04 January 2024: Articles 
Innovative Approach to Difficult Airway Management: Utilizing the Cook Airway Exchange Catheter for Double-Lumen Tube Intubation
Unusual setting of medical care
Adrien MaseriDOI: 10.12659/AJCR.942288
Am J Case Rep 2024; 25:e942288
Abstract
BACKGROUND: The Cook® Airway ExchangeCatheter (Cook® AEC, Cook Group Incorporated, Bloomington, Indiana, USA) is an 83-cm-long graduated hollow tube with an external diameter of 11, 14, or 19 French, commonly used for tracheal tube replacement. Although this application is reliable in the exchange of single-lumen tubes, the failure rate markedly rises during the exchange from a single-lumen to a double-lumen endotracheal tube. It is also often used as a bridge to extubation in patients with difficult airways and for oxygenation support applications.
CASE REPORT: We describe the case of a 58-year-old patient with unexpected difficult airway management. He was scheduled to undergo a minimally invasive hybrid esophagectomy (laparoscopic abdominal stage followed by an open right thoracotomy, requiring one-lung ventilation with a double-lumen tube). After the laparoscopic abdominal stage, performed with a single-lumen endotracheal tube, we exchanged it for a double-lumen endotracheal tube. After several unsuccessful exchanges with a Cook® Airway Exchange Catheter due to the flexibility of the exchange catheter, we decided to use the exchange catheter as a method to maintain adequate ventilation while using it as a target to facilitate tracheal intubation alongside it, using a videolaryngoscope.
CONCLUSIONS: This case report discusses an unusual use of the Cook® Airway ExchangeCatheter during videolaryngoscopic double-lumen endotracheal tube (DLT) intubation. It reviews previously documented uses in the literature, while highlighting the possibility of failure during tube exchange. It also highlights its value as a support for oxygenation and ventilation during difficult intubation attempts.
Keywords: Airway Extubation, airway management, case reports, Intubation, Intratracheal, Laryngoscopy
Background
The Cook® AEC (Cook® AEC, Cook Group Incorporated, Bloomington, Indiana, USA [1]) is an 83-cm-long graduated hollow tube with an external diameter of 11, 14, or 19 French (Fr), commonly used for tracheal tube replacement. Although this application is reliable in the exchange of single-lumen tubes, the failure rate markedly rises during the exchange from a single-lumen to a double-lumen endotracheal tube [2]. However, in clinical practice it is often used as a bridge to extubation in patients with difficult airways [3] or for oxygenation support. The selection of the external diameter of the Cook® AEC is based on the internal diameter of the single-lumen endotracheal tube (SLT) (Table 1). This case report discusses an unusual use of the Cook® AEC during videolaryngoscopic double-lumen endotracheal tube (DLT) intubation. It also highlights the value of its use as a support for oxygenation and ventilation during difficult intubation attempts.
Case Report
This is a case of a 58-year-old white man scheduled to undergo minimally invasive hybrid esophagectomy for adenocarcinoma of the lower third of the esophagus, classified as ASA 2, with hypertension and obesity (BMI 33.5 kg/m2). He reported no tobacco smoking, alcohol use, or substance abuse history. His usual oral therapy included perindopril 5 mg, indapamide 1.25 mg, amlodipine 5 mg, simvastatin 40 mg, allopurinol 300 mg, and moxonidine 0.4 mg.
In terms of predictive ventilation score, the DIFFMASK [4] score was 7 (age, sex, obesity, beard), corresponding to an intermediate risk of difficult mask ventilation. The patient was encouraged to shave his beard, but this is not generally mandatory at our institution, except in the case of planned awake fiberoptic intubation. Intubation was considered a low risk for advanced airway management: Mallampati score II, 3-finger mouth opening, thyromental distance greater than 6.5 cm, good neck extension, and neck circumference less than 40 cm. Assessment of esophageal cancer extension revealed 2 involved lymph nodes: one adjacent to the lesion on the right posterolateral side and the other subdiaphragmatic at the level of the lesser curvature. No secondary nodes were found. Ear, nose, and throat examination also revealed 2 small lesions in the right tonsil.
Standard ASA monitoring was used. Anesthesia was induced with 200 mg propofol, 25 mg esketamine, 50 mg rocuronium, 100 mg lidocaine, and 10 mcg sufentanil. Bag-valve ventilation was uneventful, but the first intubation attempt with a Macintosh size 3 laryngoscope blade failed (esophageal intubation, Cormack-Lehane score of IV). The Glidescope® (Verathon Incorporated, Bothell, Washington, USA) was then successfully used to insert a size 8.0 cuffed SLT.
For the thoracic stage, the SLT had to be replaced with a 39 Fr left DLT. A 14 Fr Cook® AEC was inserted into the SLT to guide the exchange under videolaryngoscopy. The initial attempt was unsuccessful. A size 8.0 SLT was again placed to ventilate the patient. We decided not to use the AEC for first-line ventilation as the first stage of the operation had already been performed and the displacement of the AEC would induce a risk of catastrophic esophageal distension.
Four attempts were made with the videolaryngoscope by various anesthetists, but it was not possible to place and advance the endotracheal tube through the vocal cords. We decided to leave the Cook® AEC in the trachea and connect it to the ventilator using the supplied Rapi-Fit® adapter (15-mm connector). We maintained ventilation at 6–8 ml/kg, 12/’ on the AEC, removed the SLT, and successfully intubated with the DLT under visual control of the videolaryngoscope. The endotracheal tube was then secured with a Sterisets® fixation cord (Sterisets® Medical Products, Penafiel, Portugal). Figure 1A–1C reproduces the described procedure on a simulation model of the case. There were no other significant events during the procedure. The patient received 125 mg of methylpredniso-lone to prevent laryngeal edema, was successfully extubated, and was then transferred to intensive care.
The procedure used to exchange the tube did not affect the patient’s outcome. He was able to return to the surgical ward 2 days later and was discharged home on postoperative day 13 without complications. The patient was subsequently lost to our institution as his oncological follow-up was carried out in another clinic. We learned from the National Global Health Network that his oncologist discovered complete invasion of his liver by metastases 2 months later. The patient died from these metastases 4 months after surgery, despite a new line of chemotherapy. He was not eligible for a liver transplant.
Discussion
This case highlights 2 different issues: the versatility of the Cook® AEC and the possibility that a tracheal tube exchange can fail even with a dedicated device.
The most common use of an airway change in the literature is to extubate a patient who has difficult airway management [3].
As described in the American Society of Anesthesiologists [5] and Difficult Airway Society guidelines, it is used as a guide for reintubation if extubation fails when using SLT. The AEC is inserted through the endotracheal tube, the SLT is removed, and the AEC is left in place in the trachea. An external diameter of 11- or 14-Fr is well tolerated in the awake patient. The usual insertion depth is 20 to 22 cm orally. It can be difficult to pass the device under the vocal cords when using small AECs (eg, an 11-Fr [6] catheter) because the relatively thin AEC is likely to move backwards when the larger, stiffer adult tracheal tube is advanced during reintubation. Advancing the SLT into the upper airway may then displace the AEC posteriorly into the esophagus and also snag on the arytenoid cartilage. It is therefore important to have an accurate correlation between the size of the AEC and the inner diameter of the endotracheal tube (Table 1). The greater rigidity of DLT compared to SLT and the relative flexibility of 14-Fr catheter may partly explain our difficulty in passing on DLT. The extra-firm version of Cook® AEC is specifically designed to replace double-lumen tubes, but was not available at our institution at that time. Another use of AEC is oxygen supplementation [7], either by jet ventilation or oxygen insufflation. It can also be used as a primary jet ventilation technique for maxillofacial or laryngeal surgery [8]. Failure of an SLT exchange attempt is another scenario where the AEC can be used to provide back-up oxygenation when the team needs time to consider an alternative airway management plan. It can be connected to one of the 2 Rapi-Fit® adapters supplied [1] and used for jet ventilation or conventional ventilation.
Potential complications [9] of AEC use include barotrauma in up to 11% of patients, pneumothorax, gastric distension and perforation, tracheal laceration and pneumomediastinum, and even cardiac arrest. Most of these cases were reported when the AEC was used with jet ventilation. However, 2 cases of tension pneumothorax [10,11] have been described in patients ventilated manually with an AEC. Another complication of the AEC is exchange failure due to displacement of the AEC when the first tube is removed before the second is placed [12]. The use of the AEC as a guide was described in a different setting by Saunders et al [13], who performed a nasotracheal to orotracheal tube exchange in a patient who had undergone awake fiberoptic intubation. They placed an AEC in the trachea through the nasal SLT and performed the tube exchange using a video-assisted fiberoptic intubation technique with the AEC as a guide. The AEC was not removed until the position of the orotracheal tube was confirmed.
Finally, the Cook® AEC can be used to exchange airway devices as part of a difficult airway management plan. An example is the replacement of a conventional SLT placed by awake fiber-optic intubation with a DLT via an AEC[14] in a patient with ankylosing spondylitis. Another example is fiberoptic intubation of a neonate with Pierre Robin syndrome [15] using an AEC to replace a supraglottic airway device (SAD) with an SLT without the risk of tracheal displacement when the SAD is removed.
Failure is not uncommon with tube replacement. Failure rates for tracheal tube exchanges can be as high as 9.3% for SLT to SLT and 39.9% for SLT to DLT [2]. In a study published by Mort [16], the success rate of reintubation from SLT to SLT in the ICU was 92%, with a first-pass success rate of 87% in patients with known or suspected difficult airways. One reason for failure in this article was inadvertent removal of the AEC from the glottis during the reintubation process. Video assistance has also been shown to be beneficial in tracheal tube replacement, increasing first-pass success rates [17].
We chose not to use a bronchial blocker in this patient because the surgical procedure involved extensive manipulation around the main bronchi and the risk of blocker displacement was high. In addition, the patient’s surgeon clearly favored the use of a double-lumen endotracheal tube over a bronchial blocker.
Conclusions
The Cook® AEC is a certified airway exchange catheter, but its use can be challenging when exchanging single-lumen to double-lumen endotracheal tubes. Its flexibility increases failure rates and can be managed with an extra-firm version of the AEC. It is also important to remember the ventilatory and oxygenation support role of the AEC during difficult intubations, allowing airway plans to be established in complete safety.
References:
1.. , Cook® Airway Exchange Catheter, 2022 [cited 2022 09 september]; Available from: https://www.cookmedical.com/products/cc_cae_webds/
2.. McLean S, Lanam CR, Benedict W, Airway exchange failure and complications with the use of the Cook Airway Exchange Catheter®: A single center cohort study of 1177 patients: Anesth Analg, 2013; 117(6); 1325-27
3.. Parotto M, Cooper RM, Behringer EC, Extubation of the challenging or difficult airway: Curr Anesthesiol Rep, 2020; 10(4); 334-40
4.. Lundstrøm LH, Rosenstock CV, Wetterslev J, Nørskov AK, The DIFFMASK score for predicting difficult facemask ventilation: A cohort study of 46,804 patients: Anaesthesia, 2019; 74(10); 1267-76
5.. Apfelbaum JL, Hagberg CA, Connis RT, 2022 American Society of Anesthesiologists practice guidelines for management of the difficult airway: Anesthesiology, 2022; 136(1); 31-81
6.. Law J, Duggan L, Extubation guidelines: Use of airway exchange catheters: Anaesthesia, 2012; 67(8); 918-19 ; author reply 921–22
7.. Duggan LV, Law JA, Murphy MF, Brief review: Supplementing oxygen through an airway exchange catheter Efficacy, complications, and recommendations: Can J Anesth, 2011; 58(6); 560-68
8.. Kim HT, Moon SY, Song DU, Lee KH, Airway management using O(2) flush via Cook airway exchange catheter® for microlaryngeal surgery: Korean J Anesthesiol, 2012; 63(1); 87-89
9.. Thomas V, Neustein SM, Tracheal laceration after the use of an airway exchange catheter for double-lumen tube placement: J Cardiothorac Vasc Anesth, 2007; 21(5); 718-19
10.. Rashid AM, Williams C, Noble J, Pneumothorax, an underappreciated complication with an airway exchange catheter: J Thorac Dis, 2012; 4(6); 659-62
11.. Chen WY, Lin JA, Chen HL, Pneumothorax associated with tube exchanger-aided intubation following LMA-Fastrach placement in a patient during anesthesia induction: Acta Anaesthesiol Taiwan, 2004; 42(4); 227-31
12.. Hwang SM, Lee JJ, Jang JS, Lee NH, Esophageal misplacement of a single-lumen tube after its exchange for a double-lumen tube despite the use of an airway-exchange catheter: Saudi J Anaesth, 2013; 7(2); 194-96
13.. Saunders TG, Gibbins ML, Seller CA, Videolaryngoscope-assisted flexible intubation tracheal tube exchange in a patient with a difficult airway: Anaesth Rep, 2019; 7(1); 22-25
14.. Karabiyik L, Altinay E, Bedirli N, Placement of a double lumen tube in a patient with difficult intubation due to ankylosing spondylitis – a case report: Middle East J Anaesthesiol, 2011; 21(1); 135-38
15.. Choi EK, Kim JE, Soh SR, Usefulness of a Cook® airway exchange catheter in laryngeal mask airway-guided fiberoptic intubation in a neonate with Pierre Robin syndrome – a case report: Korean J Anesthesiol, 2013; 64(2); 168-71
16.. Mort TC, Continuous airway access for the difficult extubation: the efficacy of the airway exchange catheter: Anesth Analg, 2007; 105(5); 1357-62 , table of contents
17.. Mort TC, Braffett BH, Conventional versus video laryngoscopy for tracheal tube exchange: Glottic visualization, success rates, complications, and rescue alternatives in the high-risk difficult airway patient: Anesth Analg, 2015; 121(2); 440-48
Tables
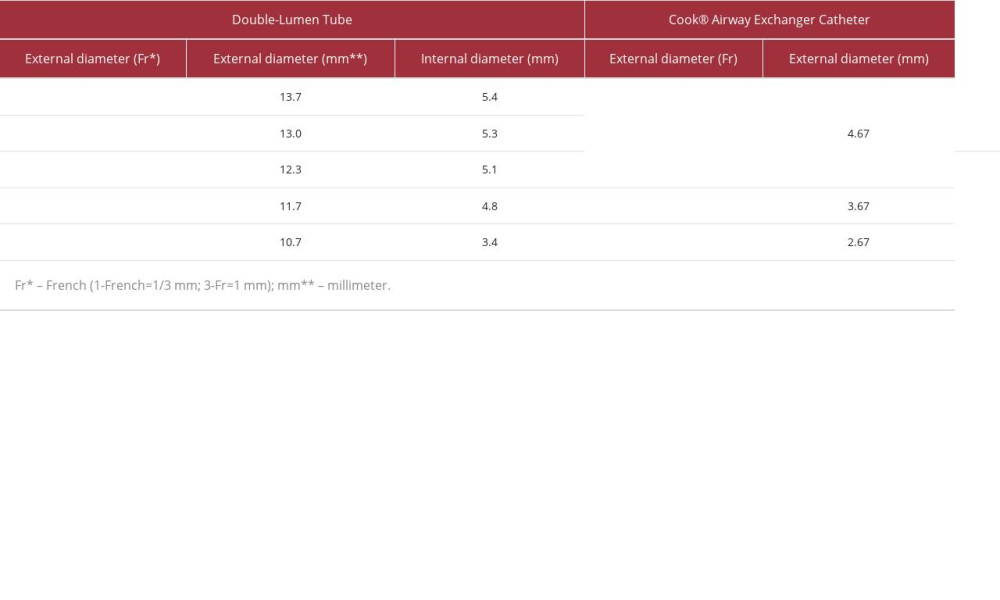 Table 1.. Comparison of the external diameter of the Cook® Airway Exchange Catheter with the internal and external diameter of the double-lumen endotracheal tube from Covidien® (Dublin, Ireland).
Table 1.. Comparison of the external diameter of the Cook® Airway Exchange Catheter with the internal and external diameter of the double-lumen endotracheal tube from Covidien® (Dublin, Ireland).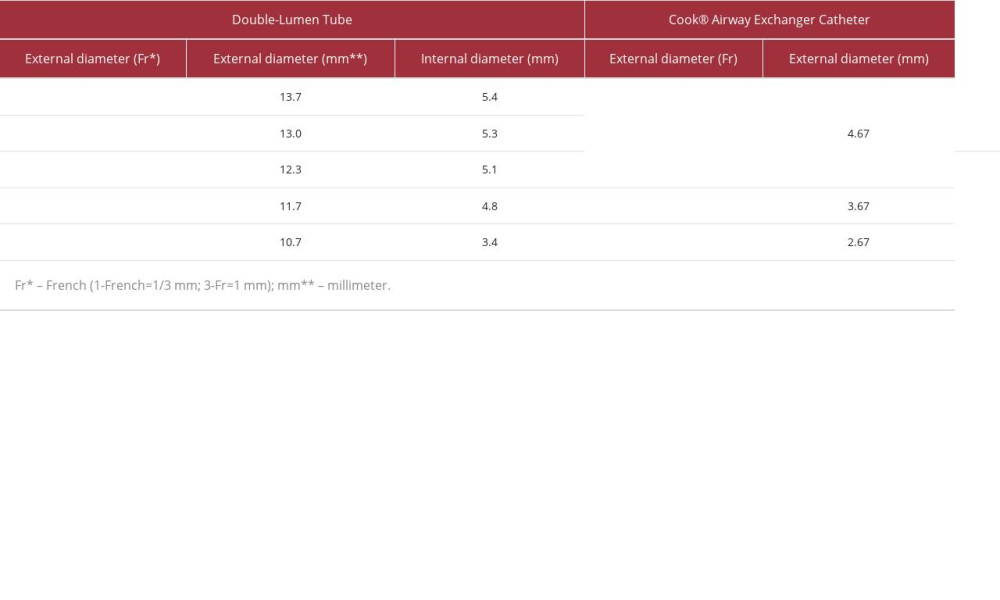 Table 1.. Comparison of the external diameter of the Cook® Airway Exchange Catheter with the internal and external diameter of the double-lumen endotracheal tube from Covidien® (Dublin, Ireland).
Table 1.. Comparison of the external diameter of the Cook® Airway Exchange Catheter with the internal and external diameter of the double-lumen endotracheal tube from Covidien® (Dublin, Ireland). In Press
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943376
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942853
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942660
19 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943174
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








