation of pubic bone fracture and total hip replacement. This report is of a 56-year-old woman presenting with a surgical screw foreign body in the bladder 19 years after open surgical reduction and internal plate and screw fixation of traumatic fracture of the pubic bone.
CASE REPORT: A 56-year-old woman visited a urologist because of gross hematuria. She mentioned a mild pelvic pain and multiple lower urinary tract infections over the past 2 years, with no other symptoms. From the previous history, she had undergone an open reduction and internal fixation of the pelvic ring, with surgical plates and screws following pubic bone’s fracture, due to an accident 19 years earlier. Cystoscopy identified the presence of a screw head protruding into the bladder wall. The screw was extracted via open surgery, and the patient was discharged 2 days later.
CONCLUSIONS: While intravesical foreign bodies are rarely seen in Emergency Departments, clinicians should maintain a level of suspicion in certain cases. The purpose of this case report is to present the unlikely and delayed complication of internal pubic bone fixation resulting in the migration of a fixation screw to the bladder. It also highlights the importance of imaging in diagnosis and localization of the foreign body in the bladder.
Keywords: urinary bladder, Foreign-Body Migration, Bone Screws, Postoperative Complications
Background
A broad selection of foreign bodies has been removed from the bladder, most of which were inserted via the urethra during non-iatrogenic acts [1]. However, there have been cases of tips of JJ ureteric fragments or Foley balloon catheters being removed incompletely and iatrogenic materials (gauze, swab, sutures, tape for stress incontinence, ceramic sheath of resectoscope, prong of endoscopic removal forceps, and bone cement) that remained in the bladder causing symptoms of mainly gross hematuria, recurrent infections of the lower urinary tract, and pelvic pain [2]. An individual’s medical history could reveal important information that would lead the doctor to conduct a more comprehensive assessment of the possible presence of an intravesical foreign body and proceed to imaging to detect it [1,2]. This report is of a 56-year-old woman presenting with a surgical screw foreign body in the bladder 19 years after open surgical reduction and internal plate and screw fixation of a traumatic fracture of the pubic bone.
Case Report
A 56-year-old female patient with no health risks, such as tobacco smoking, alcohol, or substance abuse, was admitted to our hospital because of a gross hematuria incident and multiple infections of the lower urinary tract over the past 2 years. Previous anamnesis showed a superior and inferior pubic rami bilateral fracture and symphyseal diastasis followed by open reduction and internal fixation (ORIF) with plates and screws 19 years ago. She also mentioned a total left hip replacement a few months prior and a medication of non-vitamin K antagonist oral anticoagulant due to thrombophilia.
On admission, she was afebrile, her vital signs were within the normal values, and the clinical examination revealed a mild pain in the lower abdomen. From the laboratory test results, pyuria and a few red blood cells in the general urine test were the only remarkable points. The past X-ray image of the kidney, ureters, and bladder showed the surgical plates and screws of the pubic bone and a left hip prosthesis, which was consistent with the information of the medical history (Figure 1). The current image revealed that a screw of the right pubic bone’s plate was loose, and then the suspicion of a possible correlation between the screw and the symptoms was formed (Figure 2A). The next step was a cystoscopy, which identified the presence of a screw head protruding from the posterior wall into the bladder (Figure 2B).
The patient underwent an open surgery procedure, and the screw head was detected after a cystotomy (Figure 3). The screw was dislodged applying a medical screwdriver and the bladder was reconstructed with sutures (Figure 4). A new X-ray showed the absence of the previously loose screw from the pubic bone surgical cement (Figure 5). She was discharged 2 days after the operation with a 16-Fr Foley catheter, which was removed 7 days later. She reported severe pelvic discomfort during urination and fever 10 days after the catheter removal, but these were successfully resolved with antibiotic administration. Two months following the surgical procedure, the patient had fully recovered and restored her daily routine.
Discussion
An intravesical foreign body is an infrequent yet significant urological diagnosis in the emergency department. According to the largest population-based study investigating the epidemiology of genitourinary foreign bodies (GUFB) by Rodriguez et al, of 102 333 patients with GUFB who visited the emergency department in the United States over 5 years, only 7151 (6.98%) visits were associated with urethra/bladder foreign bodies (less than 1 visit per 100 000 persons), and many of the patients had a mental health disease background (38.7% of the urethral/bladder foreign bodies cases) [3]. A different study by Nelson et al reports that GUFBs result in 375 inpatient admissions yearly across the United States, costing payers an estimated $2.61 million [4]. In this case report, we present a rare late complication of surgical screw migration to the bladder and the imaging control and open surgery to remove it. The extensive time lapse between the last surgical procedure and the migration prompted us to conduct a more thorough investigation into the cause of the screw loosening and devise a means of preventing it.
A foreign body can exist in the bladder via self-insertion through the urethra for autoerotic stimulation, relief from pain, and abortion attempts, or via iatrogenic actions or migration from adjacent organs [5]. Many objects have been reported as GUFBs, and many articles summarize several case reports from the literature, including the report from Van Ophoven and de Kernion [6]. The predominant symptoms are hematuria, dysuria, frequent urination, urge incontinence, pelvic pain, and recurrent low urinary tract infections. In the absence of explicit evidence about the presence of a foreign object within the urinary tract, the suspicion should be formed from the symptoms, anxiety when discussing sexual history, attempts to avoid genital/rectal history, and previous bladder or adjacent organs surgery. The foreign body could be detected with kidney-ureter-bladder radiography (for radio-opaque objects), ultrasonography, and computed tomography, but the confirmation and subsequent removal are accomplished via cystos-copy. Most intravesical foreign bodies can be removed during cystoscopy using grasping forceps, but in cases in which endoscopic management is impossible, cystolithotomy or open surgery is recommended [6]. The removal process relies mostly on the foreign body type, the patient’s condition, and the staff’s experience [7].
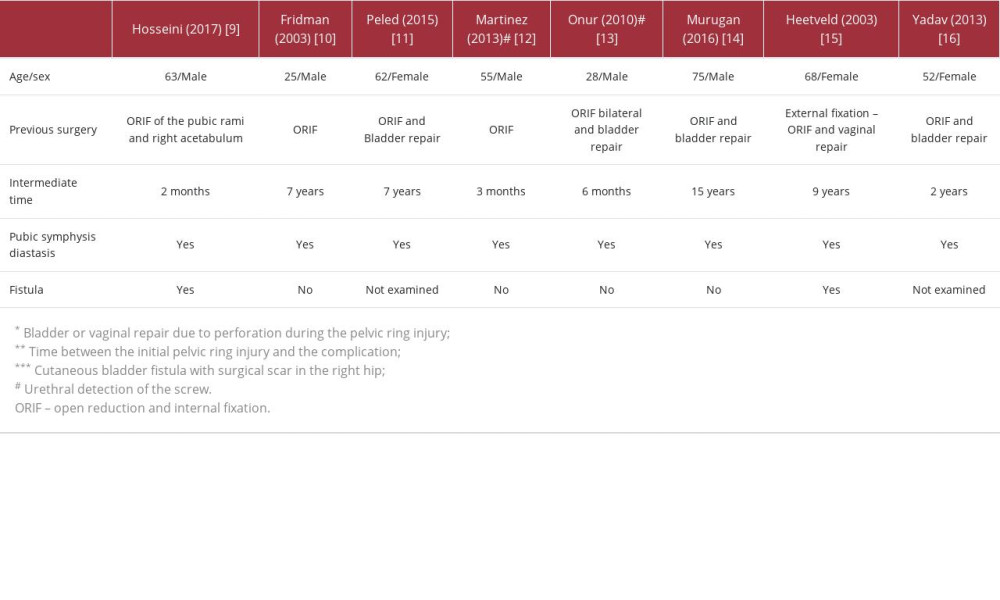
In our case, the foreign body was a screw that migrated from the pubic bone plate and protruded into the bladder wall. According to the Clavien-Dindo classification, this is a grade 3b surgical complication [8]. At the time of the ORIF, our patient had no bladder perforation but pubic symphysis diastasis. This is possibly the key reason for the screw loosening over the years, causing the bladder wall to protrude and, consequently, the patient’s symptoms. There are a few case reports in the literature that present a screw migrating from the pubic ring to the bladder or urethra [9–16]; however, this is the first case with such a long period between the initial pelvic injury and the complication, at 19 years (Table 1). The most remarkable point is the pubic diastasis, which is presented in all the reported cases, including this one. Some researchers point out that this is a significant risk factor for the screw loosening because of the instability of the plates’ placement, and thus, they suggest a follow-up with radiography surveillance, even in asymptomatic patients [10]. Peled et al add to the risk factors the osteoporosis and a fixed implant that crosses a joint or applies in a non-rigid fashion, allowing micro-motions. Therefore, they highlighted the importance of the symphyseal plate positioning, especially superiorly adjacent to the Retzius space, to avoid such complications [11]. Murugan and Ramalingam presented a similar case, with previously failed attempts to remove the plate, which may be an extra risk factor for the screw loosening [14]. Furthermore, Heetveld et al examined the role of the fistula in their case and concluded that the screw loosening and migrating caused the bladder fistula and not the opposite [15].
Another aspect of these cases is the initial perforation of the bladder due to the pelvic fracture. Bjurlin et al collected cases of genitourinary injuries due to pelvic fractures using the National Trauma Bank and reported that from 31 380 patients with pelvic fractures, only 4.6% had a genitourinary injury, and 3.39% were associated with bladder injury alone [17]. Despite the rareness of the incident, an undetected bladder perforation with ORIF due to pelvic injury could be crucial to a patient’s future quality of life. For this reason, Yadav et al recommended the need for an initial approach for a pelvic injury by the trauma surgeon, urologist, and gynecologist examining the adjacent organs’ security [16]. In the case of a concurrent bladder injury, external fixation of the pelvic fracture may be a better solution for the patient, because the clinician has to manage the bladder injury [18]. Plate removal has also been shown to reduce possible complications, and, as it seems, routine removal of the plates is not essential, with this decision needing to be individualized in cases of a potential pregnancy, residual symptoms after the surgery, impact failure, and infection [19].
Conclusions
Screw migration from a pelvic bone plate to the lower urinary system is an uncommon and late-onset surgical complication that can necessitate further surgery. This report has presented an uncommon and late complication of internal pubic bone fixation resulting in the migration of a surgical screw to the bladder. Several case reports document a comparable scenario, which exhibits 2 fundamental features: pubic diastasis and, consequently, the instability of the plates’ floor. Imaging plays a crucial role not only in diagnosing and locating foreign bodies in the bladder, but also in preventing the migration, through monitoring the screw loosening. The occurrence of repeated urinary infections following pelvic fixation should serve as a cautionary sign for the physician. In such cases, it is advisable for the doctor to recommend a cystography or cystoscopy to the patient and consider the possibility of a correlation between the symptoms and the prior pelvic surgery. In addition, detecting the concurrent adjacent organs’ damage is vital for treatment; therefore, pelvic injuries in the emergency department must be examined by trauma surgeons, urologists, and gynecologists simultaneously.
Figures
References:
1.. Kochakarn W, Pummanagura W, Foreign bodies in the female urinary bladder: 20-year experience in Ramathibodi Hospital: Asian J Surg, 2008; 31(3); 130-33
2.. Bansal A, Yadav P, Kumar M, Foreign bodies in the urinary bladder and their management: A single-centre experience from North India: Int Neurourol J, 2016; 20(3); 260-69
3.. Rodríguez D, Thirumavalavan N, Pan S, Epidemiology of genitourinary foreign bodies in the United States emergency room setting and its association with mental health disorders: Int J Impot Res, 2020; 32(4); 426-33
4.. Nelson M, Koehne E, Dornbier R, Genitourinary foreign body in United States: Incidence, patient characteristics, treatments and economic burden: Urol Pract, 2019; 6(6); 345-49
5.. Moon SJ, Kim DH, Chung JH, Unusual foreign bodies in the urinary bladder and urethra due to autoerotism: Int Neurourol J, 2010; 14(3); 186-89
6.. Van Ophoven A, deKernion JB, Clinical management of foreign bodies of the genitourinary tract: J Urol, 2000; 164(2); 274-87
7.. Rafique M, Intravesical foreign bodies: Review and current management strategies: Urol J, 2008; 5(4); 223-31
8.. Dindo D, Demartines N, Clavien PA, Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey: Ann Surg, 2004; 240(2); 205-13
9.. Hosseini SR, Rezaei H, Mohseni MG, Screw as a bladder foreign body: Urol Case Rep, 2017; 11; 69-70
10.. Fridman M, Glass AM, Noronha JA, Spontaneous urinary voiding of a metallic implant after operative fixation of the pubic symphysis: A case report: J Bone Joint Surg Am, 2003; 85(6); 1129-32
11.. Peled E, Norman D, Kakiashvili D, Henley MB, Recurrent episodes of micturition with expulsion of symphyseal plate screws following pelvic ring fixation: Case report: BMC Musculoskelet Disord, 2015; 16; 127
12.. Martinez LM, Kierl K, Slobodov G, Urethral injury by an orthopedic screw: An unusual cause of hematuria: Urology, 2013; 81(4); e25-26
13.. Onur R, Yilmaz E, Onur MR, Orhan I, Urethral erosion of a bone screw after internal urethrotomy: A rare complication after pelvic trauma: Ir J Med Sci, 2010; 179(3); 443-45
14.. Murugan P, Ramalingam M, Endoscopic management of free lying migratory orthopedic screw in bladder: Urol Case Rep, 2016; 8; 47-48
15.. Heetveld MJ, Poolman RW, Heldeweg EA, Ultee JM, Spontaneous expulsion of a screw during urination: An unusual complication 9 years after internal fixation of pubic symphysis diastasis: Urology, 2003; 61(3); 645
16.. Yadav S, Arora NC, Prasad M, Varma R, Spontaneous urinary voiding of metallic screws in a patient with symphyseal plating for type II pelvic ring disruption: Chin J Traumatol, 2013; 16(4); 230-32
17.. Bjurlin MA, Fantus RJ, Mellett MM, Goble SM, Genitourinary injuries in pelvic fracture morbidity and mortality using the National Trauma Data Bank: J Trauma, 2009; 67(5); 1033-39
18.. Giannoudis PV, Pape HC, Damage control orthopaedics in unstable pelvic ring injuries: Injury, 2004; 35(7); 671-77
19.. Giannoudis PV, Chalidis BE, Roberts CS, Internal fixation of traumatic diastasis of pubic symphysis: Is plate removal essential?: Arch Orthop Trauma Surg, 2008; 128(3); 325-31
Figures
In Press
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250