19 December 2023: Articles 
Does That Go There? A Rare Occurrence of Spontaneous Sternocleidomastoid Abscess without Trauma in a Diabetic Individual
Rare coexistence of disease or pathology
Sebastian S. Casillas-BerumenDOI: 10.12659/AJCR.942265
Am J Case Rep 2023; 24:e942265
Abstract
BACKGROUND: Spontaneous abscesses are generally typical in patients with significant risk factors and have been linked to numerous muscle groups. The sternocleidomastoid muscle, however, piqued our interest as an unusual location, especially in this patient who, other than diabetes mellitus, had no associated risk factors or signs of trauma.
CASE REPORT: A 61-year-old man appeared with neck pain, erythema, and swelling that had been present for 9 days and for which he had previously been examined in the Emergency Department. He was discharged on oral doxycycline after initial computed tomography (CT) of the neck revealed infiltration without collection. He returned with worsening symptoms and new-onset fever and chills. Vital signs were normal on assessment, with no evidence of trauma. Swelling was observed near the right sternocleidomastoid muscle insertion. A repeat CT scan of the neck revealed an abscess 2.5 cm in diameter. He was originally treated with empiric antibiotics before being moved to targeted medications. Incision and drainage were completed without complication. The patient was given a 6-week course of oral antibiotics.
CONCLUSIONS: Spontaneous intramuscular abscesses are uncommon in people who have had no previous trauma or other known risk factors, but could be encountered in diabetic patients with non-optimal blood glucose levels, due to bacteremia. As a result, these cases require a high level of suspicion to be recognized and treated early. The scarcity of literature on this illness makes determining the cause challenging. However, by highlighting this case, we intend to raise awareness and facilitate early diagnosis and treatment.
Keywords: Abscess, Neck Muscles, Neck Pain, Pyomyositis, Subcutaneous Tissue
Background
Spontaneous abscesses involving the sternocleidomastoid muscle are infrequently observed in the clinical setting; however, other locations, such as the subscapularis muscle or biceps muscle, have been reported, which gives us a notion of the spontaneity of the presentation of this clinical entity [1–3]. The presence of abscess has been correlated with risk factors such as patients’ immunocompromised status, trauma, intravenous drug use, and even malnutrition. Poorly controlled type 2 diabetes mellitus is another risk factor, which seems to be the common variable in some cases [1,4]. In the present case, we discuss an individual with type 2 diabetes mellitus presenting with a spontaneous abscess of the sternocleidomastoid muscle.
Case Report
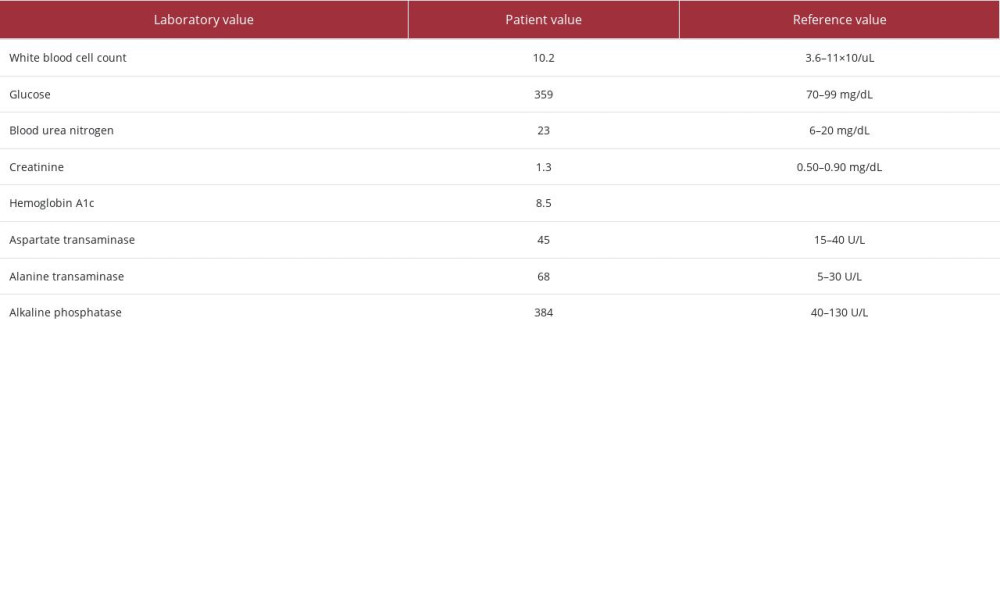
A 61-year-old male patient with a past medical history of diabetes mellitus presented to the Emergency Department (ED) with chest pain of a week’s progression, which according to the patient began after he helped his brother move. The patient mentioned that he was carrying and pushing boxes when he felt tension in his neck and right shoulder. For this reason, the patient presented to the ED, and after a negative computed tomography (CT) scan and chest X-ray, he was discharged with a prescription for tramadol. After 2 days, the patient noted erythema and swelling in the aforementioned areas and returned to the ED. A soft tissue CT scan was done, showing infiltration in the anterior neck area, with no evidence of abscess. For this reason, the patient was again discharged, but this time with doxycycline. Four days later, he returned to the ED with pain and swelling that did not subside with previous treatment, in addition to fever and chills. Vital signs showed a blood pressure of 140/72 mmHg, temperature of 36.4°C, heart rate of 82 beats per min, respiratory rate of 18 breaths per min, and oxygen saturation of 98%. Physical examination showed swelling in the anterior area of the chest at the level of the right sternoclavicular joint. A second CT scan of the neck was done and showed a 2.5-cm abscess located in the sternocleidomastoid muscle (Figure 1). Laboratory test results upon admission are shown in Table 1. The patient received a dose of vancomycin and piperacillin/tazobactam 1 time, and the Infectious Disease Department was consulted, as was the Cardiothoracic Surgery Department for evaluation. Over the next 2 days, the clinical course improved, as the patient’s pain subsided. The infectious disease team switched antibiotics to cefepime and metronidazole, since blood cultures were positive for
Discussion
An intramuscular spontaneous abscess, specifically located in the sternocleidomastoid muscle, is extremely rare in non-endemic areas, especially when there are no risk factors involved. Its occurrence in temperate regions is, however, being documented with increasing frequency. In this region, striated muscle abscesses have been known to occur in patients with a history of trauma, immunosuppression, or uncontrolled diabetes. The present case was quite unusual in terms of anatomic location of the abscess and geographical location of the patient. The patient’s history of diabetes could have been contributory, as his hemoglobin A1c (HbA1c) level was 8.5%, but was not significantly elevated above the recommended levels 7% to 8% described by Qaseem, based on the National Institute for Health and Care Excellence’s and Institute for Clinical Systems Improvement guidelines [5]. However, the risk of bacteremia remained since the blood glucose level was not optimal, and this could have posed an issue. Zacay et al demonstrated a noteworthy study result showing the risk of cellulitis among patients with HbA1c >7.5% that was significantly increased, with an odds ratio of 1.4 [6], On the other hand, in a study by Thomsen et al, an increased risk of bacteremia with HbA1c >9% was concluded, with an odds ratio of 3.6 (1.6–8.1), which can result in an overall increased risk for infections, including of the soft tissue [7]. Whether this translates to an increased risk of spontaneous abscesses as well will require evaluation in further studies.
In the literature, this medical condition has also been called pyomyositis and was previously documented by Gosnell et al, in which the authors report the case of an immunocompetent individual who developed a streptococcal infection in the sternocleidomastoid muscle [8]. Furthermore, in this article are 7 cases of sternocleidomastoid muscle abscesses, all associated with underlying factors predisposing to the aforementioned condition. The treatment of these involves a combination of intravenous and oral antibiotic therapy, with or without surgical drainage, resulting in positive outcomes. Antibiotic therapy ranged in duration from 72 h to 12 weeks.
Another case of sternocleidomastoid pyomyositis was reported by Pandey et al, involving a young female patient with no signs of trauma or underlying disease who responded well to empirical antibiotics. Cultures did not yield an offending agent, as the antibiotic therapy had already begun prior to admission. This case occurred in India, a tropical region where the incidence for intramuscular abscesses is not particularly unusual [9]. However, the absence of risk factors, beyond diabetes, raises some questions about the pathophysiology of the condition and the relationship between the anatomy of the neck and bacteremia. Could it be the vascularization that exists in this location? Could it be the lymphatic pathways and the large presence of lymph nodes in the neck? Given the lack of literature, the prevalence and incidence of this particular condition is difficult to determine. To avoid a missed diagnosis and a potentially fatal outcome, a high index of suspicion is required and should be maintained for individuals who present without obvious risk factors.
Conclusions
Generally speaking, encountering cases of spontaneous abscesses is common in the context of individuals with notable risk factors. Different muscle groups have been documented with this entity. The sternocleidomastoid muscle, however, caught our attention as a peculiar location, particularly in this individual with diabetes mellitus but with no evidence of inoculation or trauma. However, bacteremia is not uncommon in those with impaired immune systems, as in this case, in which blood glucose levels were not optimal.
References:
1.. East J, Piper D, Chan S, Spontaneous intramuscular abscesses involving the rotator cuff muscles in two cases presenting during the COVID-19 pandemic: Cureus, 2020; 12(12); e11833
2.. Furuhata R, Inoue D, Kiyota Y, Dorsal subscapularis approach for the surgical drainage of subscapularis intramuscular abscess: A case report: BMC Musculoskelet Disord, 2019; 20; 445
3.. Mourkus H, Vadivelu R, Phillips J, Literature review and a case report of spontaneous subscapular abscess in a child: Eur J Orthop Surg Traumatol, 2018; 28(6); 1235-40
4.. Sidiqi MM, Witte B, Isolated spontaneous biceps abscess causing septic shock in a diabetic patient: A rare case report: Int J Surg Case Rep, 2020; 74; 82-85
5.. Qaseem A, Wilt TJ, Kansagara D, Hemoglobin A1C targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: A guidance statement update from the American College of Physicians: Ann Intern Med, 2018; 168(9); 569-76
6.. Zacay G, Sikron FH, Heyman AD, Glycemic control and risk of cellulitis: Diabetes Care, 2021; 44(2); 367-72
7.. Thomsen RW, Riis AH, Kjeldsen S, Schønheyder HC, Impact of diabetes and poor glycaemic control on risk of bacteraemia with haemolytic Streptococci groups A, B, and G: J Infect, 2011; 63(1); 8-16
8.. Gosnell EJ, Anwar B, Varadarajan V, Freeman S, Sternocleidomastoid pyomyositis: Eur Ann Otorhinolaryngol Head Neck Dis, 2016; 133(4); 273-75
9.. Pandey A, Keshri SY, Singh G, Sternocleidomastoid abscess mimicking a thyroid swelling in a young female: J Assoc Physicians India, 2017; 65(2); 84-85
In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943136
21 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943645
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250