13 February 2024: Articles 
Robotic-Assisted Resection of a Benign Schwannoma of the Obturator Nerve: A Rare Case
Mistake in diagnosis, Unusual setting of medical care, Rare disease
Bruno Mirandola BulisaniDOI: 10.12659/AJCR.942083
Am J Case Rep 2024; 25:e942083
Abstract
BACKGROUND: Neurilemmomas are rare tumors derived from the Schwann cells that comprise the peripheral nerve sheaths. They have a slow growth and rarely display malignancy. Early diagnosis is rare, and the treatment consists by surgical resection. Although robotic-assisted surgery is commonly used for treating retroperitoneal diseases, there are few reports of resection of retroperitoneal and pelvic schwannoma through robotic-assisted surgery. In the present study, we reported a case of complete excision of a benign retroperitoneal schwannoma of the obturator nerve by robotic-assisted surgery.
CASE REPORT: A 51-year-old woman was referred by her gynecologist for left pelvic discomfort of a 3-month duration. The physical examination was normal, but a computerized tomography scan of the abdomen and pelvis showed an expansive pelvic lesion in the topography of the left iliac vessels, a hypodense contrast enhancement measuring 4.6×3.4 cm. Magnetic resonance imaging showed an extraperitoneal lesion located medially and inferiorly to the left external iliac vessels, with a size of 4.9×3.7 cm, and of probable neural etiology. Surgical resection of the tumor was recommended because of the diagnostic hypothesis of obturator nerve schwannoma.
CONCLUSIONS: This case showed that retroperitoneal neurilemmomas are difficult to diagnose owing to a lack of specific symptoms, and the best treatment is complete tumor resection. The use of robotic techniques gives greater dexterity to the surgeon, since it provides high-definition 3-dimensional vision, which can make the removal of retroperitoneal tumors susceptible to minimally invasive resection in a safe and effective way.
Keywords: Minimally Invasive Surgical Procedures, Neurilemmoma, Obturator Nerve, Retroperitoneal Neoplasms, Robotic Surgical Procedures
Background
Schwannomas or neurilemmomas are rare tumors derived from the Schwann cells that comprise the peripheral nerve sheaths. Schwannomas are frequently found on the head, neck, and extremities. Retroperitoneal incidence is rare and occurs in 0.5% to 5% of all schwannoma cases. These tumors can affect patients of all ages but are most present between the third and sixth decade of life [1]. Schwannomas are benign with slow growth and rarely display malignancy [2]. Early diagnosis is rare, and many cases are accidentally diagnosed during imaging tests or routine physical examinations, owing to asymptomatic or nonspecific symptoms [3,4]. Only a histo-pathological study confers the definitive diagnosis of schwannomas [5]. Treatment is done by surgical resection of the tumor, as these tumors are less sensitive to radiation and/or chemotherapy [4]. Schwannomas present a favorable prognosis when completely resected [6]. Although robotic-assisted surgery is commonly used for treating retroperitoneal diseases, there are few reports of resection of retroperitoneal and pelvic schwannoma through robotic-assisted surgery. The use of robotic-assisted surgery has a precise indication for lesions located in anatomical regions of difficult access, since it is necessary to have greater dexterity for dissection in these regions, especially when close to the vital structures [7]. Robotic surgery allows for faster postoperative recovery of the patient, compared with laparotomy and video laparoscopic surgery [6].
In the present study, we report a case of complete excision of benign retroperitoneal schwannoma of the obturator nerve by robotic-assisted surgery.
Case Report
TECHNIQUE:
The patient was placed in a horizontal supine position and the surgery was performed under general anesthesia. We chose to use a double J catheter passage in the left ureter and delay bladder probing. Pneumoperitoneum was done with a Palmer puncture and CO2 pressure of 14 mmHg. Then, a 12-mm trocar was introduced into the abdominal cavity for the camera. Three portals were inserted into the robot arms: arm 1 in the right iliac fossa to hook; arm 2 in the upper left quadrant for bipolar fenestration forceps; and arm 3 in the left iliac fossa for the Cadiere forceps; a 5-mm trocar was placed in the upper right quadrant (A) for the vacuum cleaner or auxiliary clamp. The table was slightly tilted to the right, with a Trendelenburg incline of 15 degrees.
During the cavity inventory, a mass was located between the uterus and the iliac vessels in the left retroperitoneal space, medially and inferiorly to the external iliac vessels. The tumor was dissected from adjacent structures after opening the retroperitoneum, preserving the capsule and neural fascicles. During the dissection, a pedicled tumor was found on the left obturator nerve. It was decided to ligate the neural pedicle with clips of polymer ligation (Weck®) with locking (Hem-o-Lok®; Teleflex Incorporated, Wayne, PA, USA) for hemostasis (Figure 2). The piece was removed through a Pfannenstiel incision.
The surgical time was 85 min. There were no complications, and the blood loss was 10 mL. The patient recovered without complications during the postoperative period and was released from fasting immediately after the surgery. The discharge occurred during the first postoperative period, and the removal of double J catheter occurred during the 15th postoperative period. In the ambulatory follow-up, the patient reported shooting pains in the inner side of the left thigh that lasted a week, followed by progressive improvement. Electromyography of the patient’s lower limbs was conducted, and there were no changes or impairment of motor or sensitive roots found during the test.
Regarding the robotic platform used for resection, care was taken so that the resection could occur in the best way and avoid possible postoperative complications. To avoid injury to the left ureter, the medical team performed the passage of a double J catheter before the procedure. Then, for the dissection of the lesion, anatomical planes were used, especially the common iliac vessels, as a reference point to be able to perform the dissection with greater security of the nerves and iliac vessels. Once the structures were identified, it was possible to dissect the lesion with greater caution and safety to preserve the adjacent structures.
The result of the macroscopic histopathological examination confirmed the presence of an encapsulated retroperitoneal neoplasia of 6.8×5.2×2.9 cm with a fusocellular pattern, no identification of necrosis or mitotic areas, and free margins (Figure 3). In addition, microscopic histopathological examination revealed areas of cystification, with cells tending toward the epithelioid at the edge, containing hyaline material in the cystic spaces. This coating, tending toward the epithelioid, showed a single layer of flattened cells or was oligoestratified, with polarity maintained around light. The margin of resection was free and included with the tumor capsule. Schwannoma diagnosis was determined by the presence of a strong and diffuse positive S100 protein antigen and Ki-67 antigen (MIB-1), with a proliferative index estimated at 3%, as demonstrated by immunohistochemical examination (Figure 4).
Discussion
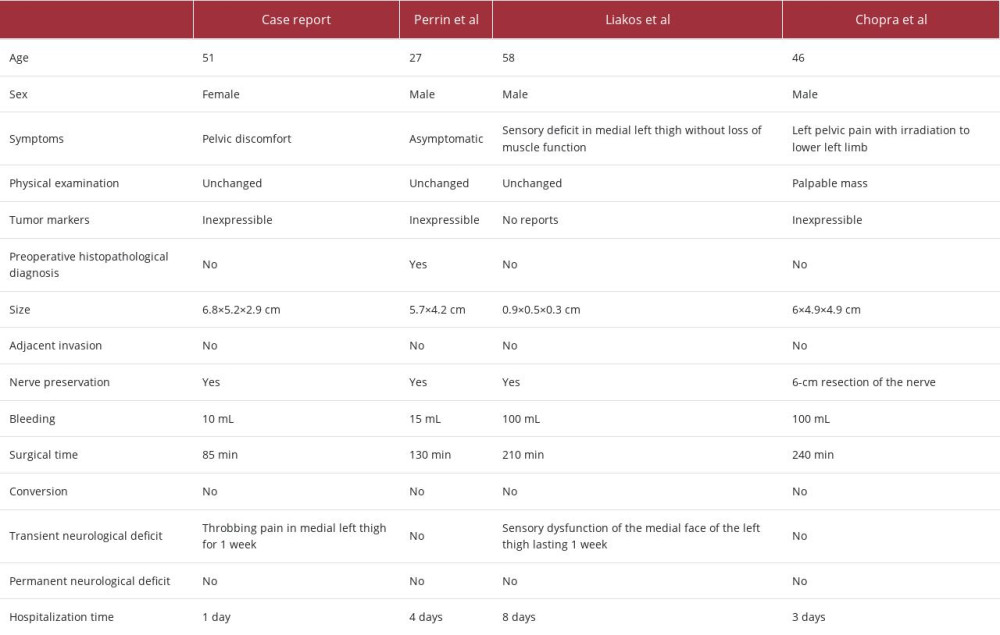
The first case of the use of robotic-assisted surgery for the treatment of benign obturator nerve schwannomas was reported in 2016 [8]. In the literature, only 3 articles in the PubMed database report robotic-assisted surgery for schwannoma resection [8–10]. In these cases, robotic-assisted surgery was useful to preserve the function of nerves from which a schwannoma arises, and there was neural injury in only 1 case. In this case, it was identified that the obturator nerve was encompassed by the tumor and, thus, there was the resection of 5 to 6 cm of the obturator nerve [9]. Postoperative permanent neurological complications were not reported in any of the cases, and even though the patient with neural injury had a complete section, they recovered without any deficits in activities of daily life [9]. Preoperative symptoms were overcome in symptomatic patients. The average surgical time was 193 min, the average hospitalization time was 5 days, and the maximum blood loss was 100 mL. All surgeries were completed successfully, without any changes to surgery or conversion to laparotomy or laparoscopy, and there was no postoperative mortality.
Schwannomas are typically benign tumors of slow growth and late diagnosis. However, they can undergo malignant transformation when associated with Von Recklinghausen disease (type II neurofibromatosis) or when an epithelioid morphology of peripheral nerve sheath tumor is present [4,11]. They are usually large at the time of diagnosis, because they are asymptomatic or have vague symptoms, such as abdominal pain [3,4], and rarely neurological manifestations, such as limb pain, paresthesia, and motor weakness due to the compression of adjacent structures [12].
The obturator nerve comes from the ventral branch of the second, third, and fourth lumbar nerves [12]. It supplies the external obturator muscle, adductor thigh muscle, and hip and knee joints and is responsible for the sensory innervation of the medial thigh [13]. Injury of the obturator nerve can result in permanent neuropathy, which causes loss of force of the adductors of the thigh and loss of sensitivity in the medial part of the thigh [9].
Preoperative diagnosis of schwannomas is difficult and can be done through noninvasive methods, such as CT, MRI, and ultrasound. Imaging tests can detect a solid mass lesion that is well defined [14]. MRI usually shows low to intermediate signal intensity in T1-weighted images and high signal intensity in T2-weighted images [15], but these changes are not specific [16]. Although schwannomas are rare, these tumors should be considered in the differential diagnosis of pelvic tumors [17]. Image-guided biopsy provides a histopathological diagnosis, owing to the challenging preoperative diagnosis of retroperitoneal schwannomas. Imaging can aid in determining the tumor’s size, margin, vascularity, and involvement with adjacent organs, but its findings are not precise enough to make a diagnosis. There are no definitive non-histological diagnostic methods; however, cross-sectional radiology and core needle biopsy can distinguish the tumors from other malignant or invasive conditions [3].
Complete excision is the preferred treatment for schwannomas, which are usually single nodules, solid and encapsulated, and can be resected without capsule rupture [2,7]. It is important to make every effort to preserve the integrity of the nerve, even if it is not always possible [18]. In case of obturator nerve injury during surgical excision, a neurosurgical evaluation is recommended, because a surgical repair with return of nervous function is possible [9]. Benign schwannoma surgery has a good prognosis for patients; however, long-term follow-up is necessary because the recurrence rate is 20% [6,8,19]. However, since once the robotic platform provides precise maneuverability and improved dexterity with wristed instruments, the benign schwannoma can be completely removed, reducing the risks of recurrence. Therefore, if this possibility is available in the medical center, it is a preferred technique, since it reduces the complications of resectioning benign retroperitoneal schwannomas. Schwannomas can be either sessile or pedunculated. The resection area for sessile tumors is more complicated because the base is the biggest region of the lesion, requiring a larger resection area, but as the base narrows in the pedunculated form, the resection area will be smaller.
The greatest challenges in the minimally invasive resection of retroperitoneal tumors are the restricted work area, the proximity of large vessels, and the proximity to the ureter [7]. Robotic-assisted surgery allows some advantages over laparoscopic surgery, such as the 3-dimensional visualization of the tumor, instruments endowed with 7 degrees of freedom (compared with 5 degrees of freedom in laparoscopic surgery), dimensioning of movement, and filtering of tremors and ergo-nomic comfort for the surgeon, which lead to a more accurate procedure. These benefits help surgeons conduct minimally invasive surgeries, even for large retroperitoneal tumors of difficult resection by conventional laparoscopy [7]. However, the limitations of robotic surgery involve a learning curve for the surgeon, low availability of this technique in hospitals, and the added cost of the procedure. On the other hand, the use of the robotic technique is compensated, at least in part, by the lower number of blood transfusions, shorter average hospitalization time, and patients’ earlier return to usual activities [7].
Schwannoma resection of the obturator nerve using robotic-assisted surgery has been reported in only 3 cases to date [8]. In the present case, the patient had nonspecific symptoms, and the tumor was found incidentally by imaging tests. The surgery was laborious due to the location and proximity of the external and internal iliac vessels. Robotic-assisted surgery allowed complete resection of the retroperitoneal schwannoma, since the tumor mass was well circumscribed and did not present invasion of adjacent tissues, despite its intimate contact with these structures. Thus, the high-definition 3-dimensional vision provided by the robotics platform contributed to the precise dissection of the tumor and its safe removal [7].
In summary, the main advantages of the surgical technique and use of the robotic platform in our article are not restricted to the surgeon’s greater ability to manipulate tissue, but include the reduced chance of injuring adjacent tissues. In addition, as the robotic platform offers the possibility of precise maneuverability and increased dexterity with wrist instruments, the retroperitoneal schwannoma can be completely removed, reducing the risks of further adjacent tissue injuries. If this option is available in a medical center, it is a preferred technique that reduces the complications of resection of retroperitoneal schwannomas. The biodemographic, morphological and surgical data of patients with obturator nerve schwannoma operated by robotic-assisted surgery was summarized on Table 1.
Conclusions
Retroperitoneal schwannomas are rare and difficult to diagnose preoperatively, owing to the lack of specific symptoms. Complete tumor resection is the indicated treatment, as it also provides a definitive diagnosis of the lesion. The use of robotic techniques gives greater dexterity to the surgeon, making the removal of retroperitoneal tumors in a minimally invasive resection safe and effective, resulting in shorter hospitalization time and faster return to daily activities.
Figures
References:
1.. Patocskai EJ, Tabatabaian M, Thomas MJ, Cellular schwannoma: A rare presacral tumour: Can J Surg, 2002; 45(2); 141-44
2.. Yi K, Wang YM, Chen J, Laparoscopic resection of an obturator schwannoma: A case report: Chin Med J (Engl), 2010; 123(13); 1804-6
3.. Nepal P, Mataki Y, Maemura K, Retroperitoneal schwannoma sandwiched between abdominal aorta and inferior vena cava. A case report: Int J Surg Case Rep, 2020; 73; 112-15
4.. Ribeiro MA, Elias YG, Augusto SS, Laparoscopic resection of primary retroperitoneal schwannoma: A case report: World J Clin Cases, 2020; 8(18); 4114-21
5.. Nah YW, Suh JH, Choi DH, Benign retroperitoneal schwannoma: Surgical consideration: Hepatogastroenterology, 2005; 52(66); 1681-84
6.. Melvin WS, Laparoscopic resection of a pelvic schwannoma: Surg Laparosc Endosc, 1996; 6(6); 489-91
7.. Bindal V, Bhatia P, Kalhan S, Robot-assisted excision of a large retroperitoneal schwannoma: JSLS, 2014; 18(1); 150-54
8.. Das Gupta TK, Brasfield RD, Solitary malignant schwannoma: Ann Surg, 1970; 171(3); 419-28
9.. Chopra S, Dharmaraja A, Satkunasivam R, Gill IS, Robot-assisted laparoscopic resection of a pelvic schwannoma: Urol Case Rep, 2017; 11; 63-65
10.. Liakos N, Mendrek MA, Witt JH, Wagner C, Robot-assisted nerve-sparing excision of a symptomatic obturator nerve schwannoma: A case report: Cureus, 2020; 12(11); e11468
11.. Marchevsky AM, Balzer B, Mediastinal tumors of peripheral nerve origin (so-called neurogenic tumors): Mediastinum, 2020; 4; 32
12.. Sumalatha S, Appala N, Shetty A, Serendipitous discovery of a benign obturator nerve schwannoma: Case report with a brief clinical review: Sultan Qaboos Univ Med J, 2021; 21(3); 477-80
13.. Scotto V, Rosica G, Valeri B, Benign schwannoma of the obturator nerve: A case report: Am J Obstet Gynecol, 1998; 179(3 Pt 1); 816-17
14.. Di Furia M, Salvatorelli A, Della Penna A, Advantage of laparoscopic resection for pelvic schwannoma: Case report and review of the literature: Int J Surg Case Rep, 2018; 45; 38-41
15.. Nishikimi T, Yoshino Y, Yamada H, Two cases of pelvic schwannomas simultaneously resected with the prostate by robot-assisted surgery: IJU Case Rep, 2021; 4(5); 277-81
16.. Perrin H, Brunner P, Ortega JC, Robotic resection of an obturator schwannoma with preservation of normal nerve fascicles and function: J Robot Surg, 2017; 11(4); 479-83
17.. Gleason T, Le BH, Parthasarathy K, Robinson-Bennett B, Obturator nerve schwannoma as a mimic of ovarian malignancy: Case Rep Obstet Gynecol, 2017; 2017; 9724827
18.. Aubert J, Debiais F, Levillain P, [Schwannoma of the obturator nerve with urologic manifestations: Report of a case.]: Ann Urol (Paris), 2000; 34(1); 58-65 [in French]
19.. Park NY, Chong GO, Lee YS, Laparoscopic resection of schwannoma in the anomaly of obturator nerve: J Laparoendosc Adv Surg Tech A, 2007; 17(6); 769-73
Figures
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250