17 February 2024: Articles 
Successful Antiviral Treatment for Chronic Adenoiditis Caused by Herpes Virus in a Pediatric Patient: A Case Report
Unknown etiology, Challenging differential diagnosis, Unusual or unexpected effect of treatment
Leon KongDOI: 10.12659/AJCR.942418
Am J Case Rep 2024; 25:e942418
Abstract
BACKGROUND: The adenoids are lymphatic tissue located in the nasopharynx and play a role in upper-airway immunity. Inflammation of the adenoids is called adenoiditis, which can cause a variety of symptoms. This is a common condition and is due to acute viral or bacterial infection. Most patients experience mild symptoms of upper-respiratory tract infection with a self-limiting course.
CASE REPORT: A 5-year-old female patient was brought into the clinic by her parents with concerns regarding hearing and sleep. Clinical assessment was consistent with persistent otitis media with effusion and sleep-disordered breathing. She was scheduled for surgery, including nasendoscopy, adenoidectomy, and bilateral grommet insertion. During surgery, direct visualization of the postnasal space showed complete obstruction by hypertrophic, inflamed adenoids covered in a thick, white film. A biopsy was taken, which detected herpes virus cytopathic effect. A diagnostic workup excluded a neoplastic process and other bacterial or fungal infections. A trial of oral antiviral medication was successful and follow-up nasendoscopy showed resolution of adenoid hypertrophy.
CONCLUSIONS: Direct visualization of the postnasal space, with a transoral mirror or 120-degree endoscope, prior to adenoidectomy can aid diagnosis. Adenoiditis may be caused by a wide range of organisms, including herpes virus. Active mucopurulent discharge should raise concern for infection by bacteria, fungi, or virus. Previous research on viral infection of the adenoids have been in asymptomatic patients with presumed latent infection and undergoing elective adenoidectomy. To our knowledge, this is the first paper to report on successful treatment with antiviral medication alone.
Keywords: case reports, Adenoids, Varicella Zoster Virus Infection
Background
The adenoids are lymphatic tissue located in the nasopharynx, consisting of B and T lymphocytes. As part of Waldeyer’s ring of mucosa-associated lymphoid tissue (MALT), the adenoids play a role in upper-airway immunity as the first line of defense against inhaled or ingested pathogens [1,2]. Physiological growth of the adenoids peaks around the age of 7 years, and they tend to atrophy during adolescence [3]. Inflammation of the adenoids is called adenoiditis, which can cause a variety of symptoms. This is commonly related to acute viral or bacterial infection. Most patients experience mild symptoms of upper-respiratory tract infection with a self-limiting course. Adenoidectomy is a frequently employed treatment for chronic cases, with an incidence of 3–7 per 1000 people [1]. In this report, we present a child who was found to have an unusual chronic infection of the adenoids by herpes virus, resulting in systemic manifestations. Written consent has been obtained from the patient’s parent to present this case in accordance with the Case Report guidelines.
Case Report
In September 2022, a 5-year-old girl presented to the outpatient Ear Nose Throat (ENT) clinic due to concerns regarding persistent otitis media with effusion (OME) and sleep-disordered breathing. For the past 4 months, her parents had noticed her hearing had deteriorated such that she would ignore them when they were trying to talk to her. She suffered from nasal obstruction and tended to mouth breath. Recently, her parents had noticed loud snoring at night. She was constantly unwell with either nose or throat infections. She was more lethargic than before, with associated loss of appetite, intermittent vomiting, and weight loss of 5 kg over this period. She reported intermittent otalgia with otorrhea. She denied puru-lent rhinorrhea, facial pain, sore throat, reflux, skin rash, joint pain, fevers, or gastrointestinal disturbance.
Her medical history was relevant for 1 prior episode of acute otitis media and tonsillitis. She had an uncomplicated birth history. She was fully immunized. She did not have any regular medications or known drug allergies. Her family history included maternal fallopian tube tuberculosis (TB) treated 2 years prior to pregnancy. The family had moved from Wellington to Hamilton in the past 4 months. There had not been any overseas travel since the COVID-19 pandemic. They had previously travelled to India.
Past interventions included 5 courses of oral antibiotics in the last 4 months, including 4 courses of amoxicillin 15 mg/kg 3 times a day (5 days) and 1 course of sulfamethoxazole-trimethoprim 400/80 mg 2 times a day (7 days) with minimal benefit. The patient had not been receiving anti-allergy treatment such as intranasal steroid or antihistamines.
On examination, she was alert. There were bilateral deep cervical lymph nodes palpable. Oral cavity examination showed grade 2 tonsils with pharyngeal inflammation. Anterior rhinoscopy showed non-inflamed turbinates and a patent nasal airway. Otoscopy revealed dull tympanic membranes bilaterally, indicative of middle-ear effusion. She had an otherwise normal cardiopulmonary and abdominal examination. Tympanometry had been monitored by a community Ear Clinic nurse, with persistent B tympanograms bilaterally for the past 3 months (Figure 1).
The patient was scheduled for surgery 2 days later. The initial surgical plan was for nasendoscopy, adenoidectomy, and bilateral myringotomy, and Sheehy grommet insertion. She had thick middle-ear effusions and had grommets inserted. However, there were also unexpected intraoperative findings. The entire nasopharynx appeared abnormal (Figure 2). There was total obstruction of the posterior choanae by a white film covering hypertrophic adenoids, which extended into the nasal cavity with no view of the nasal septum via posterior rhinoscopy with a transoral mirror. The white film was very thick and tenacious and completely covered the Eustachian tubes. Suctioning was ineffective and the tissue was friable and bled easily on contact. The experienced surgeon had not seen this appearance before in clinical practice. Due to concern for neoplastic or atypical infectious process, the decision was made to limit the nasopharyngeal intervention to biopsy and saline irrigation. Multiple biopsies were taken and sent for microscopy, culture (bacteria, diphtheria, TB, fungus), cytology, and histology. No antibiotics were prescribed postoperatively given previous failed courses.
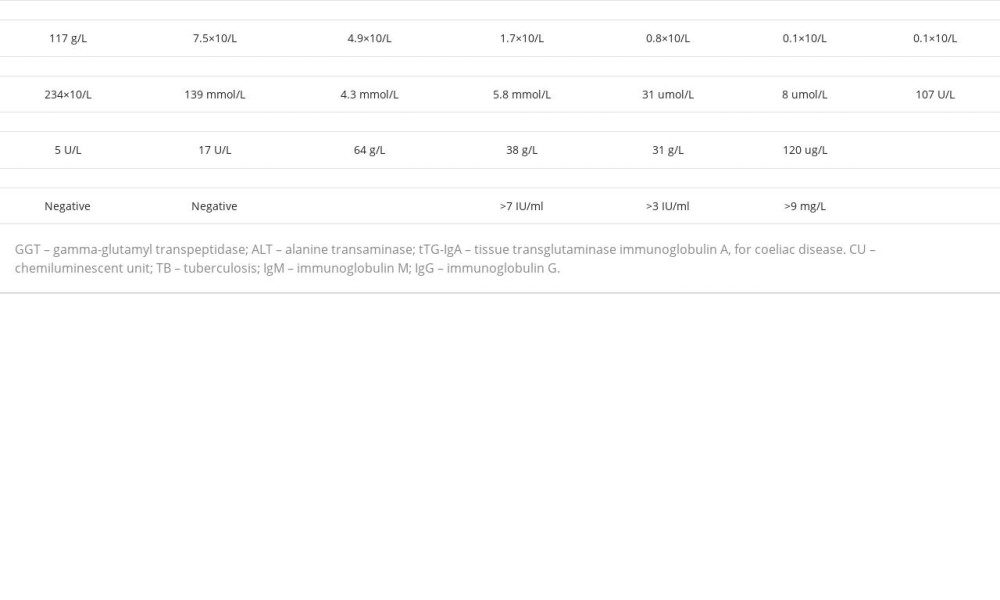
As part of the diagnostic workup, chest X-ray and blood tests including full blood count, renal function, liver function, coeliac screen, QuantiFERON Gold, and antibody levels (Mycoplasma pneumoniae, Bordetella pertussis toxin, Tetanus, diphtheria, Haemophilus influenzae) were ordered (Table 1). C-reactive protein (CRP) and procalcitonin were not tested. These did not reveal any underlying abnormality. The patient was also referred for review by the pediatrician.
Histology report (Figure 3): microscopic: squamous mucosa exhibiting superficial ulceration with an overlying purulent exudate.
Periodic acid-Schiff (PAS) stain for fungal organisms was negative.
Acid-fast stain and mycobacteria culture was negative.
Step sections of the tissue showed herpes virus cytopathic effect. Further immunohistochemistry was performed and was negative for herpes simplex virus 1 (HSV1), herpes simplex virus 2 (HSV2), and cytomegalovirus (CMV).
Two weeks after surgery, she was reviewed by the pediatrician and based on the above findings was started on a 10-day course of oral acyclovir 200 mg 5 times a day. One week later, she was reviewed by the otolaryngologist and the patient reported significant improvement in appetite, sleep, and energy. No adverse effects were reported. A follow-up nasendoscopy done in the ENT clinic in November 2022 showed no adenoidal obstruction and no signs of active postnasal space infection (Figure 4). The patient was reviewed at 1 year with no further recurrence of adenoid obstruction or infection.
Discussion
This case demonstrates a patient who suffered from persistent middle-ear effusion and sleep-disordered breathing. This was found to be related to inflammation and hypertrophy of the adenoids, which was eventually diagnosed as chronic viral adenoiditis due to herpes virus. This case highlights the benefit of direct examination of the postnasal space prior to adenoidectomy. This will allow detection of unusual pathology and prevention of unnecessary surgery. For a cooperative patient, this can be attempted in-clinic with flexible nasendoscopy. However, as it is common for younger patients to refuse this when awake, often the opportunity for direct examination is not afforded until the time of surgery. We suggest using an indirect transoral mirror or a 120-degree endoscope for visualization.
Pathology of the adenoid is usually related to adenoiditis or adenoid hypertrophy. Adenoiditis may present with nasal obstruction, nasal discharge, mouth-breathing, and postnasal drip syndrome (chronic cough, throat clearing). This can affect patients in various ways, including contributing to sleep-disordered breathing or obstructive sleep apnea, as well as Eustachian tube dysfunction and otitis media with effusion [1]. Long term effects include adenoid facies, which are characteristic physical features affecting maxillofacial development due to mouth-breathing, including narrow maxillary arches, upper-lip incompetence, lower-mandible position, and downward tongue position [4]. The effects of untreated otitis media with effusion can be detrimental, including hearing impairment and speech delay.
Purulent nasal discharge as a symptom is commonly reported with self-limiting upper-respiratory tract infection and sinusitis. However, this patient had chronic symptoms and endoscopic examination revealed a thick white mucopurulent film over the adenoids. The differential diagnoses to consider include bacterial infection (such as diphtheria), fungal infection (candidiasis), and foreign-body reaction. Diphtheria due to
Adenoids can act as a reservoir for bacteria and viruses [3]. A wide spectrum of different viruses, including herpes and common respiratory viruses, have been detected in adenoidectomy samples. A diagnosis of virus infection can be made by a combination of tests including serology, polymerase chain reaction (PCR), culture and biopsy [9]. Many viral infections have characteristic cytologic changes (viral cytopathic effect) that can enable definitive diagnosis by H&E alone [9]. Studies by various authors have found a >94% chance of detecting at least 1 viral species in adenoidectomy samples by PCR [2,10,11]. The common herpes viruses detected in the adenoids include Epstein-Barr virus (EBV), human herpesvirus-6 (HHV-6), and human herpesvirus-7 (HHV-7) [2,10,11]. However, most of these patients do not have symptoms of active infection [10,11]. This result suggests chronic infection in the respiratory tract and confounds the significance of pathogens detected during acute respiratory infections. Herpes viruses are usually acquired via respiratory tract secretions or saliva during childhood. Primary infection is usually asymptomatic or causes only mild symptoms [10]. Characteristically, herpes virus persists in the host as a lifelong infection after primary infection, termed latency [3,10]. For example, primary infection of varicella (chick-enpox) in young children causes a generalized vesicular rash. Antiviral medication is not indicated unless the host is immunocompromised [12].
However, unlike the previous studies, our case demonstrates that on rare occasions, a virus can be attributed to symptomatic disease. The virus implicated in this case is most likely varicella zoster virus (VZV). This would be consistent with the cytopathic effect observed, which has a similar appearance to HSV1 and HSV2 [12]. HSV1, HSV2, and CMV were excluded by immunohistochemistry. EBV, HHV-6, and HHV-7 were unlikely because they do not typically induce cytopathic changes in cell culture [12]. Of interest, the rate of VZV found in adenoids from studies by Ivaska and Sato were 0% [10,11]. Previous papers reporting on viral infections of the adenoids have been exclusively on patients undergoing adenoidectomy [2,10,11]. None have explicitly reported on the use of antiviral medication prior to surgery. To our knowledge, this paper is the first to report on successful treatment of adenoiditis and adenoid hypertrophy with antiviral medication.
Investigation of suspected adenoiditis includes either direct nasendoscopy, which may reveal adenoid edema and mucopurulent discharge, or a lateral neck X-ray showing an enlarged adenoid pad [6]. Abnormal postnasal space tissue can be biopsied and sent for histology and microbial culture. In our case, a viral cytopathic effect was observed in the tissue, suggesting this was not merely a latent infection. A trial of antiviral medication had a dramatic benefit, which again supports the diagnosis of herpes virus as the underlying cause. A non-surgical approach may be preferred in select cases, such as patients with cleft palate or trisomy 21 who are at higher risk of post-operative velopharyngeal insufficiency. Under routine circumstances, a trial of medical therapy with nasal steroid spray could be considered, with adenoidectomy reserved for cases with symptoms persisting over 3 months [4]. Further research should include identification of appropriate patients with active adenoiditis and observing if they benefit from antiviral or antibiotic medication, which should be guided by biopsy and/or culture.
Conclusions
The presence of nasal symptoms and/or associated complications, including sleep and otologic pathology, should prompt direct visualization of the postnasal space for diagnosis of adenoid-related pathology. Although active mucopurulent discharge can often be related to infection by bacteria or fungi, a viral cause should be kept in the differential. In this case, the patient’s presentation was attributed to a herpes virus, which is more often reported as a latent infection. Antiviral medication was prescribed, with clinical resolution, without the need for other measures normally employed in adenoid pathology, including nasal steroid spray or surgery.
Figures
References:
1.. Paramaesvaran S, Ahmadzada S, Eslick GD, Incidence and potential risk factors for adenoid regrowth and revision adenoidectomy: A meta-analysis: Int J Pediatr Otorhinoloaryngol, 2020; 137; 110220
2.. Faden H, Callanan V, Pizzuto M, The ubiquity of asymptomatic respiratory viral infections in the tonsils and adenoids of children and their impact on airway obstruction: Int J Pediatr Otorhinolaryngol, 2016; 90; 128-32
3.. Lomaeva I, Aghajanyan A, Dzhaparidze L, Adenoid hypertrophy risk in children carriers of G-1082A polymorphism of IL-10 infected with human herpes virus (HHV6, EBV, CMV): Life, 2022; 12; 266
4.. Mnatsakanian A, Heil JR, Sharma S, Anatomy, head and neck: Adenoids: StatPearls [online], 2022 [cited 2023 Oct 30]. Available from:https://www.ncbi.nlm.nih.gov/books/NBK538137/
5.. Truelove SA, Keegan LT, Moss WJ, Clinical and epidemiological aspects of diphtheria: A systematic review and pooled analysis: Clin Infect Dis, 2020; 71(1); 89-97
6.. Wang H, Chronic adenoiditis: J Int Med Res, 2020; 48(11); 300060520971458
7.. Karpova EP, Kharina DV, [The possibilities for the rational pharmacotherapy of adenoiditis in the children.]: Vestnik Otorinolaringologii, 2016; 81(5); 73-76 [in Russian]
8.. Vila T, Sultan AS, Montelongo-Jauregui D, Jabra-Rizk MA, Oral candidiasis: A disease of opportunity: J Fungi (Basel), 2020; 6(1); 15
9.. Solomon IH, Hornick JL, Laga AC, Immunohistochemistry is rarely justified for diagnosis of viral infections: Am J Clin Pathol, 2017; 147; 96-104
10.. Ivaska LE, Silvoniemi A, Mikola E, Herpesvirus infections in adenoids in patients with chronic adenotonsillar disease: J Med Virol, 2022; 94(9); 4470-77
11.. Sato M, Li H, Ikizler M, Detection of viruses in human adenoid tissues by use of mulitplex PCR: J Clin Microbiol, 2009; 74(3); 771-73
12.. Whitley RJ, Herpesviruses: Medical microbiology, 1996, Texas, University of Texas Medical Branch at Galveston chapter 68
Figures
In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250