05 May 2024: Articles 
Bilateral Simultaneous Basal Ganglia Hemorrhage: A Case Report
Unusual clinical course, Unusual setting of medical care
Jingcheng JiangDOI: 10.12659/AJCR.943174
Am J Case Rep 2024; 25:e943174
Abstract
BACKGROUND: Simultaneous bilateral basal ganglia hemorrhage is an infrequent occurrence in medical literature. The etiology of bilateral basal ganglia intracerebral hemorrhage remains elusive, in contrast to that of unilateral basal ganglia hypertensive intracerebral hemorrhage, resulting in lack of consensus among scholars. Importantly, patients with uremia and cerebral hemorrhage, especially patients with large hematoma volumes, exhibit a markedly elevated mortality rate. Patients can benefit from implementation of positive and efficacious therapeutic approaches.
CASE REPORT: We present a clinical case involving a 42-year-old male patient who was admitted to the hospital in a comatose state. The initial head computed tomography scan revealed the presence of simultaneous basal ganglia hemorrhage; this phenomenon could potentially be attributed to the occurrence of cerebral hemorrhage induced by severe renal hypertension in individuals with uremia. The patient underwent emergency surgical intervention to evacuate the hematoma, followed by continuous blood purification treatment. Ultimately, these interventions have the potential to improve patient outcomes.
CONCLUSIONS: Incidence of bilateral basal ganglia hemorrhage is exceptionally rare and associated with an unfavorable prognosis, often resulting in mortality among individuals with severe underlying conditions or complications. The hematoma was successfully eliminated through the use of skull resection and neuroendoscopy techniques, resulting in favorable outcomes. The implementation of bedside continuous hemodialysis in patients with uremic cerebral hemorrhage can enhance therapeutic efficacy, thus warranting its recommendation for similar cases. Based on our observations, it is plausible that severe hypertension plays a contributory role in the development of simultaneous bilateral basal ganglia bleeding.
Keywords: Neurosurgery, Uremia, essential hypertension, Basal Ganglia Hemorrhage
Introduction
Simultaneous bilateral basal ganglia hemorrhage is a rare phenomenon, accounting for approximately 0.3% of cases of spontaneous hemorrhage [1]. The underlying cause of bilateral basal ganglia intracerebral hemorrhage remains unknown, unlike that of unilateral basal ganglia hypertensive intracerebral hemorrhage, leading to a lack of agreement among scholars. It is worth mentioning that patients with uremia and cerebral hemorrhage, especially those with extensive bleeding, experience a significantly higher mortality rate. To the best of our knowledge, there have been no documented instances of successful treatment for patients with uremia presenting with simultaneous bilateral basal ganglia bleeding.
Case Report
On July 21, 2023, a middle-aged male patient was brought to the hospital by his family following a loss of consciousness. Upon assessment, the patient exhibited a Glasgow coma scale (GCS) score of 6 points (E1V1M4), signifying a lack of response to external stimuli. Additionally, the patient presented with bilateral pupils measuring 0.3 cm in diameter, with no reactivity to light. Furthermore, asymmetry in facial features was noted, with a shallow left nasolabial sulcus, and the left limb demonstrated painful stimulation without resultant movement. The initial National Institutes of Health Stroke Scale (NIHSS) score was recorded as 29 points. The patient had a history of hypertension spanning 7 years. Physicians advocate the use of nifedipine sustained-release tablets and terazosin for the management of blood pressure in patients. The doctor advocated the use of nifedipine sustained-release tablets and terazosin to control the patient’s blood pressure, and the patient adopted this treatment plan for treatment. Unfortunately, the patient’s blood pressure was not adequately monitored, resulting in sustained systolic blood pressure levels exceeding 200 mmHg. Urapidil via intravenous injection was administered as an emergency measure to regulate blood pressure subsequent to hospital admission. Furthermore, the patient experienced the onset of uremia 2 years prior. He opted against heparin anticoagulation and instead adopted a sodium citrate anticoagulation regimen for his hemodialysis therapy. The admission blood test results revealed a creatinine level of 982 μmol/L.
The cranial computed tomography scan conducted in response to the patient’s emergency situation revealed bilateral simultaneous basal ganglia hemorrhage. Using the Coniglobus formula, the calculated volume of bleeding in the right basal ganglia amounted to 40 mL, while the left basal ganglia exhibited a bleeding volume of 5 mL (Figure 1A). As outlined in the Chinese Guidelines for the Diagnosis and Treatment of Cerebral Hemorrhage (2019) [2], surgical intervention can be warranted in cases of basal ganglia hemorrhage ≥30 mL accompanied by coma. After obtaining consent from the patient’s guardian, a craniotomy was conducted, using the right pterion approach. To aid in the evacuation of the hematoma, neuroendoscopy was used (Figure 1B, 1C). Following the successful removal of the hematoma, the cerebral tissue exhibited elevated tension, necessitating the implementation of a decompression craniectomy. The range of skull resection was approximately 8×10 cm. Intracranial pressure monitoring was not conducted, as a result of financial constraints experienced by the patient.
The patient demonstrated an improvement in his level of consciousness on the second day after surgery, as evidenced by a GCS score of 10 (E2V3M5). Subsequent to the surgical procedure, continuous bedside hemodialysis was administered. Following a duration of 2 weeks of uninterrupted treatment, the treatment modality shifted to intermittent hemodialysis, with the procedure conducted thrice weekly. Additionally, the patient developed pseudobulbar paralysis, necessitating the insertion of a gastric tube. After a 3-week hospitalization, the patient demonstrated improvement in language ability, manifesting the ability to articulate monosyllabic sounds and use simple vocabulary. The patient had differing levels of limb strength, with the right limb at level 5, the left lower limb at level 2, and the left upper limb at level 0. Subsequently, the patient was transferred to a rehabilitation center for further training. At a 3-month follow-up, the patient’s language ability had fully recovered, albeit with a decrease in responsiveness. The symptoms of pseudobulbar paralysis had alleviated, enabling the patient to ingest food. The patient exhibited muscle strength levels of 2 in the left upper limb, 4 in the left lower limb, and normal strength in the right limb. The subsequent NIHSS score obtained during the retest was documented as 13 points. The blood test results indicated a creatinine level of 892.3 μmol/L.
Discussion
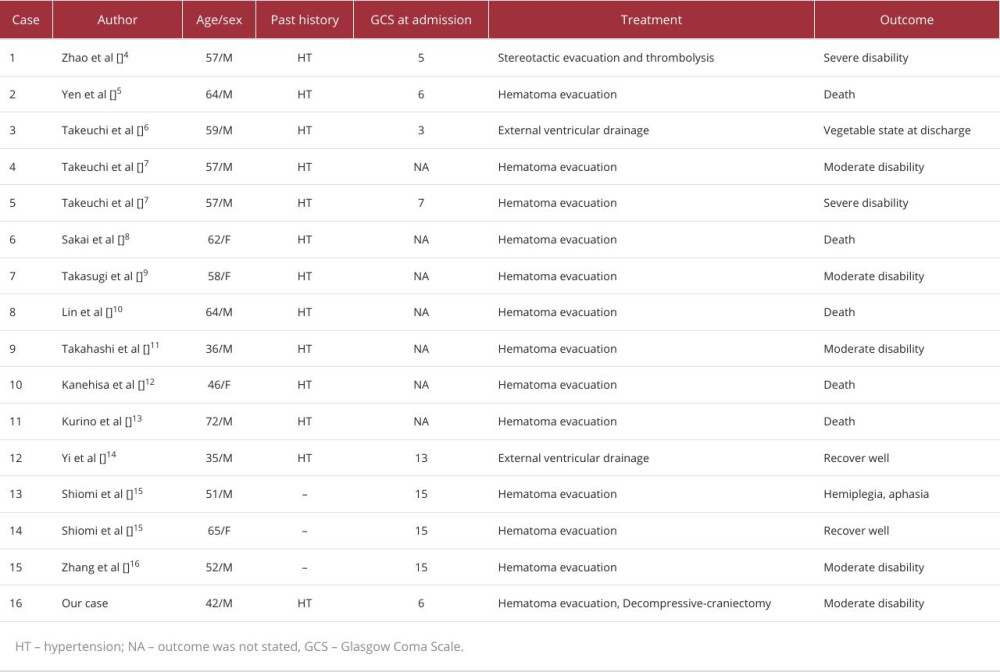
Basal ganglia hemorrhage, a prevalent form of hypertensive intracerebral hemorrhage, typically manifests unilaterally. Simultaneous bilateral basal ganglia hemorrhage is a rare occurrence. The latter, however, exhibits a higher propensity for severe complications, such as pulmonary infection, deep vein thrombosis, and pseudobulbar paralysis. We reviewed the literature on co-occurring basal ganglia hemorrhage, and the prognosis was primarily unfavorable [3–16] (Table 1). The efficacy of surgical intervention for bilateral basal ganglia hemorrhage remains a subject of contention. The surgical techniques employed in this study primarily involved neuroendoscopic surgery and puncture drainage surgery, which are associated with reduced trauma. However, the administration of dehydrating drugs after cerebral hemorrhage in the presence of uremia can exacerbate internal environment disorders. Craniotomy was performed to alleviate pressure, while neuroendoscopy-assisted surgery was conducted to extract the hematoma. Compared with microinvasive surgery, this approach effectively alleviates intracranial hypertension and minimizes brain tissue damage. Continuous bedside hemodialysis was used as a strategy to minimize disruptions in the internal electrolyte balance [17].
The precise etiology of bilateral basal ganglia hemorrhage occurring simultaneously remains uncertain. One potential mechanism is the fortuitous simultaneous rupture of bilateral microaneurysms on lenticulostriate arteries. Alternatively, a more compelling explanation is that the initial hemorrhage leads to specific hemodynamic circumstances, such as a reflexive elevation in blood pressure, which triggers the rupture of a second microaneurysm on the contralateral side within a brief timeframe [3,4].
Conclusions
The incidence of bilateral basal ganglia hemorrhage is exceptionally rare and is associated with an unfavorable prognosis, often resulting in mortality among individuals with severe underlying conditions or complications. Remarkably, our case represents the initial documented instance of a successful surgical intervention for bilateral basal ganglia hemorrhage in a patient with uremia. The use of craniotomy and neuroendoscopic techniques presents a potentially superior alternative for patients in achieving effective hematoma eradication. The implementation of bedside continuous hemodialysis in patients with uremic cerebral hemorrhage has enhanced therapeutic efficacy, thus warranting its recommendation for similar cases. Based on our observations, it is plausible that severe hypertension plays a contributory role in the development of simultaneous bilateral basal ganglia bleeding [18].
References:
1.. Silliman S, McGill J, Booth R, Simultaneous bilateral hypertensive putaminal hemorrhages: J Stroke Cerebrovasc Dis, 2003; 12(1); 44-46
2.. Zhu S, Lian L, Zhang S, Chinese guidelines for diagnosis and treatment of acute intracerebral hemorrhage 2019: Chin J Neurol, 2019; 52(12); 994-1005
3.. Yang Z, Chen J, Mu J, Simultaneous bilateral basal ganglia hemorrhage: Curr Drug Deliv, 2017; 14(6); 807-15
4.. Zhao J, Chen Z, Wang Z, Simultaneous bilateral hypertensive basal ganglia hemorrhage: Neurol Neurochir Pol, 2016; 50(4); 275-79
5.. Yen CP, Lin CL, Kwan AL, Simultaneous multiple hypertensive intracerebral haemorrhages: Acta Neurochir (Wien), 2005; 147(4); 393-99 ; discussion 399
6.. Takeuchi S, Takasato Y, Masaoka H, Bilateral lenticulostriate artery aneurysms: Br J Neurosurg, 2009; 23(5); 543-44
7.. Takeuchi S, Takasato Y, Masaoka H, Simultaneous multiple hypertensive intracranial hemorrhages: J Clin Neurosci, 2011; 18(9); 1215-18
8.. Sakai T, Yokota H, Kokashi M, [A case of bilateral hypertensive intra-cerebral hemorrhage.]: 7th Annual Meeting Program of Japanese Society of Cerebral Apoplexy, 1982; 166 [in Japanese]
9.. Takasugi N, Nakajima H, Norikane H, [Simultaneous bilateral hypertensive intracerebral hematomas]: Med J Kagawa Pref Central Hosp, 1984; 3; 119-22 [in Japanese]
10.. Lin CN, Howng SL, Kwan AL, Bilateral simultaneous hypertensive intracerebral hemorrhages: Gaoxiong Yi Xue Ke Xue Za Zhi, 1993; 9(5); 266-75
11.. Takahashi T, Kajikawa H, Fujii S, Multiple Hypertensive brain hemorrhages with simultaneous occurrence – report of four cases: J Hiroshima Medical Association, 1994; 47; 623-28
12.. Kanehisa Y, Three cases with multiple intracerebral hemorrhage occurring simultaneously: Naika (Internal Medicine), 1994; 73; 185-89
13.. Kurino M, Ichimura H, Koga K, Two cases of simultaneous bilateral hypertensive intracerebral hemorrhage: Medical J Oita Prefectural Hospital, 2000; 29; 141-44
14.. Yi HJ, Shin IY, Hwang HS, Simultaneous multiple basal ganglia and cerebellar hemorrhage: Case report: J Cerebrovasc Endovasc Neurosurg, 2013; 15(4); 316-19
15.. Shiomi N, Miyagi T, Koga S, [Simultaneous multiple hypertensive intracerebral hematoma]: No Shinkei Geka, 2004; 32(3); 237-44 [in Japanese]
16.. Zhang DY, Li SS, Liang J, Hypertensive symmetrical cerebral hemorrhage in bilateral basal ganglia: A case report: J Int Neurol Neurosurg, 2019; 46(3); 305-6
17.. Magnani S, Atti M, Uremic toxins and blood purification: A review of current evidence and future perspectives: Toxins (Basel), 2021; 13(4); 246
18.. Sheikh Hassan M, Mohamed Ali A, Farah Osman M, Spontaneous bilateral basal ganglia hemorrhage due to severe hypertension: Vasc Health Risk Manag, 2022; 18; 473-77
In Press
02 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942681
03 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943597
03 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943392
04 Apr 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943271
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250