12 August 2020: Articles 
Atypical Reactivation of Varicella Zoster Virus Associated with Pancreatitis in a Heart Transplant Patient
Unusual clinical course, Challenging differential diagnosis, Educational Purpose (only if useful for a systematic review or synthesis)
Christine Shieh1BCDEF*, Ashley Barnes1BD, Drew M. Johnson2B, Ilya M. Danelich3BE, Preethi Pirlamarla2B, Rene Alvarez2B, Howard Massey4B, Mahek Shah2ABCDEDOI: 10.12659/AJCR.923969
Am J Case Rep 2020; 21:e923969
Abstract
BACKGROUND: Acute pancreatitis is rare following solid organ transplantation but is associated with high mortality. It has been most commonly reported following renal transplant but can occur with other solid organ transplantations.
CASE REPORT: A 46-year-old male who had an orthotopic heart transplant 6 months ago presented with a 3-week history of abdominal pain. The patient described it as intermittent, sharp, and stabbing, originating in the periumbilical area and radiating to the back. His lipase was elevated at 232 U/L. Given that the patient’s symptoms and lipase were elevated to greater than three times the upper limit of normal, he patient was diagnosed with acute pancreatitis. The patient also mentioned a diffuse itchy rash that started a few days prior to admission. Dermatology was consulted, and given the man’s clinical presentation, there was concern for atypical reactivation of varicella zoster virus (VZV). VZV polymerase chain reaction of the vesicles returned positive. The patient was started on acyclovir and his symptoms improved.
CONCLUSIONS: This is the first reported case of VZV-associated pancreatitis in a heart transplant patient. Our patient presented with acute pancreatitis and was treated supportively. However, he did not receive antiviral treatment until his rash was discovered. Timely treatment of VZV resulted in resolution of both the rash and pancreatitis. Timely diagnosis of pancreatitis and VZV is important to prevent development of multiorgan failure and death.
Keywords: Abdominal Pain, Heart Transplantation, Herpesvirus 3, Human, Immunosuppression, latent infection, transplant recipients, Varicella Zoster Virus Infection, Virus Activation
Background
Acute pancreatitis is rare following solid organ transplantation but is associated with high mortality [1]. It has most commonly been reported following renal transplant, with an incidence ranging from 2% to 7% and a 50% to 100% mortality rate [2]. Acute pancreatitis is known to occur after heart transplantation, especially in the early postoperative period [3]. Given the high morbidity and mortality associated with such cases, early recognition and identification of a reversible etiology remains key. Common etiologies of pancreatitis in immunocompetent patients include gallstones, alcohol use, and medications. Among solid organ transplant recipients who are immunosuppressed, specific etiologies such as steroid use, azathioprine, and cytomegalovirus (CMV) reactivation have also been reported [1]. While only a few cases of pancreatitis in renal transplant patients have been attributed to VZV, some patients became critically ill and died from disseminated disease [4]. Here, we present the first reported case of acute pancreatitis associated with atypical reactivation of VZV presenting as a varicella-like rash in a heart transplant recipient.
Case Report
A 46-year-old male with a history of non-ischemic dilated cardiomyopathy who had an orthotopic heart transplant 6 months prior presented with a 3- week history of abdominal pain. The patient thought the pain was from lifting, but it had gotten progressively worse over the last few days. Other medical history included chronic obstructive pulmonary disorder, pulmonary sarcoidosis, hypertension, and diabetes. At the time of presentation, the patient was on triple immunosuppression with mycophenolate mofetil, tacrolimus, and prednisone.
The patient described his abdominal pain as intermittent, sharp, and stabbing, originating in the periumbilical area and radiating to the back. Associated symptoms included decreased oral intake, nausea, and vomiting. Work-up in the emergency department 3 days prior for mild abdominal pain included a computed tomography scan of the abdomen, which revealed no evidence of pancreatitis, cholecystitis, colitis, hydronephrosis, or gallstones. During the patient’s current hospitalization, his blood alcohol and triglyceride levels were within normal limits. His blood lipase was elevated at 232 U/L, uptrending from 130 U/L 3 days previously. Given the patient’s symptoms and lipase being elevated to greater than three times the upper limit of normal, he was diagnosed with acute pancreatitis.
The patient was admitted to the inpatient service and was in mild-moderate distress from the abdominal pain. He was started on supportive care for acute pancreatitis with intravenous fluids and opioids for pain control. An abdominal ultra-sound showed no evidence of gall stones, or gallbladder wall thickening. The etiology of the pancreatitis remained unclear. The patient’s steroid dose was halved and atorvastatin was discontinued in case it was contributory.
The patient mentioned an itchy rash over his body that started a few days prior to admission and had progressed since. The rash was noted to be vesicular, erythematous, diffuse on his neck, back, and groin, and present on both sides of the midline (Figure 1A). He denied sick contacts and reported a remote history of chicken pox. A review of previous records demonstrated presence of pre-transplant immunoglobulin G (IgG) varicella zoster virus (VZV) antibodies. Dermatology was consulted and described the lesions as vesicles on an erythematous base with no dermatomal distribution (Figure 1B). Given that the lesions were in multiple stages of development, there was concern for atypical reactivation of VZV that appeared more like varicella than herpes zoster in the setting of immunosuppression. The vesicles were swabbed for VZV polymerase chain reaction (PCR testing), which returned positive. A Tzanck smear showed giant multinucleated keratinocytes, confirming the PCR findings. VZV PCR and both VZV immunoglobulin M (IgM) and IgG antibodies tested positive in blood. CMV and herpes simplex virus PCR were negative.
The patient was started on acyclovir 10 mg/kg q8h for 7 to 10 days and placed on airborne precaution within hours of suspicion for disseminated VZV. His symptoms improved with continued supportive care for pancreatitis. After the lesions crusted over, the patient was transitioned to oral valacyclovir to complete a 10-day course. He was discharged and followed up in transplant clinic, where the symptoms had completely resolved and lipase levels were back within normal limits (31 U/L). He continues to have an uneventful post-transplant course.
Discussion
To our knowledge, this is the first reported case of VZV-associated pancreatitis in a heart transplant patient. Our patient presented with a subtle rash that appeared more like VCV than HZV despite the prior history of chickenpox. Incidence of pancreatitis among heart transplant recipients can range from 2% to 18%, significantly higher than for other cardiac procedures [5]. However, the diagnosis may be delayed due to subtler clinical presentations and the potentially large differential diagnoses for abdominal pain post solid organ transplant. While gallstones and alcohol intake are the most common causes, other etiologies in immunocompromised patients, such as drugs or opportunistic infections, must be entertained.
Our patient met the Atlanta criteria for pancreatitis based on his lipase level and clinical presentation although his imaging was negative. Nearly all common etiologies of pancreatitis were ruled out in this patient; however, his symptoms did not begin to resolve until he initiated antiviral treatment for VZV. Although VZV may not be an irrefutable cause of his pancreatitis, the association between VZV and visceral organ involvement in immunosuppressed patients has been documented in the literature and should not be overlooked. In nearly all cases, the presentation of visceral involvement preceded the VZV rash, and a delayed diagnosis of VZV resulted in organ failure and death [6]. A study by Locksley et al. on VZV infection in bone marrow transplant recipients found that 21% had visceral symptoms before skin manifestations [7].
Cases of VZV-induced pancreatitis have been described in immunocompetent patients as well [8].
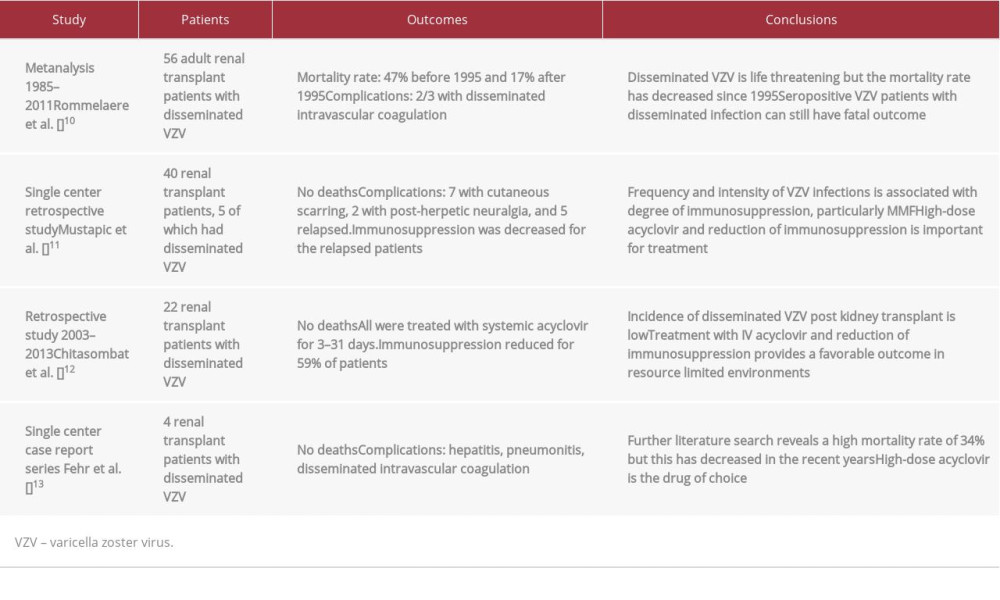
This case and other similar cases presented previously in renal transplant patients (Table 1) reinforce the importance of preventing VZV infection in immunocompromised patients [10–13]. Our patient had prior immunity to varicella, as evidenced by a reactive VZV IgG antibody, but interestingly, presented with what appears to be VZV despite no recent sick contacts with positive IgM and IgG serology. IgM serology can provide evidence for a recent active VZV infection, but does not discriminate between a primary infection and reinfection or reactivation of latent infection due to transient increase in specific IgM antibodies on such re-exposure to VZV. Thus, we hypothesize that our patient likely represents a case of VZV reactivation from previous latency. In general, all potential transplant patients should undergo serologic testing and seronegative patients should be vaccinated prior to the surgery [9]. Those who are not vaccinated and are exposed post-transplant should receive VZV immunoglobulin or acyclovir [9]. Therapy with acyclovir or alternative equivalent antiviral therapies should be initiated within 24 to 72 hours of symptom onset to maximize efficacy.
Conclusions
In summary, timely diagnosis of pancreatitis in the setting of disseminated VZV is important in immunocompromised patients to prevent development of multiorgan failure and death. Identification of the appropriate etiology for pancreatitis in post-transplant patients requires maintaining a high suspicion for alternative diagnosis beyond conventional known risk factors.
References:
1.. Sinha S, Ratan J, Lakhtakia S, Narayan G, Acute pancreatitis following kidney transplantation – role of viral infections: J Clin Translat Res, 2003; 17(1); 32-36
2.. Tabakovic M, Salkic NN, Bosnjic J, Alibegovic E, Acute pancreatitis after kidney transplantation: Case Rep Transplant, 2012; 2012; 768193
3.. Herline AJ, Pinson CW, Wright JK, Acute pancreatitis after cardiac transplantation and other cardiac procedures: Case control analysis in 24,631 patients: Am Surg, 1999; 65(9); 819-25
4.. Chhabra P, Ranjan P, Bhasin DK, Simultaneous occurrence of varicella zoster virus induced pancreatitis and hepatitis in a renal transplant recipient: A case report and review of the literature: Perm J, 2017; 21; 16-083
5.. Lin TW, Tsai MT, Roan JN, Obscured hemorrhagic pancreatitis after orthotopic heart transplantation complicated with acute right heart failure and hepatic dysfunction: a case report: J Cardiothorac Surg, 2016; 11(1); 166
6.. Bookhout C, Molylan V, Thorne LB, Two fatal herpesvirus cases: Treatable but easily missed diagnoses: ID Cases, 2016; 6; 65-67
7.. Locksley RM, Flournoy N, Sullivan KM, Meyers JD, Infection with varicella-zoster virus after marrow transplantation: J Infect Dis, 1985; 152(6); 1172-81
8.. Wang Z, Ye J, Han YH, Acute pancreatitis associated with herpes zoster: Case report and literature review: World J Gastroenterol, 2014; 20(47); 18053-56
9.. Pergam SA, Limaye AP, AST Infectious Diseases Community of Practice: Varicella zoster virus (VZV) in solid organ transplant recipients: Am J Transplant, 2009; 9(S4); S108-15
10.. Rommelaere M, Marechal C, Yombi JC, Disseminated varicella zoster virus infection in adult renal transplant recipients: Outcome and risk factors: Transplant Proc, 2012; 44(9); 2814-17
11.. Mustapic Z, Basic-Jukic N, Kes P, Varicella zoster infection in renal transplant recipients: Prevalence, complications and outcome: Kidney Blood Press Res, 2011; 34; 382-86
12.. Chitasombat MN, Watcharananan SP, Prevalence and outcome of disseminated varicella zoster infection post kidney transplantation: J Med Assoc Thai, 2016; 99(4); 381-85
13.. Fehr T, Bossart W, Wahl C, Binswanger U, Disseminated varicella infection in adult renal allograft recipients: Four cases and a review of the literature: Transplant, 2002; 73(4); 608-11
In Press
04 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.941835
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943042
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.942578
05 Mar 2024 : Case report 
Am J Case Rep In Press; DOI: 10.12659/AJCR.943801
Most Viewed Current Articles
07 Mar 2024 : Case report 
DOI :10.12659/AJCR.943133
Am J Case Rep 2024; 25:e943133
10 Jan 2022 : Case report 
DOI :10.12659/AJCR.935263
Am J Case Rep 2022; 23:e935263
19 Jul 2022 : Case report 
DOI :10.12659/AJCR.936128
Am J Case Rep 2022; 23:e936128
23 Feb 2022 : Case report 
DOI :10.12659/AJCR.935250
Am J Case Rep 2022; 23:e935250