26 February 2024: Articles 
Treatment of Medication-Related Osteonecrosis of the Jaws without Segmental Resections: A Case Series
Unusual clinical course, Challenging differential diagnosis, Unusual or unexpected effect of treatment, Diagnostic / therapeutic accidents, Rare disease, Adverse events of drug therapy, Educational Purpose (only if useful for a systematic review or synthesis)
Tito Lúcio FernandesDOI: 10.12659/AJCR.942980
Am J Case Rep 2024; 25:e942980
Abstract
BACKGROUND: Medication-related osteonecrosis of the jaw (MRONJ) is a rare but serious reaction to anti-resorptive drugs (ARDs) in patients treated for osteoporosis and conditions related to cancer. Treatment for MRONJ consists of the use of non-operative therapies according to the evolution of the disease, which consist of the use of antimicrobial mouthwashes, systemic antibiotics, and operative therapies, such as debridement of necrotic bone, marginal or segmental resection, and bone reconstruction of the jaws in more advanced stages of the disease.
CASE REPORT: This is a case series of 11 female patients treated for MRONJ, with a mean age of 76.5 years. Patients with malignant diseases of the jaws or those undergoing head and neck radiotherapy were excluded. Nine patients were medicated for osteoporosis with oral bisphosphonates and denosumab, and 2 patients used zoledronate to treat metastatic breast cancer. MRONJ prevailed in the mandible, most patients were classified as stage 2, and the most frequent triggers were tooth extraction and prosthetic trauma. All patients initially underwent non-operative therapies and were operated according to MRONJ stage, but none required segmental resection. Adjuvant treatments were used in 5 patients, and mean treatment and follow-up periods were 5 and 18.3 months, respectively. There was complete resolution of disease in all patients, with only 1 relapse.
CONCLUSIONS: This case series suggests that it is possible to treat MRONJ with conservative therapies in the early stages of the disease and minimally invasive surgeries in more advanced stages of the disease, thus avoiding segmental jaw resections.
Keywords: Bisphosphonate-Associated Osteonecrosis of the Jaw, Bone Density Conservation Agents, Minimally Invasive Surgical Procedures, Oral Surgical Procedures, osteonecrosis, Evidence-Based Dentistry
Background
Medication-related osteonecrosis of the jaw (MRONJ) is a rare disease, first described by Marx in 2003 [1], that consists of an adverse reaction to antiresorptive drugs (ARDs) used alone or in combination with immunomodulators or antiangiogenic drugs in patients either currently or previously treated for conditions related to cancer, osteoporosis, and osteopenia [2,3]. There are millions of people worldwide diagnosed with osteoporosis, and the medications mostly used in its treatment are bisphosphonates, denosumab, raloxifene, teriparatide, and, more recently, romosozumab [4]. The main hypotheses related to the pathophysiology of MRONJ are inhibition of bone remodeling, inflammation or infection, inhibition of angio-genesis, innate or acquired immune dysfunction, and genetic predisposition [3].
The American Association of Oral and Maxillofacial Surgery (AAOMS) recently updated the MRONJ staging system to better characterize all aspects of its clinical and radiographic presentation [2,3] (Table 1). The risk of developing MRONJ in patients exposed to antiresorptive therapy for the treatment of osteoporosis with oral bisphosphonates is 0.02% to 0.05%, with denosumab the risk is 0.04% to 0.3%, and with romosozumab it is 0.03% to 0.05%. On the other hand, in cancer patients treated with denosumab the risk of MRONJ is 6.9%, and in patients exposed to zoledronate it can be as high as 18% [3].
Due to the increasing knowledge of MRONJ by healthcare professionals, a large number of patients have been diagnosed at disease stage 0, which highlights the importance of early diagnosis to achieve better treatment results [5].
Standard treatment for MRONJ consists of discontinuing the ARD, using antimicrobial rinses or systemic antibiotics, and performing surgeries such as debridement of necrotic bone or segmental resection and vascularized bone reconstruction in advanced stages of the disease [2,6,7].
The AAOMS has recently developed a series of treatment algorithms to streamline the management strategies for patients with MRONJ. These strategies consist of non-operative (Figure 1) and operative therapies (Figure 2), used in all stages of the disease [3].
The aim of this study was to retrospectively evaluate the outcome of a consecutive series of patients treated for MRONJ without segmental jaw resections in a private oral and maxillofacial surgery clinic in southern Brazil.
Case Reports
A retrospective review of the database of a private oral and maxillofacial surgery clinic in southern Brazil was conducted. All adult patients diagnosed with MRONJ from September 2011 to March 2023 were selected, and patients with malignant diseases of the jaws or those undergoing head and neck radiotherapy were excluded [2].
A review of the medical records of the selected individuals was carried out to obtain data including age and sex, history of anti-resorptive therapy (with indication of the pathology for which it was used), type, route and duration of administration, co-morbidities, and predisposing factors for MRONJ. Clinical and imaging characteristics, location, triggering factors, and stage of the disease were also recorded at initial presentation. Operative and non-operative treatments performed were registered, as were adjuvant treatments used, duration and results of treatments, incidence of complications, relapse and follow-up time (Table 2), and a checklist of the main diagnostic and therapeutic procedures used to treat MRONJ (Table 3) [3,7].
The Research Ethics Board of the State University of Ponta Grossa, Paraná, Brazil, approved this study (CAAE – 47185721. 1.0000.0105).
A total of 11 female patients were included in this study. The mean age at the start of treatment was 76.5 years (range, 58 to 85 years). Most patients (81.8%) were medicated with oral bisphosphonates (alendronate and ibandronate sodium) to treat osteoporosis, 2 of which were initially treated with a bisphosphonate and later received denosumab (Prolia, Amgen Technology, Dublin, Ireland). Only 2 patients (18.2%) were exposed to intravenous zoledronate (Zometa, Novartis, Stein, Swiss) to treat metastatic breast cancer. The time of exposure to ARDs ranged from 2 to 20 years (mean 8.6 years), and most patients (8 out of 9) who used medications for more than 4 years presented with a more advanced stage of the disease (Figure 3).
The most frequent comorbidities observed in patients were depression, cardiac arrhythmia, and systemic arterial hyper-tension, followed by hypothyroidism, dyslipidemia, smoking, bronchial asthma, autoimmune myositis, hemorrhagic gastritis, sarcopenia, fibromyalgia, rheumatoid arthritis, osteoarthritis, diabetes mellitus, and alcoholism (Figure 4). In addition, some patients had concomitant comorbidities, with up to 5 of them.
MRONJ lesions were mostly diagnosed in the posterior region of the mandible (45.4%), followed by the anterior mandible (27.3%), posterior maxilla (18.2%), and anterior maxilla (9.1%). At the initial clinical presentation, alveolar bone exposure was found in 45.4% of cases. In addition, the patients presented clinical signs such as suppuration, edema or gingival hyperemia, paresthesia, intra and extraoral fistulas, spontaneous sequestration, mandibular neuralgia, and verrucous lesions on the floor of the mouth.
The initial imaging evaluation consisted of panoramic radiographs and computed tomography (CT) scans, which revealed alveolar osteolysis in most cases (90.9%), which extended beyond the alveolar bone in 4 cases. Only 1 patient presented with alveolar osteosclerosis on the posterior maxilla. Patients were classified according to initial clinical and radiographic presentation as stage 1 (9.1%), stage 2 (54.5%), and stage 3 (18.2%).
The most frequent triggers for MRONJ observed in this group were tooth extraction and prosthetic trauma (36.4% each), followed by dental implant therapy (27.2%). There was 1 patient whose initial trigger was mandibular implant therapy, which subsequently relapsed in another region of the mandible due to prosthetic trauma. This patient was initially classified as stage 3 and later reclassified as stage 2. In addition, 2 patients had dual MRONJ triggers: 1 patient required endodontic treatment adjacent to a tooth extraction site, while the other had prosthetic trauma and experienced a fall that led to a concomitant mandibular fracture.
The mean evolution of MRONJ before diagnosis and treatment beginning was 4.5 months (range, 1 to 12 months). All patients started non-operative treatment with 0.12% chlorhexidine digluconate rinses (Periogard, Colgate-Palmolive, São Paulo, SP, Brazil), and those who presented suppuration or underwent operative treatment received antibiotics. Surgeries were performed on all patients and consisted of sequestrectomies, dental implant removals, and debridements. Three patients required marginal resections with piezosurgery, 2 in the mandible (Piezosurgery, Mectron, Carasco, GE, Italy) and 1 in the maxilla (Osteomed, Rio Claro, SP, Brazil). Some patients required additional surgeries, such as sequestrectomy for MRONJ relapse, removal of remaining dental implants, and an apicoectomy in a tooth adjacent to the osteonecrosis site.
Most surgeries (72.7%) were performed on an outpatient basis with local anesthesia and oral sedation, and only 3 patients were treated under general anesthesia in a hospital setting.
Adjuvant treatment for MRONJ was performed in 5 patients (45.4%). Pentoxifylline 800 mg/day with tocopherol 800 mg/day [16] (PENTOCO) was administered in 4 patients, and hyperbaric oxygen therapy (HBOT) was used in 1 patient, who subsequently received PENTOCO for the treatment of MRONJ relapse.
The average duration of treatments was 5 months (ranging from 1 to 19 months), and the patient with the longest treatment had a pathological fracture in the left mandibular body due to a fall but had no alveolar bone exposure. This patient initially received non-operative treatment with PENTOCO for 18 months, the mandibular fracture repaired spontaneously, and surgery was performed to treat a late alveolar bone exposure (Figure 5).
Ten patients evolved with complications related to the surgical wound, and the most frequent was suture dehiscence (Vicryl 4-0 and Monocryl 4-0, Ethicon, Johnson & Johnson, São Paulo, SP, Brazil; 90.9%), requiring only local wound care, and 1 of these patients had an oronasal fistula for 1 month postoperatively, which healed spontaneously. In spite of such events, all patients had a good evolution of the disease, with resolution of oral symptoms and complete bone healing at the operated sites, and were pain-free after treatment.
There was only 1 MRONJ relapse 3 years after surgery due to prosthetic trauma (Figure 6). The mean follow-up of patients in this study was 18.3 months (range, 3 to 52 months).
Discussion
MRONJ diagnostic criteria and treatment protocols have changed over the years. When initially described, it was a disease characterized by bone exposure of the jaws and was restricted to patients who used bisphosphonates [1,2]. Currently, MRONJ can present without necrotic bone exposure and, due to the emergence of new forms of treatment for osteoporosis and metastatic bone disease, it can be related to antiangiogenic drugs and ARDs other than bisphosphonates [3,8]. Only 1 patient in this series did not initially present with bone exposure and had an intraoral fistula. Although this patient had MRONJ stage 3, with marked bone destruction in the anterior region of the mandible, non-operative treatment was attempted for 18 months with the adjuvant use of PENTOCO. After this time, the mandibular osteo-necrosis improved but it progressed with alveolar bone exposure and required surgery, with marginal resection of the mandible.
MRONJ is limited to the jaws, due to the greater vascularization and bone turnover rate. It prevails in the mandible (75%), and the occurrence can be related to the type, dose, and route of administration of the ARD, with greater risk from the parenteral route. In addition, patients with more than 4 years of anti-resorptive therapy have a potential risk of MRONJ as high as 0.21% [4,9,10]. In this series, most patients developed MRONJ in the mandible (72.7%) and used oral bisphosphonates to treat osteoporosis (81.8%). The only 2 patients exposed to intravenous medication to treat breast cancer metastasis developed the disease in the maxilla.
Diabetes mellitus, smoking, and immunosuppressive medications are risk factors for MRONJ, and patients with osteoporosis and immunodeficiency are at increased risk [11,12]. One patient in this series had diabetes mellitus, 2 patients were smokers, and 1 of them was also an alcoholic. In addition, 2 other patients had autoimmune diseases (rheumatoid arthritis and autoimmune myositis), of which 1 patient used immunomodulators during the anti-resorptive therapy.
Therefore, MRONJ is a multifactorial disease with a synergistic effect of trauma, infection, and decreased bone turnover.
Tooth extractions, prosthetic trauma, and dental implant therapy can also trigger the onset of MRONJ. Patients undergoing tooth extractions have a risk of developing MRONJ, from 0.5% to 1%, reaching up to 5% in high-risk patients, which is similar to the risk of developing osteoradionecrosis in irradiated patients. Furthermore, patients with dental implants exposed to denosumab have a 0.5% risk of developing the disease [11,13,14]. Hence, tooth extraction, prosthetic trauma, and dental implant therapy were the most frequent triggering factors among patients in this series.
Current MRONJ treatment strategies emphasize that both non-operative and operative management are acceptable for all stages of the disease, based on clinical judgment and individual patient factors. Patients who are refractory to non-operative treatment or who are unable to maintain adequate oral hygiene are candidates for operative therapy. Thus, the risk-benefit ratio should take into account the individual’s ability for wound caring in order to prevent infection and spread of disease, the morbidity of an invasive surgical procedure, and oral rehabilitation concerns after marginal or segmental resection surgery [3]. All patients in the series were initially treated non-operatively but even so, as bone exposure and associated symptoms persisted, they all required surgeries that ranged from minimally invasive procedures to marginal re-sections. This may be related to the fact that most patients (10/11) presented with MRONJ stages 2 and 3. Furthermore, of the 3 patients with MRONJ stage 3 who underwent marginal resections, 2 developed disease in the mandible and 1 in the maxilla, and most importantly, no patient required segmental resection. Additionally, the only patient who underwent maxillary marginal resection presented wide exposure of the maxillary sinus, requiring the use of a pedicled graft with a buccal fat pad [15].
Regardless of treatment modality and stage of MRONJ, discontinuation of the anti-resorptive therapy before or early in treatment is associated with faster disease resolution, whereas continuation of this therapy can delay symptom resolution by approximately 4 to 6 months [6]. All patients in this series had the anti-resorptive therapy discontinued at the beginning of treatment with the agreement of the prescribing physician, and were instructed to restart the medication from 3 to 6 months after the resolution of the disease.
Adjuvant therapies in the treatment of MRONJ can include the application of low-level laser, HBOT, ozone, and photodynamic therapies, platelet and leukocyte-rich fibrin in the surgical sites, and the use of medications, such as teriparatide and PENTOCO, among other therapies [3,11,16–18]. In the early cases of this series, adjuvant therapies were not used for the treatment of MRONJ, due to the lack of scientific evidence at the time. With the emergence of new treatment protocols, in 2019, HBOT was used as an adjuvant therapy in a patient with stage 3 MRONJ with good results, but this treatment became difficult because the patient needed to travel daily for sessions. Recently, PENTOCO has been our adjuvant therapy of choice for MRONJ, with satisfactory clinical results.
Current findings suggest that MRONJ can be responsibly prevented in patients using ARDs, and treated predictably in those patients who develop the disease. Additionally, some recently introduced compounds have been demonstrated to have a significant influence on the oral environment [19]. The use of lysates [20] and postbiotics [21] can modify clinical and micro-biological parameters in periodontal patients; therefore, these products should be considered in future clinical trials as adjuvants and in MRONJ prevention and management.
It is essential to emphasize the need for professional and scientific interaction between healthcare professionals for the prevention and treatment of MRONJ, particularly between physicians who treat metabolic and metastatic bone diseases and dental surgeons, who are responsible for the prevention, diagnosis, and treatment of the disease. The lack of diagnosis and correct treatment of MRONJ by healthcare teams can lead to disastrous consequences for patients, such as the occurrence of pathologic mandibular fracture and its complications [22].
The limitations of this study are its retrospective nature and small sample size. Therefore, prospective studies and randomized clinical trials, preferably with a multicenter design to reach a large number of cases, that compare operative vs non-operative treatment protocols, or more conservative vs aggressive operative protocols for the treatment of MRONJ, and that evaluate available adjuvant treatments [10], are important to elucidate the best way to treat patients with this rare disease.
Conclusions
This study highlighted the importance of early diagnosis of MRONJ and the use of more conservative methods to treat it. The use of conservative techniques in the early stages of the disease and minimally invasive surgeries in more advanced stages can avoid segmental jaw resections that require extensive bone reconstruction, which significantly impacts patients’ quality of life.
Figures
Tables
Table 1.. American Association of Oral and Maxillofacial Surgery clinical and radiographic staging system of medication-related osteonecrosis of the jaw.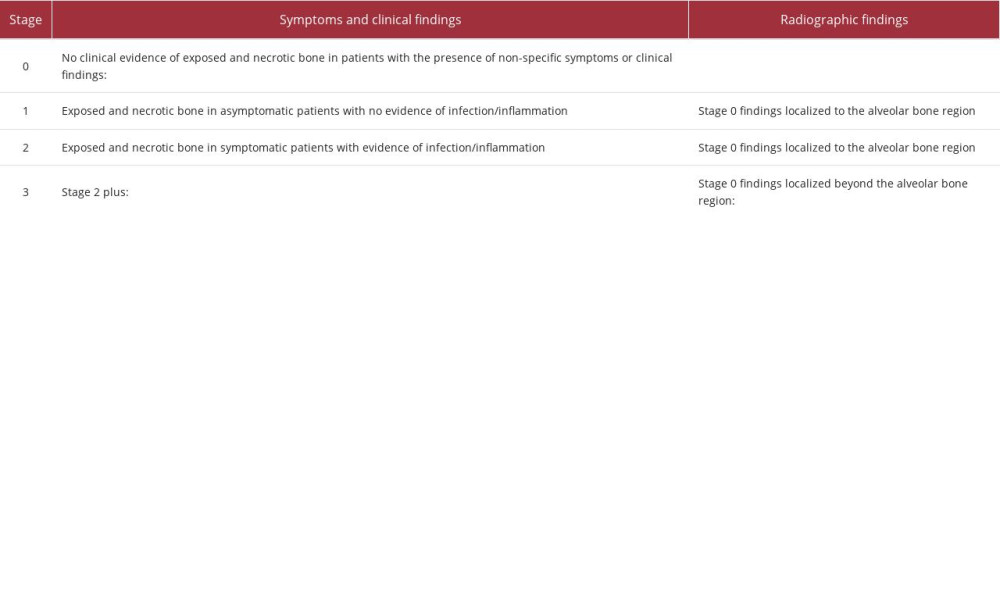 Table 2.. Patients treated for medication-related osteonecrosis of the jaws.
Table 2.. Patients treated for medication-related osteonecrosis of the jaws.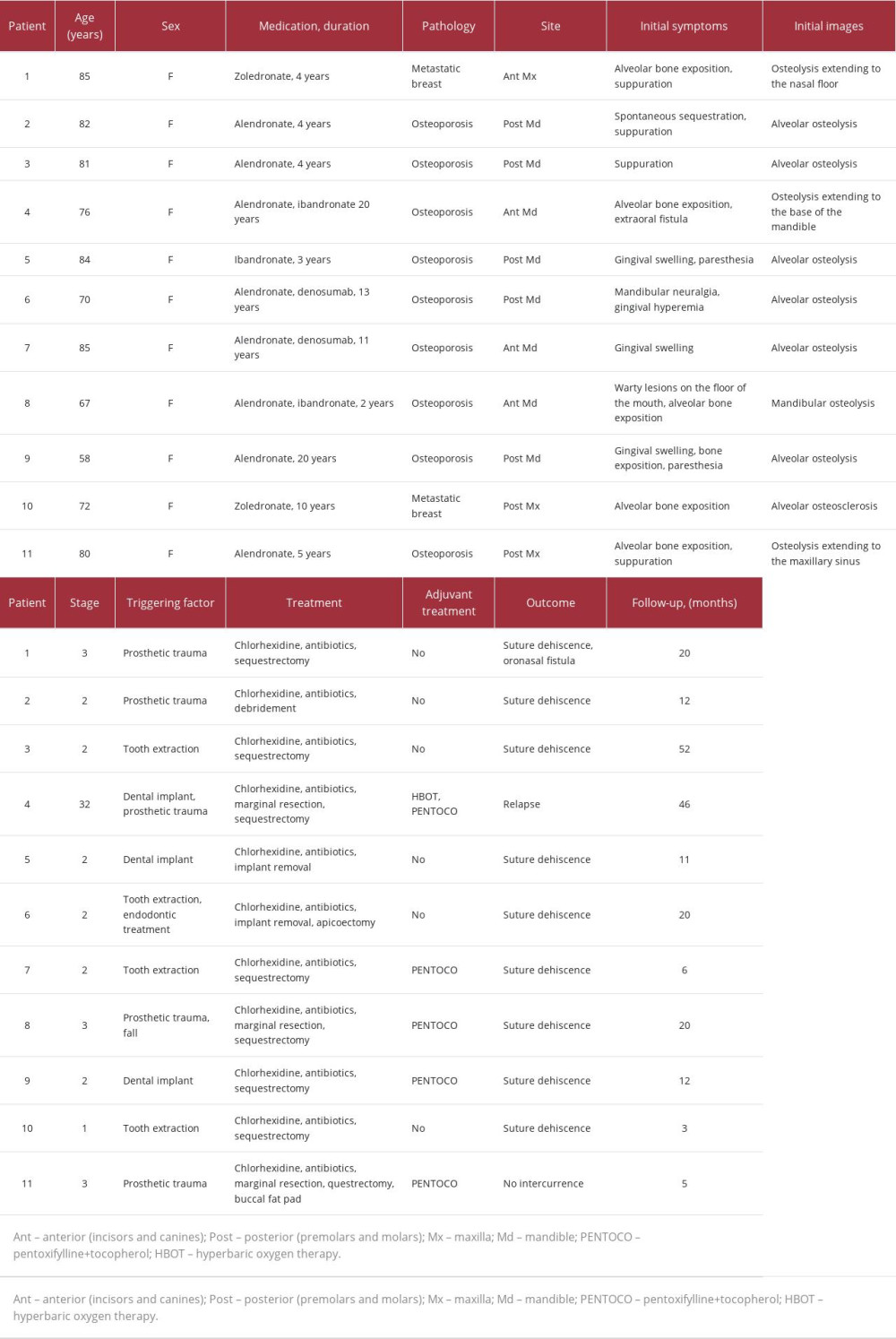 Table 3.. Checklist of the main diagnostic and therapeutic procedures used to treat medication-related osteonecrosis of the jaw.
Table 3.. Checklist of the main diagnostic and therapeutic procedures used to treat medication-related osteonecrosis of the jaw.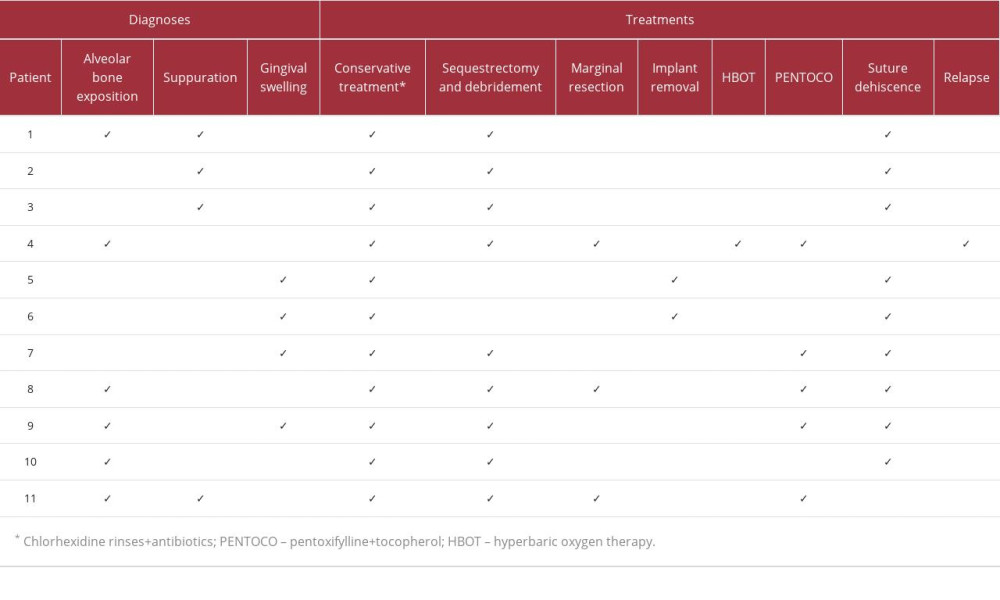
References:
1.. Marx RE, Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws. A growing epidemic: J Oral Maxillofac Surg, 2003; 61(9); 1115-18
2.. Ruggiero SL, Dodson TB, Fantasia J, American association of oral and maxillofacial surgeons position paper on medication-related osteonecrosis of the jaw – 2014 update: J Oral Maxillofac Surg, 2014; 72; 1938-56
3.. Ruggiero SL, Dodson TB, Aghaloo T, American Association of Oral and Maxillofacial Surgeons’ position paper on medication-related osteonecrosis of the jaws – 2022 update: J Oral Maxillofac Surg, 2022; 80(5); 920-43
4.. Ayub N, Faraj M, Ghatan S, The treatment gap in osteoporosis: J Clin Med, 2021; 10(13); 1-13
5.. Badr M, Kyriakidou E, Atkins A, Harrison S, Aggressive denosumab-related jaw necrosis – a case series: Br Dent J, 2017; 223(1); 13-16
6.. Hinson AM, Siegel ER, Stack BC, Temporal correlation between bisphosphonate termination and symptom resolution in osteonecrosis of the jaw: A pooled case report analysis: J Oral Maxillofac Surg, 2015; 73; 53-62
7.. Caldroney S, Ghazali N, Dyalram D, Lubek JE, Surgical resection and vascularized bone reconstruction in advanced stage medication-related osteo-necrosis of the jaw: Int J Oral Maxillofac Surg, 2017; 46; 871-76
8.. Fedele S, Porter SR, D’Aiuto F, Nonexposed variant of bisphosphonate-associated osteonecrosis of the jaw: A case series: Am J Med, 2010; 123(11); 1060-64
9.. Hallmer F, Andersson G, Götrick B, Prevalence, initiating factor, and treatment outcome of medication-related osteonecrosis of the jaw – a 4-year prospective study: Oral Surg Oral Med Oral Pathol Oral Radiol, 2018; 126(6); 477-85
10.. Beth-Tasdogan NH, Mayer B, Hussein H, Interventions for managing medication-related osteonecrosis of the jaw: Cochrane Database Syst Rev, 2017; 10(10); CD012432
11.. Heifetz-Li JJ, Abdelsamie S, Campbell CB, Systematic review of the use of pentoxifylline and tocopherol for the treatment of medication-related osteonecrosis of the jaw: Oral Surg Oral Med Oral Pathol Oral Radiol, 2019; 128(5); 491-97
12.. Mirelli C, Marino S, Bovio A, Medication-related osteonecrosis of the jaw in dental practice: A retrospective analysis of data from the Milan cohort: Dent J, 2022; 10(5); 1-16
13.. Dodson TB, The frequency of medication-related osteonecrosis of the jaw and its associated risk factors: Oral Maxillofac Surg Clin North Am, 2015; 27(4); 509-16
14.. Watts NB, Grbic JT, Binkley N, Invasive oral procedures and events in postmenopausal women with osteoporosis treated with denosumab for up to 10 years: J Clin Endocrinol Metab, 2019; 104(6); 2443-52
15.. Duarte LFM, Alonso K, Basso EC, Dib LL, Surgical treatment of bisphospho-nate-related osteonecrosis of the jaws with the use of buccal fat pad: Case report: Braz Dent J, 2015; 26(3); 317-20
16.. Epstein MS, Wicknick FW, Epstein JB, Berenson JR, Gorsky M, Management of bisphosphonate-associated osteonecrosis: pentoxifylline and tocopherol in addition to antimicrobial therapy. An initial case series: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2010; 110(5); 593-6
17.. Pardo-Zamora G, Martínez Y, Moreno JA, Ortiz-Ruíz AJ, Treatment of stage 2 medication-induced osteonecrosis of the jaw: A case series: Int J Environ Res Public Health, 2021; 18(3); 1-18
18.. Almeida MVC, Moura AC, Santos L, Photodynamic therapy as an adjunct in the treatment of medication-related osteonecrosis of the jaw: A case report: J Lasers Med Sci, 2021; 12; e12
19.. Butera A, Pascadopoli M, Pellegrini M, Oral microbiota in patients with peri-implant disease: A narrative review: Applied Sci, 2022; 12(7); 3250
20.. Vale GC, Mayer MPA: Arch Oral Biol, 2021; 128; 105174
21.. Butera A, Maiorani C, Gallo S, Evaluation of adjuvant systems in non-surgical peri-implant treatment: A literature review: Healthcare, 2022; 10(5); 886
22.. Fernandes TL, Fernades BV, Jitumori C, Franco GCN, A case report of oral bisphosphonate treatment for osteoporosis leading to atypical femoral fracture and pathologic mandibular fracture: Am J Case Rep, 2023; 24; e941144
Figures
Tables
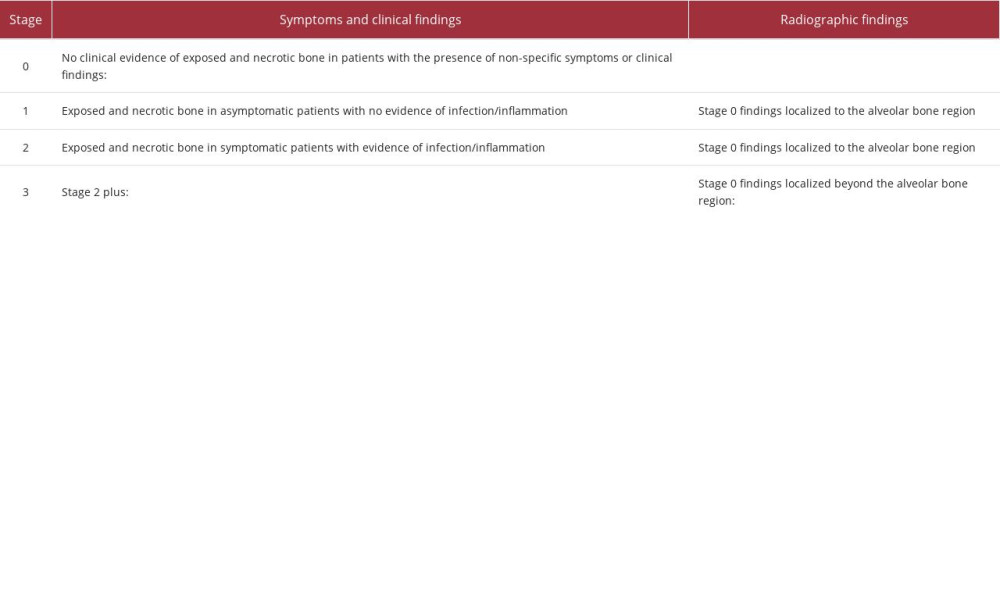 Table 1.. American Association of Oral and Maxillofacial Surgery clinical and radiographic staging system of medication-related osteonecrosis of the jaw.
Table 1.. American Association of Oral and Maxillofacial Surgery clinical and radiographic staging system of medication-related osteonecrosis of the jaw.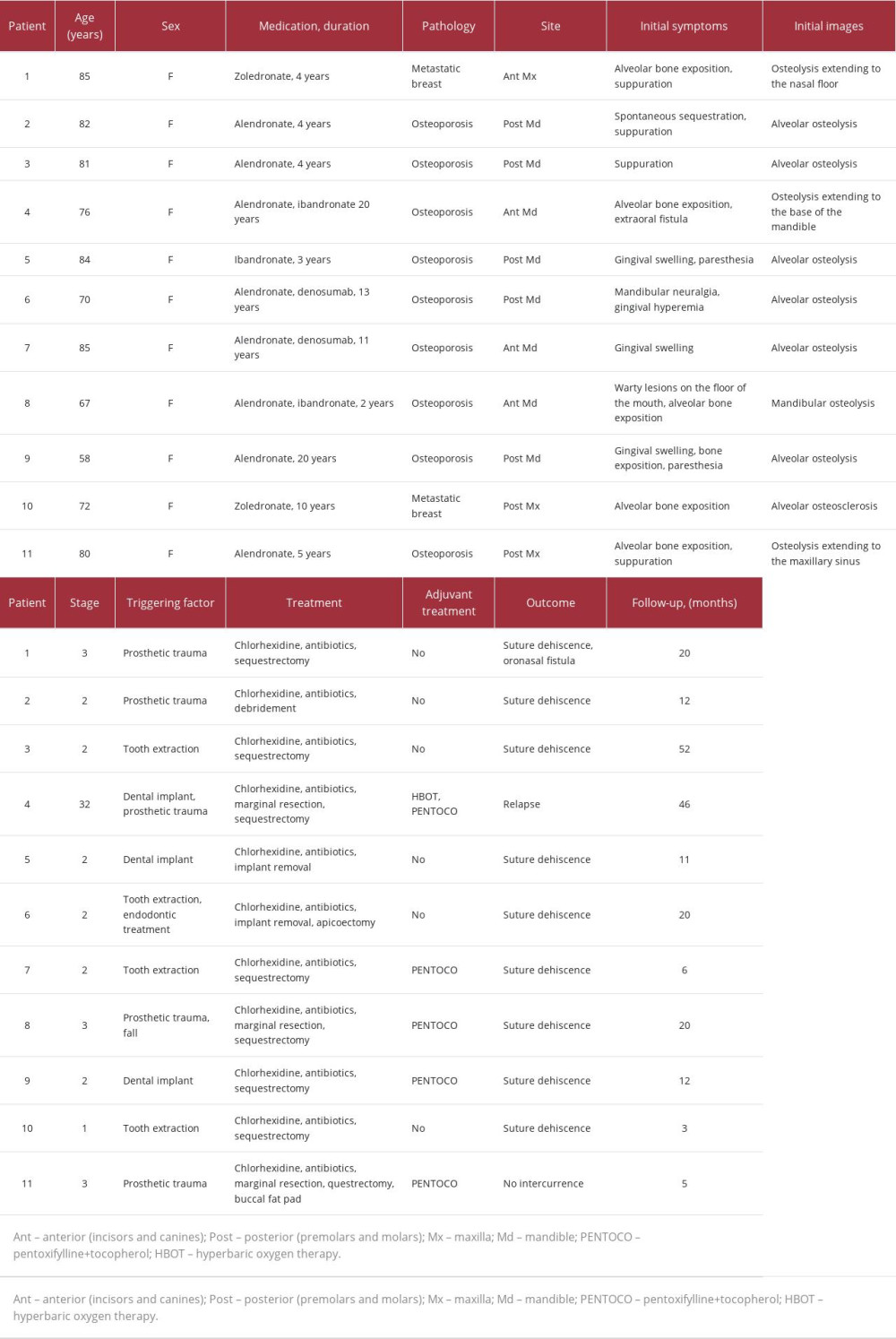 Table 2.. Patients treated for medication-related osteonecrosis of the jaws.
Table 2.. Patients treated for medication-related osteonecrosis of the jaws.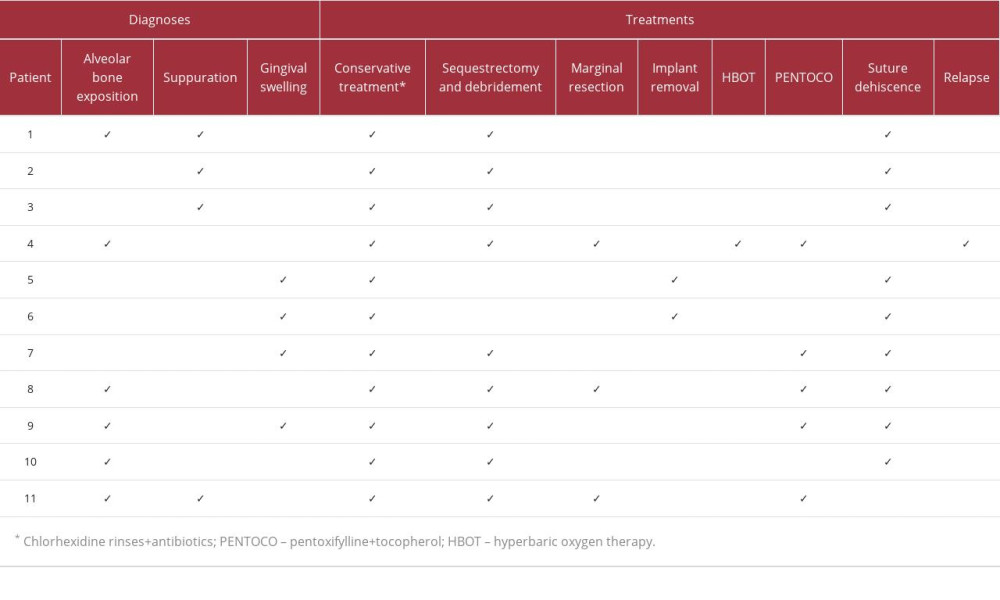 Table 3.. Checklist of the main diagnostic and therapeutic procedures used to treat medication-related osteonecrosis of the jaw.
Table 3.. Checklist of the main diagnostic and therapeutic procedures used to treat medication-related osteonecrosis of the jaw.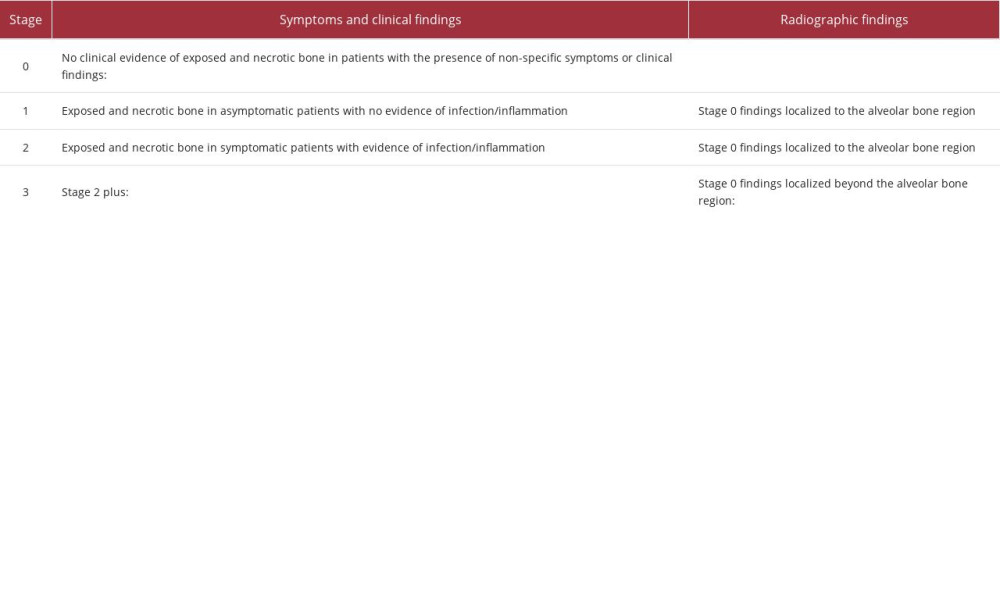 Table 1.. American Association of Oral and Maxillofacial Surgery clinical and radiographic staging system of medication-related osteonecrosis of the jaw.
Table 1.. American Association of Oral and Maxillofacial Surgery clinical and radiographic staging system of medication-related osteonecrosis of the jaw.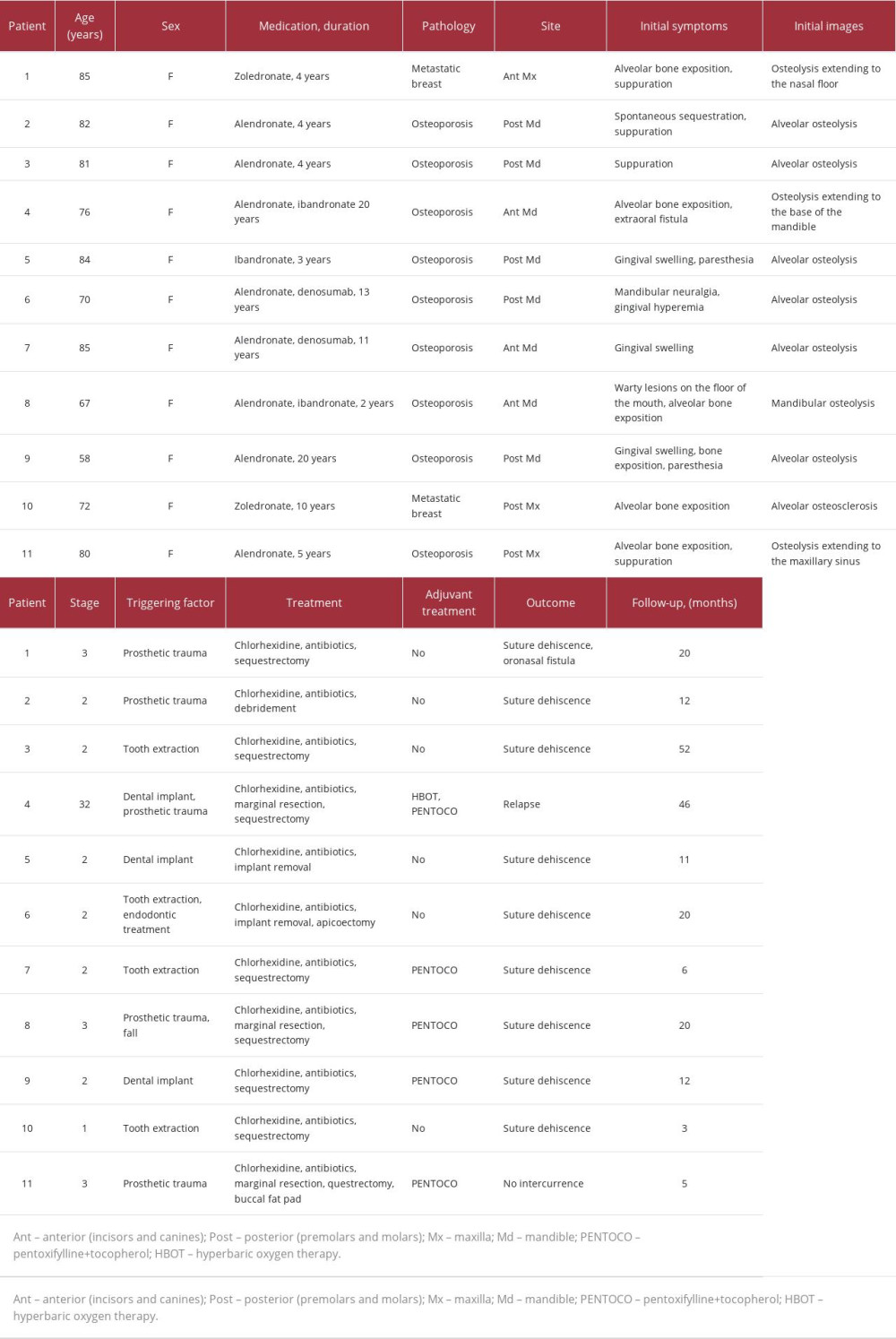 Table 2.. Patients treated for medication-related osteonecrosis of the jaws.
Table 2.. Patients treated for medication-related osteonecrosis of the jaws.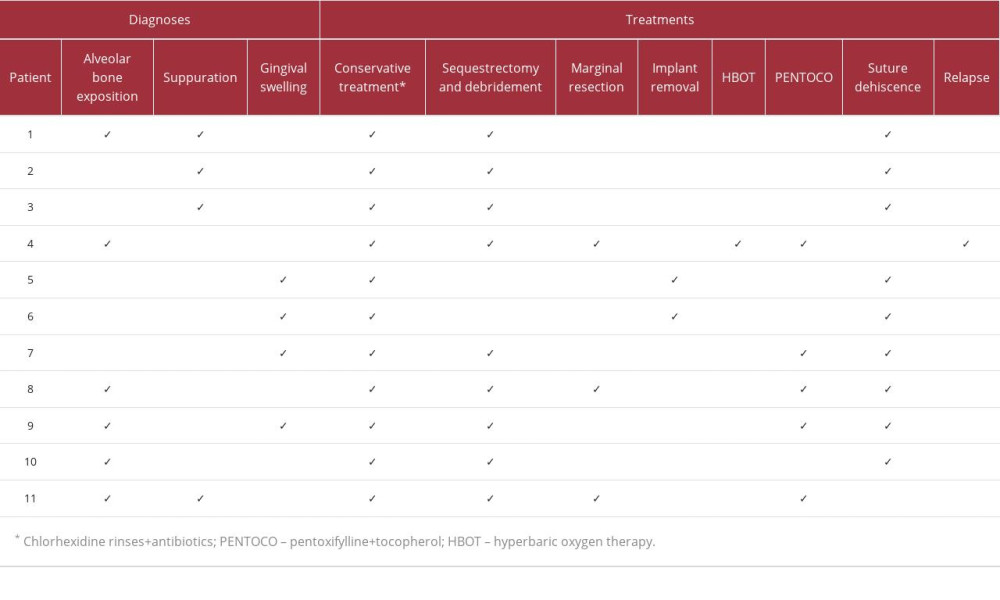 Table 3.. Checklist of the main diagnostic and therapeutic procedures used to treat medication-related osteonecrosis of the jaw.
Table 3.. Checklist of the main diagnostic and therapeutic procedures used to treat medication-related osteonecrosis of the jaw. In Press
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943070
17 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943370
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943803
18 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943467
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250








